Abstract
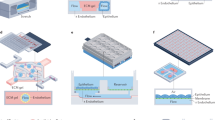
One of the problems that has slowed the development and approval of new anticancer therapies is the lack of preclinical models that can be used to identify key molecular, cellular and biophysical features of human cancer progression. This is because most in vitro cancer models fail to faithfully recapitulate the local tissue and organ microenvironment in which tumours form, which substantially contributes to the complex pathophysiology of the disease. More complex in vitro cancer models have been developed, including transwell cell cultures, spheroids and organoids grown within flexible extracellular matrix gels, which better mimic normal and cancerous tissue development than cells maintained on conventional 2D substrates. But these models still lack the tissue–tissue interfaces, organ-level structures, fluid flows and mechanical cues that cells experience within living organs, and furthermore, it is difficult to collect samples from the different tissue microcompartments. In this Review, we outline how recent developments in microfluidic cell culture technology have led to the generation of human organs-on-chips (also known as organ chips) that are now being used to model cancer cell behaviour within human-relevant tissue and organ microenvironments in vitro. Organ chips enable experimentalists to vary local cellular, molecular, chemical and biophysical parameters in a controlled manner, both individually and in precise combinations, while analysing how they contribute to human cancer formation and progression and responses to therapy. We also discuss the challenges that must be overcome to ensure that organ chip models meet the needs of cancer researchers, drug developers and clinicians interested in personalized medicine.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Day, C. P., Merlino, G. & Van Dyke, T. Preclinical mouse cancer models: a maze of opportunities and challenges. Cell 163, 39–53 (2015).
Gould, S. E., Junttila, M. R. & de Sauvage, F. J. Translational value of mouse models in oncology drug development. Nat. Med. 21, 431–439 (2015).
Killion, J. J., Radinsky, R. & Fidler, I. J. Orthotopic models are necessary to predict therapy of transplantable tumors in mice. Cancer Metastasis Rev. 17, 279–284 (1999).
Justus, C. R., Leffler, N., Ruiz-Echevarria, M. & Yang, L. V. In vitro cell migration and invasion assays. J. Vis. Exp. 88, 51046 (2014).
Mehta, G., Hsiao, A. Y., Ingram, M., Luker, G. D. & Takayama, S. Opportunities and challenges for use of tumor spheroids as models to test drug delivery and efficacy. J. Control. Release 164, 192–204 (2012).
Edmondson, R., Broglie, J. J., Adcock, A. F. & Yang, L. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. Assay Drug Dev. Technol. 12, 207–218 (2014).
Hirschhaeuser, F. et al. Multicellular tumor spheroids: an underestimated tool is catching up again. J. Biotechnol. 148, 3–15 (2010).
Guan, P.-P. et al. By activating matrix metalloproteinase-7, shear stress promotes chondrosarcoma cell motility, invasion and lung colonization. Oncotarget 6, 9140–9159 (2015).
Heldin, C.-H., Rubin, K., Pietras, K. & Ostman, A. High interstitial fluid pressure — an obstacle in cancer therapy. Nat. Rev. Cancer 4, 806–813 (2004).
Polacheck, W. J., Charest, J. L. & Kamm, R. D. Interstitial flow influences direction of tumor cell migration through competing mechanisms. Proc. Natl Acad. Sci. USA 108, 11115–11120 (2011).
Ghosh, S. P. et al. Amelioration of radiation-induced hematopoietic and gastrointestinal damage by Ex-RAD(R) in mice. J. Radiat. Res. 53, 526–536 (2012).
Chaudhuri, P. K., Low, B. C. & Lim, C. T. Mechanobiology of tumor growth. Chem. Rev. 118, 6499–6515 (2018).
Drost, J. & Clevers, H. Organoids in cancer research. Nat. Rev. Cancer 18, 407–418 (2018).
Bhadriraju, K. & Chen, C. S. Engineering cellular microenvironments to improve cell-based drug testing. Drug Discov. Today 7, 612–620 (2002).
Bhatia, S. N. & Ingber, D. E. Microfluidic organs-on-chips. Nat. Biotechnol. 32, 760–772 (2014).
Novak, R. et al. Scalable fabrication of stretchable, dual channel, microfluidic organ chips. J. Vis. Exp. 140, e58151 (2018).
Jain, A. et al. Primary human lung alveolus-on-a-chip model of intravascular thrombosis for assessment of therapeutics. Clin. Pharmacol. Ther. 103, 332–340 (2018).
Barrile, R. et al. Organ-on-chip recapitulates thrombosis induced by an anti-CD154 monoclonal antibody: translational potential of advanced microengineered systems. Clin. Pharmacol. Ther. 104, 1240–1248 (2018).
