Abstract
Stent thrombosis (ST) is a rare but severe complication of coronary procedures with high mortality, high relapse rate and a very complex pathophysiology. An individual’s susceptibility to ST is multifactorial and results from interactions between clinical factors, endothelial biology, hypersensitivity and/or inflammatory reactions, blood rheology, platelet reactivity, clotting factors, physical and mechanical properties of the stent and from the effects of these different factors on the fluid dynamics of blood flow. Since the introduction of stents 32 years ago, continuous improvements in our understanding of the pathophysiology of ST have triggered important advances, including new therapies, new technologies and an increased awareness of the implications of implantation techniques. Furthermore, advances in medical imaging and in the mathematical processing of this information have allowed a more detailed assessment of the mechanisms of ST at the time of its onset. Evidence shows that addressing the risk factors for ST leads to a substantial reduction in its incidence, both early and late after stent implantation. A better knowledge of the mechanisms of this complication is, however, necessary to direct the choice of the most appropriate strategy for its prevention and treatment.
Key points
-
Although rare, stent thrombosis remains a major complication after stent implantation, with up to 45% mortality and a recurrence rate as high as 20%.
-
The mechanisms of stent thrombosis are multifactorial, and novel risk factors have been identified.
-
Multiple interactions between device-related factors, patient-related factors and procedure-related factors determine the risk of stent thrombosis at different time.
-
Although apparently complex, these concepts must be understood and applied in routine clinical practice given that their correction is associated with substantial reductions in the rate of stent thrombosis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
MedMarket Diligence. Global dynamics of surgical and interventional cardiovascular procedures, 2015–2022 [report #C500]. (MedMarket Diligence, 2016).
Claessen, B. E. et al. Stent thrombosis: a clinical perspective. JACC Cardiovasc. Interv. 7, 1081–1092 (2014).
Torrado, J. et al. Restenosis, stent thrombosis, and bleeding complications: navigating between Scylla and Charybdis. J. Am. Coll. Cardiol. 71, 1676–1695 (2018).
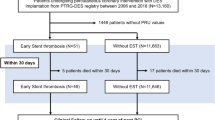
Iakovou, I. et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293, 2126–2130 (2005).
D’Ascenzo, F. et al. Incidence and predictors of coronary stent thrombosis: evidence from an international collaborative meta-analysis including 30 studies, 221,066 patients, and 4276 thromboses. Int. J. Cardiol. 167, 575–584 (2013).
Baber, U. et al. Impact of the everolimus-eluting stent on stent thrombosis: a meta-analysis of 13 randomized trials. J. Am. Coll. Cardiol. 58, 1569–1577 (2011).
Bonaa, K. H. et al. Drug-eluting or bare-metal stents for coronary artery disease. N. Engl. J. Med. 375, 1242–1252 (2016).
Palmerini, T. et al. Long-term safety of drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. J. Am. Coll. Cardiol. 65, 2496–2507 (2015).
Palmerini, T. et al. Clinical outcomes with bioabsorbable polymer- versus durable polymer-based drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. J. Am. Coll. Cardiol. 63, 299–307 (2014).
Toyota, T., Shiomi, H., Morimoto, T. & Kimura, T. Meta-analysis of long-term clinical outcomes of everolimus-eluting stents. Am. J. Cardiol. 116, 187–194 (2015).
Philip, F., Stewart, S. & Southard, J. A. Very late stent thrombosis with second generation drug eluting stents compared to bare metal stents: network meta-analysis of randomized primary percutaneous coronary intervention trials. Catheter. Cardiovasc. Interv. 88, 38–48 (2016).
Valgimigli, M. et al. Standardized classification and framework for reporting, interpreting, and analysing medication non-adherence in cardiovascular clinical trials: a consensus report from the Non-adherence Academic Research Consortium (NARC). Eur. Heart J. https://doi.org/10.1093/eurheartj/ehy377 (2018).
Lemesle, G. et al. Incident myocardial infarction and very late stent thrombosis in outpatients with stable coronary artery disease. J. Am. Coll. Cardiol. 69, 2149–2156 (2017).
Raber, L. et al. Very late coronary stent thrombosis of a newer-generation everolimus-eluting stent compared with early-generation drug-eluting stents: a prospective cohort study. Circulation 125, 1110–1121 (2012).
Kereiakes, D. J. et al. Predictors of death or myocardial infarction, ischaemic-driven revascularisation, and major adverse cardiovascular events following everolimus-eluting or paclitaxel-eluting stent deployment: pooled analysis from the SPIRIT II, III, IV and COMPARE trials. EuroIntervention 7, 74–83 (2011).
