Abstract
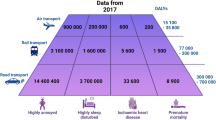
Epidemiological studies have found that transportation noise increases the risk of cardiovascular morbidity and mortality, with high-quality evidence for ischaemic heart disease. According to the WHO, ≥1.6 million healthy life-years are lost annually from traffic-related noise in Western Europe. Traffic noise at night causes fragmentation and shortening of sleep, elevation of stress hormone levels, and increased oxidative stress in the vasculature and the brain. These factors can promote vascular dysfunction, inflammation and hypertension, thereby elevating the risk of cardiovascular disease. In this Review, we focus on the indirect, non-auditory cardiovascular health effects of transportation noise. We provide an updated overview of epidemiological research on the effects of transportation noise on cardiovascular risk factors and disease, discuss the mechanistic insights from the latest clinical and experimental studies, and propose new risk markers to address noise-induced cardiovascular effects in the general population. We also explain, in detail, the potential effects of noise on alterations of gene networks, epigenetic pathways, gut microbiota, circadian rhythm, signal transduction along the neuronal–cardiovascular axis, oxidative stress, inflammation and metabolism. Lastly, we describe current and future noise-mitigation strategies and evaluate the status of the existing evidence on noise as a cardiovascular risk factor.
Key points
-
Noise is associated with cardiovascular diseases, such as arterial hypertension, coronary artery disease, heart failure and arrhythmia, and should therefore be considered a cardiovascular risk factor.
-
Noise-induced stress increases blood pressure, stress hormone levels, endothelial dysfunction, oxidative stress, NADPH oxidase 2 (NOX2) activity, nitric oxide synthase uncoupling and vascular inflammation in mice, all of which are prevented by NOX2 deficiency.
-
Translational field studies in healthy individuals and patients with heart disease established that short-term simulated aircraft and railway noise impairs sleep quality and increases stress hormone levels, blood pressure, endothelial dysfunction and oxidative stress.
-
The quality of evidence on the adverse cardiovascular effects of noise exposure has increased for several cardiometabolic risk factors since the WHO evaluation in 2018, especially for obesity and diabetes mellitus.
-
Noise-induced stress increases cerebral oxidative stress and downregulates and uncouples neuronal nitric oxide synthase, providing a potential explanation for the observed retardation in the development of cognitive function (memory and learning) in children exposed to aircraft noise.
-
Mitigation strategies to reduce population exposure to transportation noise are available and need to be implemented.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 1907–1918 (2017).
World Health Organization. Environmental Noise Guidelines for the European Region http://www.euro.who.int/en/publications/abstracts/environmental-noise-guidelines-for-the-european-region-2018 (2018).
GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422 (2017).
OECD/EU. Health at a Glance: Europe 2018: State of Health in the EU Cycle (OECD Publishing, 2018).
Piepoli, M. F. et al. 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 37, 2315–2381 (2016).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart association task force on clinical practice guidelines. Circulation 140, e596–e646 (2019).
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2224–2260 (2012).
WHO. Projections of mortality and causes of death, 2016 to 2060 https://www.who.int/healthinfo/global_burden_disease/projections/en/ (2021).
WHO. The Global Health Observatory https://www.who.int/data/gho/data/themes/noncommunicable-diseases (2021).
Landrigan, P. J. et al. The lancet commission on pollution and health. Lancet 391, 462–512 (2018).
Lelieveld, J. et al. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur. Heart J. 40, 1590–1596 (2019).
Burnett, R. et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl Acad. Sci. USA 115, 9592–9597 (2018).
Wild, C. P. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomarkers Prev. 14, 1847–1850 (2005).
Münzel, T. et al. The adverse effects of environmental noise exposure on oxidative stress and cardiovascular risk. Antioxid. Redox Signal. 28, 873–908 (2018).
Kryter, K. D. Effects of Noise on Man. 1st edn (Academic Press, 1970).
Peterson, E. A., Augenstein, J. S., Tanis, D. C. & Augenstein, D. G. Noise raises blood pressure without impairing auditory sensitivity. Science 211, 1450–1452 (1981).
European Environment Agency. Environmental noise in Europe https://www.eea.europa.eu/publications/environmental-noise-in-europe (2020).