Hassell, B. A. et al. Human organ chip models recapitulate orthotopic lung cancer growth, therapeutic responses, and tumor dormancy in vitro. Cell Rep. 21, 508–516 (2017). This study describes the development of a human lung cancer chip that recapitulates tumour growth, invasion patterns and responses to therapy observed in patients.
Choi, Y. et al. A microengineered pathophysiological model of early-stage breast cancer. Lab Chip 15, 3350–3357 (2015). This study describes the generation of an early-stage breast cancer chip model that can be used to evaluate the efficacy and toxicity of an anticancer drug.
Musah, S. et al. Mature induced-pluripotent-stem-cell-derived human podocytes reconstitute kidney glomerular-capillary-wall function on a chip. Nat. Biomed. Eng. 1, 0069 (2017).
Huh, D. et al. Reconstituting organ-level lung functions on a chip. Science 328, 1662–1668 (2010).
Huh, D. et al. A human disease model of drug toxicity — induced pulmonary edema in a lung-on-a-chip microdevice. Sci. Transl Med. 4, 159ra147 (2012).
Stucki, A. O. et al. A lung-on-a-chip array with an integrated bio-inspired respiration mechanism. Lab Chip 15, 1302–1310 (2015).
Benam, K. H. et al. Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nat. Methods 13, 151–157 (2016).
Benam, K. H. et al. Matched-comparative modeling of normal and diseased human airway responses using a microengineered breathing lung chip. Cell Syst. 3, 456–466 (2016).
Sellgren, K. L., Butala, E. J., Gilmour, B. P., Randell, S. H. & Grego, S. A biomimetic multicellular model of the airways using primary human cells. Lab Chip 14, 3349–3358 (2014).
Jang, K.-J. et al. Human kidney proximal tubule-on-a-chip for drug transport and nephrotoxicity assessment. Integr. Biol. 5, 1119–1129 (2013).
Maschmeyer, I. et al. A four-organ-chip for interconnected long-term co-culture of human intestine, liver, skin and kidney equivalents. Lab Chip 15, 2688–2699 (2015).
Musah, S., Dimitrakakis, N., Camacho, D. M., Church, G. M. & Ingber, D. E. Directed differentiation of human induced pluripotent stem cells into mature kidney podocytes and establishment of a glomerulus chip. Nat. Protoc. 13, 1662–1685 (2018).
Kim, H. J. & Ingber, D. E. Gut-on-a-chip microenvironment induces human intestinal cells to undergo villus differentiation. Integr. Biol. 5, 1130–1140 (2013).
Kasendra, M. et al. Development of a primary human small intestine-on-a-chip using biopsy-derived organoids. Sci. Rep. 8, 2871 (2018).
Esch, M. B., Mahler, G. J., Stokol, T. & Shuler, M. L. Body-on-a-chip simulation with gastrointestinal tract and liver tissues suggests that ingested nanoparticles have the potential to cause liver injury. Lab Chip 14, 3081–3092 (2014).
Li, C. Y. et al. Micropatterned cell–cell interactions enable functional encapsulation of primary hepatocytes in hydrogel microtissues. Tissue Eng. Part A 20, 2200–2212 (2014).
Beckwitt, C. H. et al. Liver ‘organ on a chip’. Exp. Cell Res. 363, 15–25 (2018).
Sieber, S. et al. Bone marrow-on-a-chip: long-term culture of human haematopoietic stem cells in a three-dimensional microfluidic environment. J. Tissue Eng. Regen. Med. 12, 479–489 (2018).
Herland, A. et al. Distinct contributions of astrocytes and pericytes to neuroinflammation identified in a 3D human blood-brain barrier on a chip. PLOS ONE 11, 1–21 (2016).
Adriani, G., Ma, D., Pavesi, A., Kamm, R. D. & Goh, E. L. K. A 3D neurovascular microfluidic model consisting of neurons, astrocytes and cerebral endothelial cells as a blood-brain barrier. Lab Chip 17, 448–459 (2017).
Wang, Y. I., Abaci, H. E. & Shuler, M. L. Microfluidic blood-brain barrier model provides in vivo-like barrier properties for drug permeability screening. Biotechnol. Bioeng. 114, 184–194 (2017).
Kim, H. J., Li, H., Collins, J. J. & Ingber, D. E. Contributions of microbiome and mechanical deformation to intestinal bacterial overgrowth and inflammation in a human gut-on-a-chip. Proc. Natl Acad. Sci. USA 113, E7–E15 (2016).
Jalili-Firoozinezhad, S. et al. Modeling radiation injury-induced cell death and countermeasure drug responses in a human gut-on-a-chip. Cell Death Dis. 9, 223 (2018).
Wang, G. et al. Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies. Nat. Med. 20, 616–623 (2014).