Koskinas, K. C. et al. Impact of patient and lesion complexity on long-term outcomes following coronary revascularization with new-generation drug-eluting stents. Am. J. Cardiol. 119, 501–507 (2017).
Park, K. W. et al. Characteristics and predictors of drug-eluting stent thrombosis: results from the multicenter ‘Korea Stent Thrombosis (KoST)’ registry. Circ. J. 75, 1626–1632 (2011).
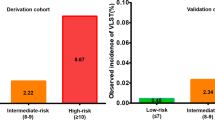
Dangas, G. D. et al. Development and validation of a stent thrombosis risk score in patients with acute coronary syndromes. JACC Cardiovasc. Interv. 5, 1097–1105 (2012).
Baran, K. W. et al. A clinical risk score for the prediction of very late stent thrombosis in drug eluting stent patients. EuroIntervention 6, 949–954 (2011).
Généreux, P. et al. Stent thrombosis and dual antiplatelet therapy interruption with everolimus-eluting stents: insights from the Xience V Coronary Stent System trials. Circ. Cardiovasc. Interv. 8, e001362 (2015).
van Werkum, J. W. et al. Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis registry. J. Am. Coll. Cardiol. 53, 1399–1409 (2009).
Park, K. W. et al. Paraoxonase 1 gene polymorphism does not affect clopidogrel response variability but is associated with clinical outcome after PCI. PLOS ONE 8, e52779 (2013).
Waksman, R. et al. Correlates and outcomes of late and very late drug-eluting stent thrombosis: results from DESERT (international drug-eluting stent event registry of thrombosis). JACC Cardiovasc. Interv. 7, 1093–1102 (2014).
Iqbal, J. et al. Incidence and predictors of stent thrombosis: a single-centre study of 5,833 consecutive patients undergoing coronary artery stenting. EuroIntervention 9, 62–69 (2013).
Choi, H. S. et al. Very late stent thrombosis in a drug-eluting stent due to interruption of anti-platelet agents in patients with acute myocardial infarction and thrombocytosis. Korean Circ. J. 41, 417–420 (2011).
Prech, M., Janus, M., Lukawski, K. & Lesiak, M. Thrombocytosis as a potential cause of a very late stent thrombosis in the left main coronary artery. Kardiol. Pol. 71, 308–309 (2013).
Giustino, G. et al. Relation between platelet count and platelet reactivity to thrombotic and bleeding risk: from the Assessment of Dual Antiplatelet Therapy With Drug-Eluting Stents study. Am. J. Cardiol. 117, 1703–1713 (2016).
Lim, S. et al. Incidence, implications, and predictors of stent thrombosis in acute myocardial infarction. Am. J. Cardiol. 117, 1562–1568 (2016).
Mayer, K. & Sibbing, D. Platelet hyperreactivity and stent thrombosis in patients undergoing coronary stenting. Curr. Vasc. Pharmacol. 10, 597–605 (2012).
Poon, E. K. W. et al. Elevated blood viscosity and microrecirculation resulting from coronary stent malapposition. J. Biomech. Eng. 140, 051006 (2018).
Lee, S. Y. et al. Short-term versus long-term dual antiplatelet therapy after drug-eluting stent implantation in elderly patients: a meta-analysis of individual participant data from 6 randomized trials. JACC Cardiovasc. Interv. 11, 435–443 (2018).
Mehran, R. et al. Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 382, 1714–1722 (2013).
Schulz, S. et al. Stent thrombosis after drug-eluting stent implantation: incidence, timing, and relation to discontinuation of clopidogrel therapy over a 4-year period. Eur. Heart J. 30, 2714–2721 (2009).
Stone, G. W. et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 382, 614–623 (2013).
Naidu, S. S. et al. Contemporary incidence and predictors of stent thrombosis and other major adverse cardiac events in the year after XIENCE V implantation: results from the 8,061-patient XIENCE V United States study. JACC Cardiovasc. Interv. 5, 626–635 (2012).
Valgimigli, M. et al. Should duration of dual antiplatelet therapy depend on the type and/or potency of implanted stent? A pre-specified analysis from the PROlonging Dual antiplatelet treatment after Grading stent-induced Intimal hyperplasia studY (PRODIGY). Eur. Heart J. 34, 909–919 (2013).
Giustino, G. et al. Duration of dual antiplatelet therapy after drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. J. Am. Coll. Cardiol. 65, 1298–1310 (2015).