Babisch, W., Gallacher, J. E., Elwood, P. C. & Ising, H. Traffic noise and cardiovascular risk. The Caerphilly study, first phase. Outdoor noise levels and risk factors. Arch. Env. Health 43, 407–414 (1988).
Babisch, W. Updated exposure-response relationship between road traffic noise and coronary heart diseases: a meta-analysis. Noise Health 16, 1–9 (2014).
Vienneau, D., Schindler, C., Perez, L., Probst-Hensch, N. & Röösli, M. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ. Res. 138, 372–380 (2015).
Kempen, E. V., Casas, M., Pershagen, G. & Foraster, M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int. J. Environ. Res. Public Health 15, 379 (2018).
Monrad, M. et al. Residential exposure to traffic noise and risk of incident atrial fibrillation: A cohort study. Env. Int. 92-93, 457–463 (2016).
Héritier, H. et al. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur. J. Epidemiol. 32, 307–315 (2017).
Seidler, A. et al. Myocardial infarction risk due to aircraft, road, and rail traffic noise. Dtsch. Arztebl Int. 113, 407–414 (2016).
van Kamp, I., Simon, S., Notley, H., Baliatsas, C. & van Kempen, E. Evidence relating to environmental noise exposure and annoyance, sleep disturbance, cardio-vascular and metabolic health outcomes in the context of IGCB (N): a scoping review of new evidence. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17093016 (2020).
Sorensen, M. et al. Road traffic noise and stroke: a prospective cohort study. Eur. Heart J. 32, 737–744 (2011).
Beelen, R. et al. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup. Env. Med. 66, 243–250 (2009).
Huss, A., Spoerri, A., Egger, M. & Röösli, M. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology 21, 829–836 (2010).
Seidler, A. L. et al. The effect of aircraft, road, and railway traffic noise on stroke - results of a case-control study based on secondary data. Noise Health 20, 152–161 (2018).
Halonen, J. I. et al. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur. Heart J. 36, 2653–2661 (2015).
Pyko, A. et al. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup. Environ. Med. 76, 201–207 (2019).
Cai, Y. et al. Road traffic noise, air pollution and incident cardiovascular disease: A joint analysis of the HUNT, EPIC-Oxford and UK Biobank cohorts. Env. Int. 114, 191–201 (2018).
Sorensen, M. et al. Long-term exposure to road traffic noise and nitrogen dioxide and risk of heart failure: a cohort study. Environ. Health Perspect. 125, 097021 (2017).
Seidler, A. et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease-A case-control study based on secondary data. Int. J. Hyg. Environ. Health https://doi.org/10.1016/j.ijheh.2016.09.012 (2016).
Carey, I. M. et al. Traffic pollution and the incidence of cardiorespiratory outcomes in an adult cohort in London. Occup. Env. Med. 73, 849–856 (2016).
Dimakopoulou, K. et al. Is aircraft noise exposure associated with cardiovascular disease and hypertension? Results from a cohort study in Athens, Greece. Occup. Environ. Med. 74, 830–837 (2017).
Basner, M. et al. Auditory and non-auditory effects of noise on health. Lancet 383, 1325–1332 (2014).
Schmidt, F. P. et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur. Heart J. 34, 3508–3514a (2013).
Basner, M. & McGuire, S. WHO environmental noise guidelines for the european region: a systematic review on environmental noise and effects on sleep. Int. Environ. Res. Public Health 15, 519 (2018).
Roswall, N. et al. Nighttime road traffic noise exposure at the least and most exposed facades and sleep medication prescription redemption - a Danish cohort study. Sleep 43, zsaa029 (2020).
Beutel, M. E. et al. Noise annoyance predicts symptoms of depression, anxiety and sleep disturbance 5 years later. Findings from the Gutenberg Health Study. Eur. J. Public. Health 30, 516–521 (2020).
Fuks, K. B. et al. Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur. Heart J. 38, 983–990 (2017).
Thacher, J. D. et al. Road traffic noise exposure and filled prescriptions for antihypertensive medication: a danish cohort study. Env. Health Perspect. 128, 57004 (2020).
Zeeb, H. et al. Traffic noise and hypertension - results from a large case-control study. Env. Res. 157, 110–117 (2017).
Pyko, A. et al. Transportation noise and incidence of hypertension. Int. J. Hyg. Env. Health 221, 1133–1141 (2018).
McHill, A. W. & Wright, K. P. Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes. Rev. 18 (Suppl. 1), 15–24 (2017).
