Abstract
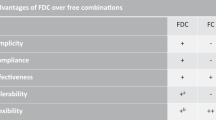
Polypills can contain multiple pharmaceutical agents targeting the cardiovascular system. The use of polypills in the secondary prevention of cardiovascular disease (CVD) has received broad support; however, the use of polypills in the primary prevention of CVD is more controversial. This controversy stems from an inherent resistance to the medicalization of primary prevention, and the lower CVD event rate in this population means that smaller absolute benefits are derived. Indeed, drug-related adverse effects, such as from aspirin, might even outweigh the benefits. The role of fixed-dose combination (FDC) therapy for blood pressure (BP) lowering in combatting the widespread undertreatment of high BP — the leading modifiable risk factor contributing to the global burden of CVD — has gained momentum. Increasing evidence suggests that FDC pills containing multiple low doses of BP-lowering drugs produce more effective BP lowering than the use of fewer separate BP-lowering drugs at higher doses, without an increase in adverse effects. Trials of FDC pills comprising three half-dose or four quarter-dose BP-lowering drugs have shown substantial efficacy. In this Review, we summarize the current evidence on low-dose BP-lowering FDC pills and the justification for this approach in the context of polypills in the primary prevention of CVD.
Key points
-
Polypills containing aspirin, a statin and blood pressure (BP)-lowering drugs have received strong support for the secondary prevention of cardiovascular disease (CVD).
-
Polypills improve adherence to medication and decrease the levels of cardiovascular risk factors, including BP and blood lipids, in small studies with surrogate end points.
-
Barriers to the implementation of polypills in the primary prevention of CVD include patient factors, clinician factors, the evidence base and regulatory and commercialization factors.
-
Fixed-dose combination pills containing multiple BP-lowering drugs at low doses are more effective at lowering BP and have a better adverse event profile than individual drugs taken at full doses.
-
Further evidence is needed on the effectiveness and tolerability of fixed, low-dose, triple-agent or quadruple-agent combination pills compared with usual-care strategies in various populations.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Katsiki, N., Athyros, V. G. & Karagiannis, A. Single-pill combinations: a therapeutic option or necessity for vascular risk treatment? J. Drug Assess. 2, 67–71 (2013).
World Heart Federation. Scaling up the use of ‘polypill’ to improve access to CVD medicines. World Heart Federation https://www.world-heart-federation.org/programmes/polypill/ (2019).
Thom, S. et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD: the UMPIRE randomized clinical trial. JAMA 310, 918–929 (2013).
Wald, N. J. & Law, M. R. A strategy to reduce cardiovascular disease by more than 80%. BMJ 326, 1419 (2003).
Li, Y. et al. Folic acid supplementation and the risk of cardiovascular diseases: a meta-analysis of randomized controlled trials. J. Am. Heart Assoc. 5, e003768 (2016).
McNeil, J. J. et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N. Engl. J. Med. 379, 1509–1518 (2018).
Bahiru, E. et al. Fixed-dose combination therapy for the prevention of atherosclerotic cardiovascular diseases. Cochrane Database Syst. Rev. 3, CD009868 (2017).
Rodgers, A. et al. An international randomised placebo-controlled trial of a four-component combination pill (“polypill”) in people with raised cardiovascular risk. PLOS ONE 6, e19857 (2011).
Malekzadeh, F. et al. A pilot double-blind randomised placebo-controlled trial of the effects of fixed-dose combination therapy (‘polypill’) on cardiovascular risk factors. Int. J. Clin. Pract. 64, 1220–1227 (2010).
Patel, A. et al. A pragmatic randomized trial of a polypill-based strategy to improve use of indicated preventive treatments in people at high cardiovascular disease risk. Eur. J. Prev. Cardiol. 22, 920–930 (2015).
Selak, V. et al. Effect of fixed dose combination treatment on adherence and risk factor control among patients at high risk of cardiovascular disease: randomised controlled trial in primary care. BMJ 348, g3318 (2014).