Varenne, O. et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet 391, 41–50 (2018).
Yeh, R. W. et al. Lesion complexity and outcomes of extended dual antiplatelet therapy after percutaneous coronary intervention. J. Am. Coll. Cardiol. 70, 2213–2223 (2017).
Cuisset, T. et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur. Heart J. 38, 3070–3078 (2017).
Sibbing, D. et al. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. Lancet 390, 1747–1757 (2017).
Capodanno, D., Alberts, M. & Angiolillo, D. J. Antithrombotic therapy for secondary prevention of atherothrombotic events in cerebrovascular disease. Nat. Rev. Cardiol. 13, 609–622 (2016).
Motovska, Z. et al. 1-year outcomes of patients undergoing primary angioplasty for myocardial infarction treated with prasugrel versus ticagrelor. J. Am. Coll. Cardiol. 71, 371–381 (2018).
Koskinas, K. C. et al. Incidence, predictors, and clinical impact of early prasugrel cessation in patients with ST-elevation myocardial infarction. J. Am. Heart Assoc. 7, e008085 (2018).
Bansilal, S. et al. Ticagrelor for secondary prevention of atherothrombotic events in patients with multivessel coronary disease. J. Am. Coll. Cardiol. 71, 489–496 (2018).
Levine, G. N. et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J. Thorac. Cardiovasc. Surg. 152, 1243–1275 (2016).
Valgimigli, M. et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 39, 213–260 (2018).
Costa, F. et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 389, 1025–1034 (2017).
Giustino, G. et al. Efficacy and safety of dual antiplatelet therapy after complex PCI. J. Am. Coll. Cardiol. 68, 1851–1864 (2016).
Lamberts, M. et al. Antithrombotic treatment in patients with heart failure and associated atrial fibrillation and vascular disease: a nationwide cohort study. J. Am. Coll. Cardiol. 63, 2689–2698 (2014).
Agarwal, N. et al. Safety and efficacy of dual versus triple antithrombotic therapy in patients undergoing percutaneous coronary intervention. Am. J. Med. 130, 1280–1289 (2017).
Verdoia, M. et al. Parathyroid hormone levels and high-residual platelet reactivity in patients receiving dual antiplatelet therapy with acetylsalicylic acid and clopidogrel or ticagrelor. Cardiovasc. Ther. 34, 209–215 (2016).
Jatene, T. et al. Frequency of cardiac death and stent thrombosis in patients with chronic obstructive pulmonary disease undergoing percutaneous coronary intervention (from the BASKET-PROVE I and II Trials). Am. J. Cardiol. 119, 14–19 (2017).
Pelliccia, F. et al. Drug-drug interactions between clopidogrel and novel cardiovascular drugs. Eur. J. Pharmacol. 765, 332–336 (2015).
Rollini, F., Franchi, F. & Angiolillo, D. J. Switching P2Y12-receptor inhibitors in patients with coronary artery disease. Nat. Rev. Cardiol. 13, 11–27 (2016).
Vranckx, P., Valgimigli, M. & Heidbuchel, H. The significance of drug-drug and drug-food interactions of oral anticoagulation. Arrhythm. Electrophysiol. Rev. 7, 55–61 (2018).
Schomig, A. et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N. Eng. J. Med. 334, 1084–1089 (1996).
Leon, M. B. et al. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. N. Engl. J. Med. 339, 1665–1671 (1998).
Schatz, R. A. A view of vascular stents. Circulation 79, 445–457 (1989).
Colombo, A. et al. Intracoronary stenting without anticoagulation accomplished with intravascular ultrasound guidance. Circulation 91, 1676–1688 (1995).
Camenzind, E., Steg, P. G. & Wijns, W. Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation 115, 1440–1455; discussion 1455 (2007).
McFadden, E. P. et al. Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet 364, 1519–1521 (2004).
Nakazawa, G. et al. Coronary responses and differential mechanisms of late stent thrombosis attributed to first-generation sirolimus- and paclitaxel-eluting stents. J. Am. Coll. Cardiol. 57, 390–398 (2011).
Curcio, A. et al. Effect of stent coating alone on in vitro vascular smooth muscle cell proliferation and apoptosis. Am. J. Physiol. Heart Circ. Physiol. 286, H902–H908 (2004).
Joner, M. et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J. Am. Coll. Cardiol. 48, 193–202 (2006).