Cappuccio, F. P., D’Elia, L., Strazzullo, P. & Miller, M. A. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33, 414–420 (2010).
Sorensen, M. et al. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ. Health Perspect. 121, 217–222 (2013).
Clark, C. et al. Association of long-term exposure to transportation noise and traffic-related air pollution with the incidence of diabetes: a prospective cohort study. Environ. Health Perspect. 125, 087025 (2017).
Eze, I. C. et al. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int. J. Epidemiol. 46, 1115–1125 (2017).
Ohlwein, S. et al. Indoor and outdoor road traffic noise and incident diabetes: Results from a longitudional German cohort study. Environ. Epidemiol. 3, e037 (2019).
Jorgensen, J. T. et al. Long-term exposure to road traffic noise and incidence of diabetes in the danish nurse cohort. Env. Health Perspect. 127, 57006 (2019).
Vienneau, D., Eze, I. C., Probst-Hensch, N. & Röösli, M. Association between transportation noise and cardio-metabolic diseases: an update of the WHO meta-analysis. Proceedings of the 23rd International Conference on Acoustics 1543–1550 (ICA, 2019).
Pyko, A. et al. Long-term exposure to transportation noise in relation to development of obesity-a cohort study. Environ. Health Perspect. 125, 117005 (2017).
Foraster, M. et al. Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Env. Int. 121, 879–889 (2018).
Christensen, J. S. et al. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: A cohort study. Environ. Res. 143, 154–161 (2015).
Sorensen, M., Sorensen, T. I. A., Ketzel, M. & Raaschou-Nielsen, O. Exposure to traffic noise and gestational weight gain and postpartum weight retention: a cohort study. Occup. Env. Med. 77, 107–114 (2020).
Eriksson, C. et al. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: a prospective study. Environ. Health Perspect. 122, 687–694 (2014).
Pyko, A. et al. Exposure to traffic noise and markers of obesity. Occup. Environ. Med. 72, 594–601 (2015).
Christensen, J. S. et al. Road traffic and railway noise exposures and adiposity in adults: a cross-sectional analysis of the danish diet, cancer, and health cohort. Environ. Health Perspect. 124, 329–335 (2016).
Foraster, M. et al. Long-term transportation noise annoyance is associated with subsequent lower levels of physical activity. Env. Int. 91, 341–349 (2016).
Roswall, N. et al. Residential exposure to traffic noise and leisure-time sports — a population-based study. Int. J. Hyg. Env. Health 220, 1006–1013 (2017).
Roswall, N. et al. Associations between residential traffic noise exposure and smoking habits and alcohol consumption — a population-based study. Env. Pollut. 236, 983–991 (2018).
Clark, C. & Paunovic, K. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and quality of life, wellbeing and mental health. Int. Environ. Res. Public Health 15, 2400 (2018).
He, S. et al. Residential noise exposure and the longitudinal risk of hospitalization for depression after pregnancy: Postpartum and beyond. Env. Res. 170, 26–32 (2019).
Orban, E. et al. Residential road traffic noise and high depressive symptoms after five years of follow-up: results from the heinz nixdorf recall study. Env. Health Perspect. 124, 578–585 (2016).
Seidler, A. et al. Association between aircraft, road and railway traffic noise and depression in a large case-control study based on secondary data. Environ. Res. 152, 263–271 (2017).
Clark, C., Crumpler, C. & Notley, A. H. Evidence for environmental noise effects on health for the United Kingdom policy context: a systematic review of the effects of environmental noise on mental health, wellbeing, quality of life, cancer, dementia, birth, reproductive outcomes, and cognition. Int. J. Environ. Res. Public Health 17, 393 (2020).
Jarup, L. et al. Hypertension and exposure to noise near airports: the HYENA study. Environ. Health Perspect. 116, 329–333 (2008).
Vienneau, D. et al. Facades, floors and maps - Influence of exposure measurement error on the association between transportation noise and myocardial infarction. Env. Int. 123, 399–406 (2019).
Babisch, W. Stress hormones in the research on cardiovascular effects of noise. Noise Health 5, 1–11 (2003).
Münzel, T. et al. Environmental noise and the cardiovascular system. J. Am. Coll. Cardiol. 71, 688–697 (2018).
Babisch, W. et al. Noise annoyance–a modifier of the association between noise level and cardiovascular health? Sci. Total. Environ. 452-453, 50–57 (2013).
