Abstract
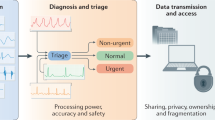
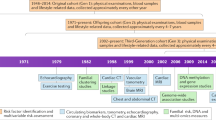
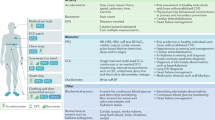
The first issue of Nature Reviews Cardiology was published in November 2004 under the name Nature Clinical Practice Cardiovascular Medicine. To celebrate our 15th anniversary in 2019, we invited six of our Advisory Board members to discuss what they considered the most important advances in their field of cardiovascular research or clinical practice in the past 15 years and what changes they envision for cardiovascular medicine in the next 15 years. Several practice-changing breakthroughs are described, including advances in procedural techniques to treat arrhythmias and hypertension and the development of novel therapeutic strategies to treat heart failure and pulmonary arterial hypertension, as well as those that target risk factors such as inflammation and elevated LDL-cholesterol levels. Furthermore, these key opinion leaders predict that machine learning technology and data derived from wearable devices will pave the way towards the coveted goal of personalized medicine.
The contributors
J.M.K. leads both clinical and research groups in the Department of Heart Rhythm Disorders at the Royal Melbourne Hospital and University of Melbourne, Melbourne, Australia. He has an international reputation as a leader in the field of atrial arrhythmia research and has authored >380 peer-reviewed publications. He serves on the editorial board of 12 international cardiology journals and is an associate editor of JACC Clinical Electrophysiology. He is the immediate past president of the Asia Pacific Heart Rhythm Society and served as scientific chair of the Cardiac Society of Australia and New Zealand for 6 years.
S.L. is Professor in Biochemistry & Molecular Biology at the Faculty of Chemical & Pharmaceutical Sciences and Professor in Cell & Molecular Biology in the Faculty of Medicine, University of Chile in Santiago, Chile and adjunct professor in the Cardiology Division, University of Texas Southwestern Medical Center in Dallas, USA. He is also the director of the Advanced Center for Chronic Diseases (ACCDiS) in Santiago, Chile. He has published >260 articles in peer-reviewed journals, as well as book chapters. He is the current president of the Latino-American section of the International Society for Heart Research (ISHR) and an associate editor for Circulation. His research interests include cell signalling in the cardiovascular system, specifically the molecular mechanisms that regulate energy metabolism, hypertrophy, and death and survival of the heart, as well as important processes in the development of diseases, such as myocardial infarction, hypertension and heart failure (HF). Recently, his work has focused on the regulation of mitochondrial dynamics and function in the heart, inter-organelle communication in chronic diseases, primary cilia and polycystins in heart function, the non-canonical renin–angiotensin system and mechanisms in the genesis and development of HF with preserved ejection fraction (EF).
F.M. is Professor of Medicine and deputy director of the Department for Internal Medicine and Cardiology at Saarland University Hospital, and visiting professor at Harvard–MIT, Biomedical Engineering, Boston, MA, USA. He holds board certifications in internal medicine, cardiology, intensive care medicine, emergency medicine and hypertension. He serves as vice-chair of the Working Group for Interventional Hypertension Treatment of the European Society of Hypertension (ESH), a board member of the European Society of Cardiology (ESC) Council on Hypertension and a writing committee member of the 2018 ESC/ESH hypertension guidelines.
M.N. is a professor at Harvard Medical School and principal investigator at the Center for Systems Biology at Massachusetts General Hospital, Boston, MA, USA. His laboratory examines the cellular and molecular processes in atherosclerosis and myocardial infarction, with a particular focus on myeloid cells and the haematopoietic system.
M.H.Y. is Professor of Cardiothoracic Surgery at the National Heart and Lung Institute, Imperial College London, and founder and director of research at the Harefield Heart Science Centre (The Magdi Yacoub Institute), London, UK, overseeing >60 scientists and students in the areas of tissue-engineered heart valves, myocardial regeneration, novel left ventricular assist devices, stem cell biology, end-stage HF and transplantation immunology. He established the largest heart and lung transplantation programme in the world. He founded the Chain of Hope in 1995 to treat children with correctable cardiac conditions from war-torn and developing countries and established training and research programmes in local cardiac units. He also founded the Aswan Heart Centre in 2009, offering medical services free of charge to all patients and advancing basic science and biomedical research in Egypt.