Guagliumi, G. et al. Examination of the in vivo mechanisms of late drug-eluting stent thrombosis: findings from optical coherence tomography and intravascular ultrasound imaging. JACC Cardiovasc. Interv. 5, 12–20 (2012).
Koster, R. et al. Nickel and molybdenum contact allergies in patients with coronary in-stent restenosis. Lancet 356, 1895–1897 (2000).
Torii, S. et al. Acute thrombogenicity of fluoropolymer-coated versus biodegradable and polymer free stents. EuroIntervention https://doi.org/10.4244/EIJ-D-17-00728 (2018).
Otsuka, F. et al. Acute thrombogenicity of a durable polymer everolimus-eluting stent relative to contemporary drug-eluting stents with biodegradable polymer coatings assessed ex vivo in a swine shunt model. JACC Cardiovasc. Interv. 8, 1248–1260 (2015).
Rizas, K. D. & Mehilli, J. Stent polymers: do they make a difference? Circ. Cardiovasc. Interv. 9, e002943 (2016).
Stone, G. W. et al. Everolimus-eluting versus paclitaxel-eluting stents in coronary artery disease. N. Eng. J. Med. 362, 1663–1674 (2010).
Kedhi, E. et al. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet 375, 201–209 (2010).
Palmerini, T. et al. Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet 379, 1393–1402 (2012).
Bangalore, S. et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation 125, 2873–2891 (2012).
Bangalore, S. et al. Bare metal stents, durable polymer drug eluting stents, and biodegradable polymer drug eluting stents for coronary artery disease: mixed treatment comparison meta-analysis. BMJ 347, f6625 (2013).
Valgimigli, M. et al. Effects of cobalt-chromium everolimus eluting stents or bare metal stent on fatal and non-fatal cardiovascular events: patient level meta-analysis. BMJ 349, g6427 (2014).
Kang, S. H. et al. Biodegradable-polymer drug-eluting stents versus bare metal stents versus durable-polymer drug-eluting stents: a systematic review and Bayesian approach network meta-analysis. Eur. Heart J. 35, 1147–1158 (2014).
Radu, M. D. et al. Coronary evaginations are associated with positive vessel remodelling and are nearly absent following implantation of newer-generation drug-eluting stents: an optical coherence tomography and intravascular ultrasound study. Eur. Heart J. 35, 795–807 (2014).
Valgimigli, M. et al. Zotarolimus-eluting versus bare-metal stents in uncertain drug-eluting stent candidates. J. Am. Coll. Cardiol. 65, 805–815 (2015).
Windecker, S. et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) — developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur. Heart J. 35, 2541–2619 (2014).
Serruys, P. W. et al. Improved safety and reduction in stent thrombosis associated with biodegradable polymer-based biolimus-eluting stents versus durable polymer-based sirolimus-eluting stents in patients with coronary artery disease: final 5-year report of the LEADERS (limus eluted from a durable versus erodable stent coating) randomized, noninferiority trial. JACC Cardiovasc. Interv. 6, 777–789 (2013).
de Winter, R. J. et al. A sirolimus-eluting bioabsorbable polymer-coated stent (MiStent) versus an everolimus-eluting durable polymer stent (Xience) after percutaneous coronary intervention (DESSOLVE III): a randomised, single-blind, multicentre, non-inferiority, phase 3 trial. Lancet 391, 431–440 (2018).
Gao, K. et al. Efficacy and safety of polymer-free stent versus polymer-permanent drug-eluting stent in patients with acute coronary syndrome: a meta-analysis of randomized control trials. BMC Cardiovasc. Disord. 17, 194 (2017).
Vlachojannis, G. J. et al. Biodegradable polymer biolimus-eluting stents versus durable polymer everolimus-eluting stents in patients with coronary artery disease: final 5-year report from the COMPARE II trial (abluminal biodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent). JACC Cardiovasc. Interv. 10, 1215–1221 (2017).
Kereiakes, D. J. et al. Efficacy and safety of a novel bioabsorbable polymer-coated, everolimus-eluting coronary stent: the EVOLVE II randomized trial. Circ. Cardiovasc. Interv. 8, e002372 (2015).
Jensen, L. O. et al. Randomized comparison of a biodegradable polymer ultrathin strut sirolimus-eluting stent with a biodegradable polymer biolimus-eluting stent in patients treated with percutaneous coronary intervention: the SORT OUT VII trial. Circ. Cardiovasc. Interv. 9, e003610 (2016).
Windecker, S. et al. Comparison of a novel biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: results of the randomized BIOFLOW-II trial. JACC Cardiovasc. Interv. 11, 7 (2018).