Hahad, O. et al. Annoyance to different noise sources is associated with atrial fibrillation in the Gutenberg Health Study. Int. J. Cardiol. 264, 79–84 (2018).
Meyer, T. & Wirtz, P. H. Mechanisms of mitochondrial redox signaling in psychosocial stress-responsive systems: new insights into an old story. Antioxid. Redox Signal. 28, 760–772 (2018).
Xia, N. & Li, H. Loneliness, social isolation, and cardiovascular health. Antioxid. Redox Signal. 28, 837–851 (2018).
Daiber, A. et al. Environmental noise induces the release of stress hormones and inflammatory signaling molecules leading to oxidative stress and vascular dysfunction-Signatures of the internal exposome. Biofactors 45, 495–506 (2019).
Münzel, T. et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur. Heart J. 38, 2838–2849 (2017).
Münzel, T. et al. Airborne disease: a case of a Takotsubo cardiomyopathie as a consequence of nighttime aircraft noise exposure. Eur. Heart J. 37, 2844 (2016).
Wallerath, T. et al. Down-regulation of the expression of endothelial NO synthase is likely to contribute to glucocorticoid-mediated hypertension. Proc. Natl Acad. Sci. USA 96, 13357–13362 (1999).
Yang, S. & Zhang, L. Glucocorticoids and vascular reactivity. Curr. Vasc. Pharmacol. 2, 1–12 (2004).
Osborne, M. T. et al. A neurobiological mechanism linking transportation noise to cardiovascular disease in humans. Eur. Heart J. 41, 772–782 (2020).
Münzel, T., Steven, S., Hahad, O. & Daiber, A. The sixth sense is involved in noise-induced stress responses and vascular inflammation: evidence for heightened amygdalar activity in response to transport noise in man. Eur. Heart J. 41, 783–785 (2020).
Jansen, G. The effect of noise during physical work. Int. Z. Angew. Physiol. 20, 233–239 (1964).
Jansen, G. & Klensch, H. Alteration of the ballistogram by sound impressions and by music. Int. Z. Angew. Physiol. 20, 258–270 (1964).
Jansen, G. Effects of noise on health. Ger. Med. Mon. 13, 446–448 (1968).
Babisch, W., Ising, H., Gallacher, J. E., Sharp, D. S. & Baker, I. A. Traffic noise and cardiovascular risk: the Speedwell study, first phase. Outdoor noise levels and risk factors. Arch. Env. Health 48, 401–405 (1993).
Lusk, S. L., Gillespie, B., Hagerty, B. M. & Ziemba, R. A. Acute effects of noise on blood pressure and heart rate. Arch. Env. Health 59, 392–399 (2004).
Dratva, J. et al. Transportation noise and blood pressure in a population-based sample of adults. Environ. Health Perspect. 120, 50–55 (2011).
Haralabidis, A. S. et al. Acute effects of night-time noise exposure on blood pressure in populations living near airports. Eur. Heart J. 29, 658–664 (2008).
Bagheri Hosseinabadi, M., Khanjani, N., Münzel, T., Daiber, A. & Yaghmorloo, M. Chronic occupational noise exposure: effects on DNA damage, blood pressure, and serum biochemistry. Mutat. Res. 841, 17–22 (2019).
Schmidt, F. et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin. Res. Cardiol. 104, 23–30 (2015).
Herzog, J. et al. Acute exposure to nocturnal train noise induces endothelial dysfunction and pro-thromboinflammatory changes of the plasma proteome in healthy subjects. Basic. Res. Cardiol. 114, 46 (2019).
Schmidt, F. P. et al. The impact of aircraft noise on vascular and cardiac function in relation to noise event number – a randomized trial. Cardiovasc Res. https://doi.org/10.1093/cvr/cvaa204 (2020).
Kim, A. et al. Effects of self-reported sensitivity and road-traffic noise levels on the immune system. PLoS ONE 12, e0187084 (2017).
Cai, Y. et al. Long-term exposure to road traffic noise, ambient air pollution, and cardiovascular risk factors in the HUNT and lifelines cohorts. Eur. Heart J. 38, 2290–2296 (2017).
Thiesse, L. et al. Transportation noise impairs cardiovascular function without altering sleep: The importance of autonomic arousals. Environ. Res. 182, 109086 (2020).