D.Z. is a professor at the Capital Medical University, Beijing Anzhen Hospital in Beijing, China. She is a member of the China National Expert Committee for Cardiovascular Diseases, the Chinese Society of Preventive Cardiology and the Cardiology Society of Chinese Medical Doctors Association. She is also on the advisory or editorial board of journals including Nature Reviews Cardiology, International Journal of Cardiology and Chinese Journal of Cardiology. She has been involved in writing several international or China-specific guidelines for various topics of preventive cardiology, including management of dyslipidaemia and hypertension.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Haissaguerre, M. et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 339, 659–666 (1998).
Haissaguerre, M. et al. Electrophysiological end point for catheter ablation of atrial fibrillation initiated from multiple pulmonary venous foci. Circulation 101, 1409–1417 (2000).
Kanj, M. H. et al. Pulmonary vein antral isolation using an open irrigation ablation catheter for the treatment of atrial fibrillation: a randomized pilot study. J. Am. Coll. Cardiol. 49, 1634–1641 (2007).
Phlips, T. et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace 20, f419–f427 (2018).
Natale, A. et al. Paroxysmal AF catheter ablation with a contact force sensing catheter: results of the prospective, multicenter SMART-AF trial. J. Am. Coll. Cardiol. 64, 647–656 (2014).
Neven, K. et al. Fatal end of a safety algorithm for pulmonary vein isolation with use of high-intensity focused ultrasound. Circ. Arrhythm. Electrophysiol. 3, 260–265 (2010).
Kuck, K. H. et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N. Engl. J. Med. 374, 2235–2245 (2016).
Mark, D. B. et al. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 321, 1275–1285 (2019).
Packer, D. L. et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 321, 1261–1274 (2019).
Friberg, L. et al. Catheter ablation for atrial fibrillation is associated with lower incidence of stroke and death: data from Swedish health registries. Eur. Heart J. 37, 2478–2487 (2016).
Marrouche, N. F. et al. Catheter ablation for atrial fibrillation with heart failure. N. Engl. J. Med. 378, 417–427 (2018).
Verma, A. et al. Approaches to catheter ablation for persistent atrial fibrillation. N. Engl. J. Med. 372, 1812–1822 (2015).
Lau, D. H., Nattel, S., Kalman, J. M. & Sanders, P. Modifiable risk factors and atrial fibrillation. Circulation 136, 583–596 (2017).
WHO. Global Status Report on Noncommunicable Diseases 2014. WHO https://www.who.int/nmh/publications/ncd-status-report-2014/en/ (2014).
WHO. Noncommunicable Diseases Country Profiles 2018. WHO https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (2018).
Dadu, R. T. & Ballantyne, C. M. Lipid lowering with PCSK9 inhibitors. Nat. Rev. Cardiol. 11, 563–575 (2014).
Robinson, J. G. et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N. Engl. J. Med. 372, 1489–1499 (2015).
Sabatine, M. S. et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 376, 1713–1722 (2017).
Ridker, P. M. et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N. Engl. J. Med. 377, 1119–1131 (2017).
Ruparelia, N., Chai, J. T., Fisher, E. A. & Choudhury, R. P. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat. Rev. Cardiol. 14, 133–144 (2017).
McMurray, J. J. Angiotensin–neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 371, 993–1004 (2014).
Gu, J. et al. Pharmacokinetics and pharmacodynamics of LCZ696, a novel dual-acting angiotensin receptor–neprilysin inhibitor (ARNi). J. Clin. Pharmacol. 50, 401–414 (2010).
Seferovic, J. P. et al. Effect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: a post-hoc analysis from the PARADIGM-HF trial. Lancet Diabetes Endocrinol. 5, 333–340 (2017).
Raz, I. & Cahn, A. Heart failure: SGLT2 inhibitors and heart failure—clinical implications. Nat. Rev. Cardiol. 13, 185–186 (2016).
Wright, E. M. Renal Na+ glucose cotransporters. Am. J. Physiol. Renal Physiol. 280, F10–F18 (2001).
Chao, E. C. SGLT-2 inhibitors: a new mechanism for glycemic control. Clin. Diabetes 32, 4–11 (2014).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes and mortality in type 2 diabetes. N. Engl. J. Med. 373, 2117–2128 (2015).
Kosiborod, M. et al. Lower risk of heart failure and death in patients initiated on sodium–glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL study. Circulation 136, 249–259 (2017).
Schiattarella, G. G. et al. Nitrosative stress drives heart failure with preserved ejection fraction. Nature 568, 351–356 (2019).
Ranganathan, S., Nakai, K. & Schönbach, C. Encyclopedia of Bioinformatics and Computational Biology: abc of Bioinformatics 1st edn (Elsevier, 2019).