Lefevre, T. et al. Comparison of a novel biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: 5-year outcomes of the randomized BIOFLOW-II trial. JACC Cardiovasc. Interv. 11, 995–1002 (2018).
Giustino, G. & Mehran, R. Role of new sirolimus self-apposing stent in coronary interventions. Minerva Cardioangiol. 63, 45–57 (2015).
Koch, K. T. et al. One-year clinical outcomes of the STENTYS self-apposing coronary stent in patients presenting with ST-segment elevation myocardial infarction: results from the APPOSITION III registry. EuroIntervention 11, 264–271 (2015).
Indolfi, C., De Rosa, S. & Colombo, A. Bioresorbable vascular scaffolds - basic concepts and clinical outcome. Nat. Rev. Cardiol. 13, 719–729 (2016).
Ali, Z. A. et al. Three-year outcomes with the absorb bioresorbable scaffold: individual-patient-data meta-analysis from the ABSORB randomized trials. Circulation 137, 464–479 (2018).
Ali, Z. A. et al. 2-year outcomes with the Absorb bioresorbable scaffold for treatment of coronary artery disease: a systematic review and meta-analysis of seven randomised trials with an individual patient data substudy. Lancet 390, 760–772 (2017).
Kereiakes, D. J. et al. 3-year clinical outcomes with everolimus-eluting bioresorbable coronary scaffolds: the ABSORB III trial. J. Am. Coll. Cardiol. 70, 2852–2862 (2017).
Stone, G. W. et al. 1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease: a patient-level, pooled meta-analysis. Lancet 387, 1277–1289 (2016).
Chevalier, B. et al. Four-year follow-up of the randomised comparison between an everolimus-eluting bioresorbable scaffold and an everolimus-eluting metallic stent for the treatment of coronary artery stenosis (ABSORB II Trial). EuroIntervention 13, 1561–1564 (2018).
Serruys, P. W. et al. Comparison of an everolimus-eluting bioresorbable scaffold with an everolimus-eluting metallic stent for the treatment of coronary artery stenosis (ABSORB II): a 3 year, randomised, controlled, single-blind, multicentre clinical trial. Lancet 388, 2479–2491 (2016).
Wykrzykowska, J. J. et al. Bioresorbable scaffolds versus metallic stents in routine PCI. N. Eng. J. Med. 376, 2319–2328 (2017).
Polimeni, A. et al. Long-term outcome of bioresorbable vascular scaffolds for the treatment of coronary artery disease: a meta-analysis of RCTs. BMC Cardiovasc. Disord. 17, 147 (2017).
Sorrentino, S. et al. Everolimus-eluting bioresorbable scaffolds versus everolimus-eluting metallic stents. J. Am. Coll. Cardiol. 69, 3055–3066 (2017).
Collet, C. et al. Early, late and very late incidence of bioresorbable scaffold thrombosis: a systematic review and meta-analysis of randomized clinical trials and observational studies. Minerva Cardioangiol. 65, 32–51 (2017).
Mukete, B. N. et al. Safety and efficacy of everolimus-eluting bioresorbable vascular scaffolds versus durable polymer everolimus-eluting metallic stents assessed at 1-year follow-up: a systematic review and meta-analysis of studies. Int. J. Cardiol. 221, 1087–1094 (2016).
Haude, M. et al. Sustained safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de novo coronary lesions: 12-month clinical results and angiographic findings of the BIOSOLVE-II first-in-man trial. Eur. Heart J. 37, 2701–2709 (2016).
Kolandaivelu, K. et al. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation 123, 1400–1409 (2011).
Genereux, P. et al. Angiographic predictors of 2-year stent thrombosis in patients receiving drug-eluting stents: insights from the ADAPT-DES study. Catheter. Cardiovasc. Interv. 89, 26–35 (2017).
Nakatani, S. et al. Initial findings of impact of strut width on stent coverage and apposition of sirolimus-eluting stents assessed by optical coherence tomography. Catheter. Cardiovasc. Interv. 81, 776–781 (2013).
Prati, F. et al. Clinical impact of OCT findings during PCI: the CLI-OPCI II study. JACC Cardiovasc. Imaging 8, 1297–1305 (2015).
Fujii, K. et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J. Am. Coll. Cardiol. 45, 995–998 (2005).
Ali, Z. A. et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet 388, 2618–2628 (2016).