Eze, I. C. et al. Genome-Wide DNA methylation in peripheral blood and long-term exposure to source-specific transportation noise and air pollution: The SAPALDIA study. Environ. Health Perspect. 128, 67003 (2020).
Foraster, M. et al. Exposure to road, railway, and aircraft noise and arterial stiffness in the SAPALDIA study: annual average noise levels and temporal noise characteristics. Environ. Health Perspect. 125, 097004 (2017).
Kalsch, H. et al. Are air pollution and traffic noise independently associated with atherosclerosis: the Heinz Nixdorf Recall Study. Eur. Heart J. 35, 853–860 (2014).
Hennig, F. et al. Investigation of air pollution and noise on progression of thoracic aortic calcification: results of the Heinz Nixdorf Recall Study. Eur. J. Prev. Cardiol. 27, 965–974 (2020).
Atanackovic, D., Brunner-Weinzierl, M. C., Kroger, H., Serke, S. & Deter, H. C. Acute psychological stress simultaneously alters hormone levels, recruitment of lymphocyte subsets, and production of reactive oxygen species. Immunol. Invest. 31, 73–91 (2002).
Herbert, T. B. et al. Cardiovascular reactivity and the course of immune response to an acute psychological stressor. Psychosom. Med. 56, 337–344 (1994).
Altura, B. M., Altura, B. T., Gebrewold, A., Ising, H. & Gunther, T. Noise-induced hypertension and magnesium in rats: relationship to microcirculation and calcium. J. Appl. Physiol. 72, 194–202 (1992).
Wu, C. C., Chen, S. J. & Yen, M. H. Effects of noise on blood pressure and vascular reactivities. Clin. Exp. Pharmacol. Physiol. 19, 833–838 (1992).
Wu, C. C., Chen, S. J. & Yen, M. H. Attenuation of endothelium-dependent relaxation in mesenteric artery during noise-induced hypertension. J. Biomed. Sci. 1, 49–53 (1994).
Lenzi, P. et al. DNA damage associated with ultrastructural alterations in rat myocardium after loud noise exposure. Environ. Health Perspect. 111, 467–471 (2003).
Frenzilli, G. et al. Effects of loud noise exposure on DNA integrity in rat adrenal gland. Environ. Health Perspect. 112, 1671–1672 (2004).
Turner, J. G., Parrish, J. L., Hughes, L. F., Toth, L. A. & Caspary, D. M. Hearing in laboratory animals: strain differences and nonauditory effects of noise. Comp. Med. 55, 12–23 (2005).
Baldwin, A. L. & Bell, I. R. Effect of noise on microvascular integrity in laboratory rats. J. Am. Assoc. Lab. Anim. Sci. 46, 58–65 (2007).
Reif, R., Zhi, Z., Dziennis, S., Nuttall, A. L. & Wang, R. K. Changes in cochlear blood flow in mice due to loud sound exposure measured with Doppler optical microangiography and laser Doppler flowmetry. Quant. Imaging Med. Surg. 3, 235–242 (2013).
Fetoni, A. R. et al. The redox protein p66(shc) mediates cochlear vascular dysfunction and transient noise-induced hearing loss. Sci. Rep. 6, 25450 (2016).
Lousinha, A. et al. Infrasound induces coronary perivascular fibrosis in rats. Cardiovasc. Pathol. 37, 39–44 (2018).
Wang, X., Lai, Y., Zhang, X. & Zhao, J. Effect of low-frequency but high-intensity noise exposure on swine brain blood barrier permeability and its mechanism of injury. Neurosci. Lett. 662, 122–128 (2018).
Kröller-Schön, S. et al. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur. Heart J. 39, 3528–3539 (2018).
Hink, U. et al. Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ. Res. 88, E14–E22 (2001).
Mollnau, H. et al. Effects of angiotensin II infusion on the expression and function of NAD(P)H oxidase and components of nitric oxide/cGMP signaling. Circ. Res. 90, E58–E65 (2002).
Oelze, M. et al. Vasodilator-stimulated phosphoprotein serine 239 phosphorylation as a sensitive monitor of defective nitric Oxide/cGMP signaling and endothelial dysfunction. Circ. Res. 87, 999–1005 (2000).
Münzel, T. et al. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur. Heart J. 41, 4057–4070 (2020).