Tsay, D. & Patterson, C. From machine learning to artificial intelligence applications in cardiac care. Circulation 138, 2569–2575 (2018).
Topol, E. Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again eBook (Basic Books, 2019).
Forouzanfar, M. H. et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA 317, 165–182 (2017).
Berra, E. et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension 68, 297–306 (2016).
Schlaich, M. P., Sobotka, P. A., Krum, H., Lambert, E. & Esler, M. D. Renal sympathetic-nerve ablation for uncontrolled hypertension. N. Engl. J. Med. 361, 932–934 (2009).
Mahfoud, F., Schlaich, M., Böhm, M., Esler, M. & Lüscher, T. F. Catheter-based renal denervation: the next chapter begins. Eur. Heart J. 39, 4144–4149 (2018).
Böhm, M., Linz, D., Ukena, C., Esler, M. & Mahfoud, F. Renal denervation for the treatment of cardiovascular high risk-hypertension or beyond? Circ. Res. 115, 400–409 (2014).
Krum, H. et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 383, 622–629 (2014).
Esler, M. D. et al. Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur. Heart J. 35, 1752–1759 (2014).
Azizi, M. et al. Optimum and stepped care standardised antihypertensive treatment with or without renal denervation for resistant hypertension (DENERHTN): a multicentre, open-label, randomised controlled trial. Lancet 385, 1957–1965 (2015).
Bhatt, D. L. et al. A controlled trial of renal denervation for resistant hypertension. N. Engl. J. Med. 370, 1393–1401 (2014).
Kandzari, D. E. et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur. Heart J. 36, 219–227 (2015).
Mahfoud, F. et al. Proceedings from the European Clinical Consensus Conference for renal denervation: considerations on future clinical trial design. Eur. Heart J. 36, 2219–2227 (2015).
Mahfoud, F. et al. Proceedings from the 2nd European Clinical Consensus Conference for device-based therapies for hypertension: state of the art and considerations for the future. Eur. Heart J. 38, 3272–3281 (2017).
Townsend, R. R. et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 390, 2160–2170 (2017).
Kandzari, D. E. et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet 6736, 1–10 (2018).
Azizi, M. et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet 391, 2335–2345 (2018).
Hering, D. et al. Substantial reduction in single sympathetic nerve firing after renal denervation in patients with resistant hypertension. Hypertension 61, 457–464 (2013).
Böhm, M. et al. Ambulatory heart rate reduction after catheter-based renal denervation in hypertensive patients not receiving anti-hypertensive medications: data from SPYRAL HTN-OFF MED, a randomized, sham-controlled, proof-of-concept trial. Eur. Heart J. 40, 743–751 (2019).
Linz, D. et al. Catheter-based renal denervation reduces atrial nerve sprouting and complexity of atrial fibrillation in goats. Circ. Arrhythm. Electrophysiol. 8, 466–474 (2015).
Linz, D. et al. Renal sympathetic denervation suppresses postapneic blood pressure rises and atrial fibrillation in a model for sleep apnea. Hypertension 60, 172–178 (2012).
Pinto, A. R. et al. An abundant tissue macrophage population in the adult murine heart with a distinct alternatively-activated macrophage profile. PLOS ONE 7, e36814 (2012).
Heidt, T. et al. Differential contribution of monocytes to heart macrophages in steady-state and after myocardial infarction. Circ. Res. 115, 284–295 (2014).
Pinto, A. R. et al. Revisiting cardiac cellular composition. Circ. Res. 118, 400–409 (2016).
Bajpai, G. et al. The human heart contains distinct macrophage subsets with divergent origins and functions. Nat. Med. 24, 1234–1245 (2018).
Hulsmans, M. et al. Macrophages facilitate electrical conduction in the heart. Cell 169, 510–522.e20 (2017).
Ensan, S. et al. Self-renewing resident arterial macrophages arise from embryonic CX3CR1(+) precursors and circulating monocytes immediately after birth. Nat. Immunol. 17, 159–168 (2016).
Epelman, S. et al. Embryonic and adult-derived resident cardiac macrophages are maintained through distinct mechanisms at steady state and during inflammation. Immunity 40, 91–104 (2014).
Chakarov, S. et al. Two distinct interstitial macrophage populations coexist across tissues in specific subtissular niches. Science 363, 6432 (2019).
Leid, J. et al. Primitive embryonic macrophages are required for coronary development and maturation. Circ. Res. 118, 1498–1511 (2016).