Souteyrand, G. et al. Mechanisms of stent thrombosis analysed by optical coherence tomography: insights from the national PESTO French registry. Eur. Heart J. 37, 1208–1216 (2016).
Adriaenssens, T. et al. Optical coherence tomography findings in patients with coronary stent thrombosis: a report of the PRESTIGE consortium (prevention of late stent thrombosis by an interdisciplinary global european effort). Circulation 136, 1007–1021 (2017).
Otsuka, F. et al. Neoatherosclerosis: overview of histopathologic findings and implications for intravascular imaging assessment. Eur. Heart J. 36, 2147–2159 (2015).
Yamaji, K. et al. Mechanisms of very late bioresorbable scaffold thrombosis: the INVEST registry. J. Am. Coll. Cardiol. 70, 2330–2344 (2017).
Costa, J. R. Jr. et al. Incidence and predictors of very late (>or = 4 years) major cardiac adverse events in the DESIRE (drug-eluting stents in the real world)-late registry. JACC Cardiovasc. Interv. 3, 12–18 (2010).
Kitahara, H. et al. Impact of stent size selection on acute and long-term outcomes after drug-eluting stent implantation in de novo coronary lesions. Circ. Cardiovasc. Interv. 10, e004795 (2017).
Puricel, S. et al. Bioresorbable coronary scaffold thrombosis: multicenter comprehensive analysis of clinical presentation, mechanisms, and predictors. J. Am. Coll. Cardiol. 67, 921–931 (2016).
Kawamoto, H. et al. Impact of strut width in periprocedural myocardial infarction: a propensity-matched comparison between bioresorbable scaffolds and the first-generation sirolimus-eluting stent. JACC Cardiovasc. Interv. 8, 900–909 (2015).
Gori, T. et al. Characteristics, predictors, and mechanisms of thrombosis in coronary bioresorbable scaffolds: differences between early and late events. JACC Cardiovasc. Interv. 10, 2363–2371 (2017).
Taniwaki, M. et al. Mechanisms of very late drug-eluting stent thrombosis assessed by optical coherence tomography. Circulation 133, 650–660 (2016).
Agrawal, M., Hakeem, A., Ahmed, Z. & Uretsky, B. F. Classification of mechanisms of strut malapposition after angiographically optimized stent implantation: an optical coherence tomography study. Catheter. Cardiovasc. Interv. 90, 225–232 (2017).
Romagnoli, E. et al. Role of residual acute stent malapposition in percutaneous coronary interventions. Catheter. Cardiovasc. Interv. 90, 566–575 (2017).
Prati, F. et al. Long-term consequences of optical coherence tomography findings during percutaneous coronary intervention: the Centro Per La Lotta Contro L’infarto — optimization of percutaneous coronary intervention (CLI-OPCI) late study. EuroIntervention 14, e443–e451 (2018).
Virmani, R. et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation 109, 701–705 (2004).
Hassan, A. K. et al. Late stent malapposition risk is higher after drug-eluting stent compared with bare-metal stent implantation and associates with late stent thrombosis. Eur. Heart J. 31, 1172–1180 (2010).
Chesnutt, J. K. & Han, H. C. Computational simulation of platelet interactions in the initiation of stent thrombosis due to stent malapposition. Phys. Biol. 13, 016001 (2016).
Cuculi, F. et al. Optical coherence tomography findings in bioresorbable vascular scaffolds thrombosis. Circ. Cardiovasc. Interv. 8, e002518 (2015).
Biondi-Zoccai, G. G. et al. Incidence, predictors, and outcomes of coronary dissections left untreated after drug-eluting stent implantation. Eur. Heart J. 27, 540–546 (2006).
Soeda, T. et al. Incidence and clinical significance of poststent optical coherence tomography findings: one-year follow-up study from a multicenter registry. Circulation 132, 1020–1029 (2015).
Choi, S. Y. et al. Intravascular ultrasound findings of early stent thrombosis after primary percutaneous intervention in acute myocardial infarction: a Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) substudy. Circ. Cardiovasc. Interv. 4, 239–247 (2011).
Won, H. et al. Optical coherence tomography derived cut-off value of uncovered stent struts to predict adverse clinical outcomes after drug-eluting stent implantation. Int. J. Cardiovasc. Imaging 29, 1255–1263 (2013).
Lee, S. Y. et al. Early strut coverage in patients receiving drug-eluting stents and its implications for dual antiplatelet therapy: a randomized trial. JACC Cardiovasc. Imaging https://doi.org/10.1016/j.jcmg.2017.12.014 (2018).