Steven, S. et al. Exacerbation of adverse cardiovascular effects of aircraft noise in an animal model of arterial hypertension. Redox Biol. 34, 101515 (2020).
Kvandova, M. et al. Environmental aircraft noise aggravates oxidative DNA damage, granulocyte oxidative burst and nitrate resistance in Ogg1(-/-) mice. Free Radic. Res. 54, 280–292 (2020).
Daiber, A. et al. Oxidative stress and inflammation contribute to traffic noise-induced vascular and cerebral dysfunction via uncoupling of nitric oxide synthases. Redox Biol. 34, 101506 (2020).
Campeau, S. et al. Hypothalamic pituitary adrenal axis responses to low-intensity stressors are reduced after voluntary wheel running in rats. J. Neuroendocrinol. 22, 872–888 (2010).
Burow, A., Day, H. E. & Campeau, S. A detailed characterization of loud noise stress: Intensity analysis of hypothalamo-pituitary-adrenocortical axis and brain activation. Brain Res. 1062, 63–73 (2005).
Eraslan, E., Akyazi, I., Erg, L. E. E. & Matur, E. Noise stress changes mRNA expressions of corticotropin-releasing hormone, its receptors in amygdala, and anxiety-related behaviors. Noise Health 17, 141–147 (2015).
Gannouni, N. et al. Qualitative and quantitative assessment of noise at moderate intensities on extra-auditory system in adult rats. Noise Health 15, 406–411 (2013).
Said, M. A. & El-Gohary, O. A. Effect of noise stress on cardiovascular system in adult male albino rat: implication of stress hormones, endothelial dysfunction and oxidative stress. Gen. Physiol. Biophys. 35, 371–377 (2016).
Schiavone, S., Jaquet, V., Trabace, L. & Krause, K. H. Severe life stress and oxidative stress in the brain: from animal models to human pathology. Antioxid. Redox Signal. 18, 1475–1490 (2013).
Wright, J. W., Dengerink, H. A., Miller, J. M. & Goodwin, P. C. Potential role of angiotensin II in noise-induced increases in inner ear blood flow. Hear. Res. 17, 41–46 (1985).
Ye, S., Zhong, H., Yanamadala, S. & Campese, V. M. Oxidative stress mediates the stimulation of sympathetic nerve activity in the phenol renal injury model of hypertension. Hypertension 48, 309–315 (2006).
Lob, H. E. et al. Induction of hypertension and peripheral inflammation by reduction of extracellular superoxide dismutase in the central nervous system. Hypertension 55, 277–283 (2010).
Neri, M. et al. Correlation between cardiac oxidative stress and myocardial pathology due to acute and chronic norepinephrine administration in rats. J. Cell. Mol. Med. 11, 156–170 (2007).
Lee, H. Y. et al. The ethanol extract of Aquilariae Lignum ameliorates hippocampal oxidative stress in a repeated restraint stress mouse model. BMC Complement. Altern. Med. 17, 397 (2017).
Grande, M. T. et al. Increased oxidative stress, the renin-angiotensin system, and sympathetic overactivation induce hypertension in kidney androgen-regulated protein transgenic mice. Free Radic. Biol. Med. 51, 1831–1841 (2011).
Rajagopalan, S. et al. Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. Contribution to alterations of vasomotor tone. J. Clin. Invest. 97, 1916–1923 (1996).
Mollnau, H. et al. Mechanisms of increased vascular superoxide production in an experimental model of idiopathic dilated cardiomyopathy. Arterioscler. Thromb. Vasc. Biol. 25, 2554–2559 (2005).
Chen, D. D., Dong, Y. G., Yuan, H. & Chen, A. F. Endothelin 1 activation of endothelin A receptor/NADPH oxidase pathway and diminished antioxidants critically contribute to endothelial progenitor cell reduction and dysfunction in salt-sensitive hypertension. Hypertension 59, 1037–1043 (2012).
Rajagopalan, S. et al. Role for endothelin-1 in angiotensin II-mediated hypertension. Hypertension 30, 29–34 (1997).
Jones, R. M. & Neish, A. S. Redox signaling mediated by the gut microbiota. Free Radic. Biol. Med. 105, 41–47 (2017).
Campbell, E. L. & Colgan, S. P. Control and dysregulation of redox signalling in the gastrointestinal tract. Nat. Rev. Gastroenterol. Hepatol. 16, 106–120 (2019).