Leuschner, F. et al. Rapid monocyte kinetics in acute myocardial infarction are sustained by extramedullary monocytopoiesis. J. Exp. Med. 209, 123–137 (2012).
Godwin, J. W., Pinto, A. R. & Rosenthal, N. A. Macrophages are required for adult salamander limb regeneration. Proc. Natl Acad. Sci. USA 110, 9415–9420 (2013).
Aurora, A. B. et al. Macrophages are required for neonatal heart regeneration. J. Clin. Invest. 124, 1382–1392 (2014).
Srivastava, D. & DeWitt, N. In vivo cellular reprogramming: the next generation. Cell 166, 1386–1396 (2016).
Chen, I. Y., Matsa, E. & Wu, J. C. Induced pluripotent stem cells: at the heart of cardiovascular precision medicine. Nat. Rev. Cardiol. 13, 333–349 (2016).
Hoeper, M. M. et al. A global view of pulmonary hypertension. Lancet Respir. Med. 4, 306–322 (2016).
Rich, S., Haworth, S. G., Hassoun, P. M. & Yacoub, M. H. Pulmonary hypertension: the unaddressed global health burden. Lancet Respir. Med. 6, 577–579 (2018).
Butrous, G. & Mathie, A. Infection in pulmonary vascular diseases: would another consortium really be the way to go? Glob. Cardiol. Sci. Pract. 2019, 1 (2019).
Lau, E. M. T., Giannoulatou, E., Celermajer, D. S. & Humbert, M. Epidemiology and treatment of pulmonary arterial hypertension. Nat. Rev. Cardiol. 14, 603–614 (2017).
Madani, M. M. Surgical treatment of chronic thromboembolic pulmonary hypertension: pulmonary thromboendarterectomy. Methodist DeBakey Cardiovasc. J. 12, 213–218 (2016).
Kolosionek, E., Crosby, A., Harhay, M. O., Morrell, N. & Butrous, G. Pulmonary vascular disease associated with schistosomiasis. Expert Rev. Anti. Infect. Ther. 8, 1467–1473 (2010).
Yacoub, M., Mayosi, B., ElGuindy, A., Carpentier, A. & Yusuf, S. Eliminating acute rheumatic fever and rheumatic heart disease. Lancet. 390, 212–213 (2017).
Jakovljevic, D. G. et al. Left ventricular assist device as a bridge to recovery for patients with advanced heart failure. J. Am. Coll. Cardiol. 69, 1924–1933 (2017).
Atherton, J. J. Stage B heart failure: rationale for screening. Heart Fail. Clin. 8, 273–283 (2012).
Yacoub, M. H. & McLeod, C. The expanding role of implantable devices to monitor heart failure and pulmonary hypertension. Nat. Rev. Cardiol. 15, 770–779 (2018).
Yacoub, M. H. & Terracciano, C. M. Bridge to recovery and the search for decision nodes. Circ. Heart Fail. 4, 393–395 (2011).
Page, A., Messer, S. & Large, S. R. Heart transplantation from donation after circulatory determined death. Ann. Cardiothorac. Surg. 7, 75–81 (2018).
Yacoub, M. Cardiac donation after circulatory death: a time to reflect. Lancet 385, 2554–2556 (2015).
Fischer, K. et al. Efficient production of multi-modified pigs for xenotransplantation by ‘combineering’, gene stacking and gene editing. Sci. Rep. 6, 29081 (2016).
Längin, M. et al. Consistent success in life-supporting porcine cardiac xenotransplantation. Nature 564, 430–433 (2018).
Cooper, D. K. C. et al. Selection of patients for initial clinical trials of solid organ xenotransplantation. Transplantation 101, 1551–1558 (2017).
El-Sherbiny, I. M. & Yacoub, M. H. Hydrogel scaffolds for tissue engineering: progress and challenges. Glob. Cardiol. Sci. Pract. 2013, 316–342 (2013).
Dainis, A. M. et al. Cardiovascular precision medicine in the genomics era. JACC Basic Transl Sci. 3, 313–326 (2018).
Popejoy, A. B. & Fullerton, S. M. Genomics is failing on diversity. Nature 538, 161–164 (2016).
Goldenberg, S. L., Nir, G. & Salcudean, S. E. A new era: artificial intelligence and machine learning in prostate cancer. Nat. Rev. Urol. 16, 391–403 (2019).
Claas, S. A. & Arnett, D. K. The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr. Cardiol. Rep. 18, 56 (2016).