Radu, M. D. et al. Flow disturbances in stent-related coronary evaginations: a computational fluid-dynamic simulation study. EuroIntervention 10, 113–123 (2014).
Gori, T. et al. Coronary evaginations and peri-scaffold aneurysms following implantation of bioresorbable scaffolds: incidence, outcome, and optical coherence tomography analysis of possible mechanisms. Eur. Heart J. 37, 2040–2049 (2016).
Gutierrez-Chico, J. L. et al. Differences in neointimal thickness between the adluminal and the abluminal sides of malapposed and side-branch struts in a polylactide bioresorbable scaffold: evidence in vivo about the abluminal healing process. JACC Cardiovasc. Interv. 5, 428–435 (2012).
Cubero-Gallego, H. et al. Early collapse of a magnesium bioresorbable scaffold. JACC Cardiovasc. Interv. 10, e171–e172 (2017).
Bennett, J. et al. Intraluminal scaffold dismantling: the downside of positive remodeling? J. Am. Coll. Cardiol. 67, 2702–2704 (2016).
Onuma, Y. et al. Incidence and imaging outcomes of acute scaffold disruption and late structural discontinuity after implantation of the absorb Everolimus-Eluting fully bioresorbable vascular scaffold: optical coherence tomography assessment in the ABSORB cohort B trial (a clinical evaluation of the bioabsorbable everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions). JACC Cardiovasc. Interv. 7, 1400–1411 (2014).
Koskinas, K. C., Chatzizisis, Y. S., Antoniadis, A. P. & Giannoglou, G. D. Role of endothelial shear stress in stent restenosis and thrombosis: pathophysiologic mechanisms and implications for clinical translation. J. Am. Coll. Cardiol. 59, 1337–1349 (2012).
Ng, J. et al. Local hemodynamic forces after stenting: implications on restenosis and thrombosis. Arterioscler. Thromb. Vasc. Biol. 37, 2231–2242 (2017).
Gao, L. et al. Incidence and morphological predictors of intrastent coronary thrombus after drug-eluting stent implantation (from a multicenter registry). Am. J. Cardiol. 117, 369–375 (2016).
Finn, A. V. & Otsuka, F. Neoatherosclerosis: a culprit in very late stent thrombosis. Circ. Cardiovasc. Interv. 5, 6–9 (2012).
Kang, S. J. et al. Optical coherence tomographic analysis of in-stent neoatherosclerosis after drug-eluting stent implantation. Circulation 123, 2954–2963 (2011).
Nakazawa, G. et al. The pathology of neoatherosclerosis in human coronary implants bare-metal and drug-eluting stents. J. Am. Coll. Cardiol. 57, 1314–1322 (2011).
Lee, S. Y. et al. Optical coherence tomography-based evaluation of in-stent neoatherosclerosis in lesions with more than 50% neointimal cross-sectional area stenosis. EuroIntervention 9, 945–951 (2013).
Moncada, M. et al. First in human evaluation of the vascular biocompatibility and biomechanical performance of a novel ultra high molecular weight amorphous PLLA bioresorbable scaffold in the absence of anti-proliferative drugs: two-year imaging results in humans. Catheter. Cardiovasc. Interv. https://doi.org/10.1002/ccd.27444 (2017).
Kuramitsu, S. et al. Incidence and clinical impact of stent fracture after everolimus-eluting stent implantation. Circ. Cardiovasc. Interv. 5, 663–671 (2012).
Kan, J. et al. Incidence and clinical outcomes of stent fractures on the basis of 6,555 patients and 16,482 drug-eluting stents from 4 centers. JACC Cardiovasc. Interv. 9, 1115–1123 (2016).
Maehara, A., Matsumura, M., Ali, Z. A., Mintz, G. S. & Stone, G. W. IVUS-guided versus OCT-guided coronary stent implantation: a critical appraisal. JACC Cardiovasc. Imaging 10, 1487–1503 (2017).
Jones, D. A. et al. Angiography alone versus angiography plus optical coherence tomography to guide percutaneous coronary intervention: outcomes from the Pan-London PCI cohort. JACC Cardiovasc. Interv. 11, 1313–1321 (2018).
Hamshere, S. et al. An observational study of clinical outcomes of everolimus-eluting bioresorbable scaffolds comparing the procedural use of optical coherence tomography against angiography alone. Coron. Artery Dis. 29, 482–488 (2018).