Soliman, E. Z. et al. A polypill for primary prevention of cardiovascular disease: a feasibility study of the World Health Organization. Trials 12, 3 (2011).
Yusuf, S. et al. Effects of a polypill (Polycap) on risk factors in middle-aged individuals without cardiovascular disease (TIPS): a phase II, double-blind, randomised trial. Lancet 373, 1341–1351 (2009).
Yusuf, S. et al. Comparison of risk factor reduction and tolerability of a full-dose polypill (with potassium) versus low-dose polypill (Polycap) in individuals at high risk of cardiovascular diseases: the Second Indian Polycap Study (TIPS-2) investigators. Circ. Cardiovasc. Qual. Outcomes 5, 463–471 (2012).
Selak, V. et al. Reaching cardiovascular prevention guideline targets with a polypill-based approach: a meta-analysis of randomised clinical trials. Heart 105, 42–45 (2018).
Australian Government Department of the Prime Minister and Cabinet. Closing the gap. Australian Government https://www.pmc.gov.au/indigenous-affairs/closing-gap (2018).
Davidson, P. M., Abbott, P., Davison, J. & Digiacomo, M. Improving medication uptake in aboriginal and Torres Strait islander peoples. Heart Lung Circ. 19, 372–377 (2010).
Ward, S. A., Demos, L., Workman, B. & McNeil, J. J. Aspirin for primary prevention of cardiovascular events in the elderly: current status and future directions. Drugs Aging 29, 251–258 (2012).
Sutcliffe, P. et al. Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews. Health Technol. Assess. 17, 1–253 (2013).
McNeill, J. J. et al. Effect of aspirin on all-cause mortality in the healthy elderly. N. Engl. J. Med. 379, 1519–1528 (2018).
Dube, C. et al. The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann. Intern. Med. 146, 365–375 (2007).
Viera, A. J. et al. Acceptance of a Polypill approach to prevent cardiovascular disease among a sample of U.S. physicians. Prev. Med. 52, 10–15 (2011).
Schwalm, M. R. et al. Polypill for the prevention of cardiovascular disease (PolyIran): study design and rational for a pragmatic cluster randomised controlled trial. Eur. J. Prev. Cardiol. 22, 1609–1617 (2015).
Schwalm, J. R. et al. Rationale and design of a cluster randomised trial of a multifaceted intervention in people with hypertension: the Heart Outcomes Prevention and Evaluation 4 (HOPE-4) study. Am. Heart J. 203, 57–66 (2018).
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. WHO https://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (2010).
Turnbull, F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 362, 1527–1535 (2003).
Chow, C. K. et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 310, 959–968 (2013).
Kishore, S. P., Salam, A., Rodgers, A., Jaffe, M. G. & Frieden, T. Fixed-dose combinations for hypertension. Lancet 392, 819–820 (2018).
Wright, J. T. Jr et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Gabb, G. M. et al. Guideline for the diagnosis and management of hypertension in adults — 2016. Med. J. Aust. 205, 85–89 (2016).
Ferrari, P. Reasons for therapeutic inertia when managing hypertension in clinical practice in non-Western countries. J. Hum. Hypertens. 23, 151–159 (2009).
Nerenberg, K. A. et al. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can. J. Cardiol. 34, 506–525 (2018).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104 (2018).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71, e127–e248 (2018).
Waeber, B. & Brunner, H. R. Low-dose combinations versus monotherapies in the treatment of hypertension. J. Hypertens. Suppl. 15, S17–S20 (1997).
Law, M. R., Wald, N. J., Morris, J. K. & Jordan, R. E. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ 326, 1427 (2003).
Egan, B. M. et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension 59, 1124–1131 (2012).
Bennett, A. et al. Efficacy and safety of quarter-dose blood pressure-lowering agents: a systematic review and meta-analysis of randomized controlled trials. Hypertension 70, 85–93 (2017).
National Institute for Health and Care Excellence. British National Formulary. NICE https://www.nice.org.uk/About/What-we-do/Evidence-Services/British-National-Formulary (2017).