Cryan, J. F. & Dinan, T. G. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 13, 701–712 (2012).
Collins, S. M., Surette, M. & Bercik, P. The interplay between the intestinal microbiota and the brain. Nat. Rev. Microbiol. 10, 735–742 (2012).
Cui, B. et al. Effects of chronic noise exposure on the microbiome-gut-brain axis in senescence-accelerated prone mice: implications for Alzheimer’s disease. J. Neuroinflammation 15, 190 (2018).
Cui, B., Gai, Z., She, X., Wang, R. & Xi, Z. Effects of chronic noise on glucose metabolism and gut microbiota-host inflammatory homeostasis in rats. Sci. Rep. 6, 36693 (2016).
Zymantiene, J. et al. Effects of long-term construction noise on health of adult female Wistar rats. Pol. J. Vet. Sci. 20, 155–165 (2017).
Hadizadeh, M., Hamidi, G. A. & Salami, M. Probiotic supplementation improves the cognitive function and the anxiety-like behaviors in the stressed rats. Iran. J. Basic. Med. Sci. 22, 506–514 (2019).
Karl, J. P. et al. Effects of psychological, environmental and physical stressors on the gut microbiota. Front. Microbiol. 9, 2013 (2018).
Crnko, S., Du Pre, B. C., Sluijter, J. P. G. & Van Laake, L. W. Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nat. Rev. Cardiol. 16, 437–447 (2019).
Park, J. S. et al. Identification of a circadian clock in the inferior colliculus and its dysregulation by noise exposure. J. Neurosci. 36, 5509–5519 (2016).
Putker, M. & O’Neill, J. S. Reciprocal control of the circadian clock and cellular redox state - a critical appraisal. Mol. Cell 39, 6–19 (2016).
Li, H. et al. Influence of mental stress and environmental toxins on circadian clocks: Implications for redox regulation of the heart and cardioprotection. Br. J. Pharmacol. 177, 5393–5412 (2020).
Schmalen, I. et al. Interaction of circadian clock proteins CRY1 and PER2 is modulated by zinc binding and disulfide bond formation. Cell 157, 1203–1215 (2014).
Ordovas, J. M. & Smith, C. E. Epigenetics and cardiovascular disease. Nat. Rev. Cardiol. 7, 510–519 (2010).
Kuznetsova, T., Prange, K. H. M., Glass, C. K. & de Winther, M. P. J. Transcriptional and epigenetic regulation of macrophages in atherosclerosis. Nat. Rev. Cardiol. 17, 216–228 (2020).
Miguel, V. et al. The role of MicroRNAs in environmental risk factors, noise-induced hearing loss, and mental stress. Antioxid. Redox Signal. 28, 773–796 (2018).
Meerson, A. et al. Changes in brain microRNAs contribute to cholinergic stress reactions. J. Mol. Neurosci. 40, 47–55 (2010).
Greco, C. M. & Condorelli, G. Epigenetic modifications and noncoding RNAs in cardiac hypertrophy and failure. Nat. Rev. Cardiol. 12, 488–497 (2015).
Guo, L. et al. Effects of environmental noise exposure on DNA methylation in the brain and metabolic health. Environ. Res. 153, 73–82 (2017).
Sainani, K. Taking on the exposome - bringing bioinformatics tools to the environmental side of the health equation. Biomed. Comput. Rev. 2016, 14–21 (2016).
Héritier, H. et al. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur. Heart J. 40, 598–603 (2019).
Sorensen, M. et al. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environ. Res. 133, 49–55 (2014).
Babisch, W. et al. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: the KORA study. Environ. Health Perspect. 122, 492–498 (2014).
Vienneau, D. et al. Years of life lost and morbidity cases attributable to transportation noise and air pollution: A comparative health risk assessment for Switzerland in 2010. Int. J. Hyg. Env. Health 218, 514–521 (2015).
Münzel, T. et al. Effects of gaseous and solid constituents of air pollution on endothelial function. Eur. Heart J. 39, 3543–3550 (2018).
Daiber, A. et al. The “exposome” concept - how environmental risk factors influence cardiovascular health. Acta Biochim. Pol. 66, 269–283 (2019).
Daiber, A. & Münzel, T. Special Issue “Impact of environmental pollution and stress on redox signaling and oxidative stress pathways”. Redox Biol. 37, 101621 (2020).