Prati, F. et al. Suboptimal stent deployment is associated with subacute stent thrombosis: optical coherence tomography insights from a multicenter matched study — from the CLI Foundation investigators: the CLI-THRO study. Am. Heart J. 169, 249–256 (2015).
Meneveau, N. & Ecarnot, F. Response by Meneveau and Ecarnot to letter regarding article, “Optical coherence tomography to optimize results of percutaneous coronary intervention in patients with non-ST-elevation acute coronary syndrome: results of the multicenter, randomized DOCTORS study (does optical coherence tomography optimize results of stenting)”. Circulation 135, e142–e143 (2017).
Maehara, A. et al. Comparison of stent expansion guided by optical coherence tomography versus intravascular ultrasound: the ILUMIEN II study (observational study of optical coherence tomography [OCT] in patients undergoing fractional flow reserve [FFR] and percutaneous coronary intervention). JACC Cardiovasc. Interv. 8, 1704–1714 (2015).
Kubo, T. et al. Optical frequency domain imaging versus intravascular ultrasound in percutaneous coronary intervention (OPINION trial): one-year angiographic and clinical results. Eur. Heart J. 38, 3139–3147 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03507777 (2018).
Brilakis, E. S. et al. Drug-eluting stents versus bare-metal stents in saphenous vein grafts: a double-blind, randomised trial. Lancet 391, 1997–2007 (2018).
Jeger, R. V. et al. Stent thrombosis after coronary stent implantation: a protective effect of high-dose statin therapy? Cardiology 126, 115–121 (2013).
Ellis, S. G. et al. Clinical, angiographic, and procedural correlates of very late absorb scaffold thrombosis: multistudy registry results. JACC Cardiovasc. Interv. 11, 638–644 (2018).
Pasceri, V. et al. Clinical effects of routine postdilatation of drug-eluting stents. Catheter. Cardiovasc. Interv. 83, 898–904 (2014).
Escaned, J. et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. Eur. Heart J. 38, 3124–3134 (2017).
Wijns, W. et al. Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study. Eur. Heart J. 36, 3346–3355 (2015).
Pilgrim, T. et al. The impact of anemia on long-term clinical outcome in patients undergoing revascularization with the unrestricted use of drug-eluting stents. Circ. Cardiovasc. Interv. 5, 202–210 (2012).
Clemmensen, P. et al. Long-term outcomes for women versus men with unstable angina/non-ST-segment elevation myocardial infarction managed medically without revascularization: insights from the TaRgeted platelet Inhibition to cLarify the Optimal strateGy to medicallY manage Acute Coronary Syndromes trial. Am. Heart J. 170, 695–705 (2015).
Acknowledgements
Reviewer information
Nature Reviews Cardiology thanks S.-J. Park and E. Brilakis for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
T.G., A.P., L.R. and T.A. researched data for the article. T.G., C.I., L.R. and T.M. discussed its content. All the authors wrote the manuscript, and T.G., C.I., L.R., T.A. and T.M. reviewed and edited it before submission.
Corresponding author
Ethics declarations
Competing interests
T.G. received a research grant from Abbott Vascular and speaker’s or consulting fees from Abbott Vascular, AstraZeneca, Biotronik, Braun, Novartis and Stentys. L.R. received research grants from Abbott Vascular, Regeneron and Sanofi, and speaker’s or consultation fees from Abbott Vascular, Amgen, AstraZeneca, Biotronik, CSL Behring, Novartis and Sanofi. T.A. received a research grant from Abbott Vascular and speaker’s or consulting fees from Abbott Vascular. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gori, T., Polimeni, A., Indolfi, C. et al. Predictors of stent thrombosis and their implications for clinical practice. Nat Rev Cardiol 16, 243–256 (2019). https://doi.org/10.1038/s41569-018-0118-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-018-0118-5
This article is cited by
-
Effects of exenatide on coronary stent’s endothelialization in subjects with type 2 diabetes: a randomized controlled trial. The Rebuild study
Cardiovascular Diabetology (2023)
-
The biology of SCUBE
Journal of Biomedical Science (2023)
-
A novel noble metal stent coating reduces in vitro platelet activation and acute in vivo thrombosis formation: a blinded study
Scientific Reports (2023)
-
Acute Intraprocedural Thrombosis After Flow Diverter Stent Implantation: Risk Factors and Relevance of Standard Observation Time for Early Detection and Management
Clinical Neuroradiology (2023)
-
Non-cardiac surgery in patients with coronary artery disease: risk evaluation and periprocedural management
Nature Reviews Cardiology (2021)