Sotos-Prieto, M. et al. Association between a healthy heart score and the development of clinical cardiovascular risk factors among women: potential role for primordial prevention. Circ. Cardiovasc. Qual. Outcomes 9, S77–S85 (2016).
Carey, R. M. et al. Prevention and control of hypertension: JACC health promotion series. J. Am. Coll. Cardiol. 72, 1278–1293 (2018).
Bi, Y. et al. Status of cardiovascular health in Chinese adults. J. Am. Coll. Cardiol. 65, 1013–1025 (2015).
Wang, Y. et al. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese Multi-Provincial Cohort Study. Eur. J. Prev. Cardiol. 22, 380–388 (2015).
Leening, M. J. et al. Lifetime perspectives on primary prevention of atherosclerotic cardiovascular disease. JAMA 315, 1449–1450 (2016).
Leistner, D. M. & Landmesser, U. Maintaining cardiovascular health in the digital era. Eur. Heart J. 40, 9–12 (2019).
Ference, B. A. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38, 2459–2472 (2017).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, 1269–1324 (2018).
Murphy, A. et al. World Heart Federation cholesterol roadmap. Glob. Heart 12, 179–197 (2017).
Schwartz, G. G. et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N. Engl. J. Med. 367, 2089–2099 (2012).
The STABILITY Investigators. Darapladib for preventing ischemic events in stable coronary heart disease. N. Engl. J. Med. 370, 1702–1711 (2014).
Keene, D. et al. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin fibrates, and CETP inhibitors: meta-analysis of randomized controlled trials including 117,411 patients. BMJ 349, g4379 (2014).
Gaziano, J. M. et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomized, double-blind, placebo-controlled trial. Lancet 392, 1036–1046 (2018).
The ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N. Engl. J. Med. 379, 1529–1539 (2018).
Zheng, S. L. & Roddick, A. J. Association of aspirin use for primary prevention with cardiovascular events and bleeding events. A systematic review and meta-analysis. JAMA 321, 277–287 (2019).
O’Donnell, M. et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 371, 612–623 (2014).
Mente, A. et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiology cohort study. Lancet 392, 496–506 (2018).
Domanski, M. J. et al. Next steps in primary prevention of coronary heart disease. Rationale for and design of the ECAD trial. J. Am. Coll. Cardiol. 66, 1828–1836 (2015).
Zhang, X. G. et al. Twenty-year epidemiologic study on LDL-C levels in relation to the risk of atherosclerotic events, hemorrhagic stroke, and cancer death among young and middle-aged population in China. J. Clin. Lipidol. 12, 1179–1189 (2018).
Rist, P. M. et al. Lipid levels and the risk of hemorrhagic stroke among women. Neurology 92, 1–9 (2019).
Gidwani, S. & Nair, A. The burden of pulmonary hypertension in resource-limited settings. Glob. Heart 9, 297–310 (2014).
Acknowledgements
F.M. is supported by Deutsche Forschungsgemeinschaft (SFB TRR219), Deutsche Gesellschaft für Kardiologie and Deutsche Hochdruckliga. S.L. is supported by Fondo de Financiamiento de Centros de Investigacion en Areas Prioritarias (FONDAP) grant 15130011 from Comision Nacional de Investigacion Cientifica y Tecnologica (CONICYT), Chile. M.N. is supported by grants from the NHLBI HL139598 and HL142494.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, contributed to discussions of content, wrote the manuscript, and reviewed and edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
J.M.K. has received fellowship and research grants from Abbott, and from Biosense Webster and Medtronic in the form of unrestricted grants to the Royal Melbourne Hospital research directorate. F.M. has received speaker honoraria and consultancy fees from Berlin Chemie, Boehringer Ingelheim, Medtronic and ReCor. M.N. has been a paid a consultant fee or received research support from Alnylam, GlaxoSmithKline, IFM Therapeutics, Medtronic, Molecular Imaging, Novartis, Sigilon and Verseaux. The other authors declare no competing interests.
Additional information
Related links
100,000 Genomes Project: https://www.genomicsengland.co.uk/about-genomics-england/the-100000-genomes-project/
Human Heredity and Health in Africa: https://www.afshg.org/h3africa/
Rights and permissions
About this article
Cite this article
Kalman, J.M., Lavandero, S., Mahfoud, F. et al. Looking back and thinking forwards — 15 years of cardiology and cardiovascular research. Nat Rev Cardiol 16, 651–660 (2019). https://doi.org/10.1038/s41569-019-0261-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-019-0261-7
This article is cited by
-
Precision cardiology in the digital era
Nature Reviews Cardiology (2019)