Münzel, T. & Daiber, A. Environmental stressors and their impact on health and disease with focus on oxidative stress. Antioxid. Redox Signal. 28, 735–740 (2018).
European Commission. Science for environment policy. IN-DEPTH REPORT 13. Links between noise and air pollution and socioeconomic status https://ec.europa.eu/environment/integration/research/newsalert/pdf/air_noise_pollution_socioeconomic_status_links_IR13_en.pdf (2016).
Knuuti, J. et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 41, 407–477 (2020).
Harder, S. & Klinkhardt, U. Thrombolytics: drug interactions of clinical significance. Drug Saf. 23, 391–399 (2000).
Dzhambov, A. M. & Lercher, P. Road traffic noise exposure and depression/anxiety: an updated systematic review and meta-analysis. Int. J. Environ. Res. Public Health 16, 4134 (2019).
T. Münzel, et al. Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur. Heart J. 38, 550–556 (2017).
Münzel, T., Gori, T., Babisch, W. & Basner, M. Cardiovascular effects of environmental noise exposure. Eur. Heart J. 35, 829–836 (2014).
Münzel, T. Endothelial dysfunction: pathophysiology, diagnosis and prognosis. Dtsch. Med. Wochenschr. 133, 2465–2470 (2008).
Vrijheid, M. The exposome: a new paradigm to study the impact of environment on health. Thorax 69, 876–878 (2014).
European Commission https://ec.europa.eu/info/events/launch-event-european-human-exposome-network-2020_en (2020).
Koay, G., Heffner, R. & Heffner, H. Behavioral audiograms of homozygous med(J) mutant mice with sodium channel deficiency and unaffected controls. Hear. Res. 171, 111–118 (2002).
Heffner, H. E., Heffner, R. S., Contos, C. & Ott, T. Audiogram of the hooded Norway rat. Hear. Res. 73, 244–247 (1994).
Martin, G. K., Lonsbury-Martin, B. L. & Kimm, J. A rabbit preparation for neuro-behavioral auditory research. Hear. Res. 2, 65–78 (1980).
Kojima, S. Comparison of auditory functions in the chimpanzee and human. Folia Primatol. 55, 62–72 (1990).
Jackson, L. L., Heffner, R. S. & Heffner, H. E. Free-field audiogram of the Japanese macaque (Macaca fuscata). J. Acoust. Soc. Am. 106, 3017–3023 (1999).
Acknowledgements
We gratefully acknowledge financial support in the form of vascular biology research grants from the Foundation Heart of Mainz (to T.M. and A.D.) and from the Boehringer Ingelheim Foundation for the collaborative research group ‘Novel and neglected cardiovascular risk factors: molecular mechanisms and therapeutic implications’ to study the effects of environmental risk factors on vascular function and oxidative stress. T.M. is a principal investigator of the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany. We also thank M. Neuser (University Medical Center Mainz, Germany) for her expert graphical assistance with the figures before submission.
Review criteria
For the mechanistic discussion of human data, we have mainly considered translational human studies from the past 20 years with a focus on the cardiovascular system or on stress, inflammatory and oxidative pathways related to cardiovascular disease. Experimental research on the cardiovascular or neuropsychological effects of transportation noise in humans is scarce. For the discussion on animal models, we focus on studies from the past 20 years that did not relate only to hearing loss. Research on the cardiovascular effects of non-auditory noise in animals is very rare. For the period before 2000, we selected only the landmark studies.
Author information
Authors and Affiliations
Contributions
The authors contributed substantially to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks M. Röösli and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Münzel, T., Sørensen, M. & Daiber, A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol 18, 619–636 (2021). https://doi.org/10.1038/s41569-021-00532-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-021-00532-5
This article is cited by
-
Noise annoyance and cardiovascular disease risk: results from a 10-year follow-up study
Scientific Reports (2024)
-
Noise and mental health: evidence, mechanisms, and consequences
Journal of Exposure Science & Environmental Epidemiology (2024)
-
Noise annoyance due to different sources is associated with tinnitus presence and distress in the general population
Journal of Exposure Science & Environmental Epidemiology (2024)
-
Effects of lifestyle factors on leukocytes in cardiovascular health and disease
Nature Reviews Cardiology (2024)
-
Luftverschmutzung und Lärm, Einfluss auf bzw. Ursache bei Herzerkrankungen
Die Kardiologie (2024)