Brayfield, A. Martindale: The Complete Drug Reference 38th edn Vol. 1 & 2 (Pharmaceutical Press, 2014).
Monthly Index of Medical Specialties. Medicine information, data and decision support for the Asia and Pacific region. MIMS http://www.mims.com/resources/portal/common/document/mims/mimsau.htm (2019).
Mahmud, A. & Feely, J. Low-dose quadruple antihypertensive combination: more efficacious than individual agents—a preliminary report. Hypertension 49, 272–275 (2007).
Chow, C. K. et al. Quarter-dose quadruple combination therapy for initial treatment of hypertension: placebo-controlled, crossover, randomised trial and systematic review. Lancet 389, 1035–1042 (2017).
Webster, R. et al. Fixed low-dose triple combination antihypertensive medication versus usual care for blood pressure control in patients with mild to moderate hypertension in Sri Lanka: a randomized clinical trial. JAMA 320, 566–579 (2018).
Wald, D. S., Morris, J. K. & Wald, N. J. Randomized Polypill crossover trial in people aged 50 and over. PLOS ONE 7, e41297 (2012).
Muntner, P. et al. Projected impact of polypill use among US adults: medication use, cardiovascular risk reduction and side effects. Am. Heart J. 161, 719–725 (2011).
World Health Organization. Secondary prevention of noncommunicable diseases in low- and middle-income countries through community-based and health service interventions: World Health Organization–Wellcome Trust meeting report, 1–3 August 2001. WHO https://apps.who.int/iris/handle/10665/42567 (2002).
Sutcliffe, P. et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLOS ONE 8, e81970 (2013).
Australian New Zealand Clinical Trial Registry. ACTRN12616001144404. ANZCTR https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=371315 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03640312 (2018).
Forouzanfar, M. H. et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA 317, 165–182 (2017).
Mills, K. T. et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450 (2016).
Acknowledgements
C.K.C. is supported by a National Health and Medical Research Council of Australia Career Development Fellowship Level 2, co-funded by a Heart Foundation Future Leaders research fellowship. Comments on a draft of the manuscript and assistance with Fig. 1 were provided by A. Rodgers (The George Institute for Global Health, University of New South Wales and Westmead Applied Research Centre, University of Sydney, Australia).
Review criteria
The authors searched EMBASE, MEDLINE and the Cochrane Central Registry of Controlled Trials for relevant papers from inception of the database to August 2018. Selected papers were either randomized clinical trials of polypills containing a combination of LDL-cholesterol-lowering and blood pressure-lowering drugs and aspirin in primary prevention populations or randomized trials of fixed-dose combination drugs containing three or more low-dose blood pressure-lowering agents. The authors also identified studies from the reference lists of important clinical trials and published reviews. The papers were identified by Q.M. and supplemented by knowledge of the literature from C.K.C.
Reviewer information
Nature Reviews Cardiology thanks J. Castellano and other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, discussed its content, wrote the manuscript and revised and edited it before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. George Health Enterprises, the social enterprise arm of the George Institute for Global Health, has received investment to develop polypills containing aspirin, a statin and blood pressure-lowering drugs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chow, C.K., Meng, Q. Polypills for primary prevention of cardiovascular disease. Nat Rev Cardiol 16, 602–611 (2019). https://doi.org/10.1038/s41569-019-0209-y
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-019-0209-y
This article is cited by
-
Association of intensive blood pressure management with cardiovascular outcomes in patients using multiple classes of antihypertensive medications: a post-hoc analysis of the STEP Trial
Hypertension Research (2024)
-
Die kardiovaskuläre Polypille - ein Alleskönner?
CardioVasc (2024)
-
„Polypill“ in der kardiovaskulären Prävention – erfolgreich durch Vereinfachung?
Die Innere Medizin (2023)
-
Polypill as a Personalized Dosage Form: Production Technology (Review)
Pharmaceutical Chemistry Journal (2023)
-
Polypills for the secondary prevention of MACE
Nature Reviews Cardiology (2022)