Montanez-Sauri, S. I., Sung, K. E., Berthier, E. & Beebe, D. J. Enabling screening in 3D microenvironments: probing matrix and stromal effects on the morphology and proliferation of T47D breast carcinoma cells. Integr. Biol. 5, 631–640 (2013).
Lang, J. D., Berry, S. M., Powers, G. L., Beebe, D. J. & Alarid, E. T. Hormonally responsive breast cancer cells in a microfluidic co-culture model as a sensor of microenvironmental activity. Integr. Biol. 5, 807–816 (2013).
Regier, M. C. et al. Transitions from mono- to co- to tri-culture uniquely affect gene expression in breast cancer, stromal, and immune compartments. Biomed. Microdevices 18, 70 (2016).
Folkman, J., Watson, K., Ingber, D. & Hanahan, D. Induction of angiogenesis during the transition from hyperplasia to neoplasia. Nature 339, 58–61 (1989).
Nguyen, D.-H. T. et al. Biomimetic model to reconstitute angiogenic sprouting morphogenesis in vitro. Proc. Natl Acad. Sci. USA 110, 6712–6717 (2013). This paper describes how angiogenic sprouting can be replicated in a microfluidic device and how this model enables the investigation of the effects of angiogenic inhibitors on sprouting morphogenesis.
Chen, M. B., Whisler, J. A., Jeon, J. S. & Kamm, R. D. Mechanisms of tumor cell extravasation in an in vitro microvascular network platform. Integr. Biol. 5, 1262–1271 (2013).
Moya, M. L., Hsu, Y.-H., Lee, A. P., Hughes, C. C. W. & George, S. C. In vitro perfused human capillary networks. Tissue Eng. Part C 19, 730–737 (2013).
Bischel, L. L., Young, E. W. K., Mader, B. R. & Beebe, D. J. Tubeless microfluidic angiogenesis assay with three-dimensional endothelial-lined microvessels. Biomaterials 34, 1471–1477 (2013).
Baker, B. M., Trappmann, B., Stapleton, S. C., Toro, E. & Chen, C. S. Microfluidics embedded within extracellular matrix to define vascular architectures and pattern diffusive gradients. Lab Chip 13, 3246 (2013).
Wang, X. et al. Engineering anastomosis between living capillary networks and endothelial cell-lined microfluidic channels. Lab Chip 16, 282–290 (2016).
Kim, S., Lee, H., Chung, M. & Jeon, N. L. Engineering of functional, perfusable 3D microvascular networks on a chip. Lab Chip 13, 1489–1500 (2013).
Miller, C. P., Tsuchida, C., Zheng, Y., Himmelfarb, J. & Akilesh, S. A. 3D human renal cell carcinoma-on-a-chip for the study of tumor angiogenesis. Neoplasia 20, 610–620 (2018).
Wu, X., Newbold, M. A. & Haynes, C. L. Recapitulation of in vivo-like neutrophil transendothelial migration using a microfluidic platform. Analyst 140, 5055–5064 (2015).
Wu, X., Newbold, M. A., Gao, Z. & Haynes, C. L. A versatile microfluidic platform for the study of cellular interactions between endothelial cells and neutrophils. Biochim. Biophys. Acta Gen. Subj. 1861, 1122–1130 (2017).
Hsu, Y.-H., Moya, M. L., Hughes, C. C. W., George, S. C. & Lee, A. P. A microfluidic platform for generating large-scale nearly identical human microphysiological vascularized tissue arrays. Lab Chip 13, 2990–2998 (2013). This study presents a microfluidic model for tissue arrays with interconnected vascular networks.
Jeon, J. S., Zervantonakis, I. K., Chung, S., Kamm, R. D. & Charest, J. L. In vitro model of tumor cell extravasation. PLOS ONE 8, e56910 (2013).
Jeon, J. S. et al. Human 3D vascularized organotypic microfluidic assays to study breast cancer cell extravasation. Proc. Natl Acad. Sci. USA 112, 214–219 (2015). This study develops a vascularized microfluidic assay to study breast cancer extravasation into different organ microenvironments.
Chen, M. B., Lamar, J. M., Li, R., Hynes, R. O. & Kamm, R. D. Elucidation of the roles of tumor integrin β1 in the extravasation stage of the metastasis cascade. Cancer Res. 76, 2513–2524 (2016).
Gilardi, M. et al. The key role of talin-1 in cancer cell extravasation dissected through human vascularized 3D microfluidic model [PO-12]. Thromb. Res. 140 (Suppl), S180–S181 (2016).
Chen, M. B. et al. On-chip human microvasculature assay for visualization and quantification of tumor cell extravasation dynamics. Nat. Protoc. 12, 865–880 (2017).
Lee, J.-H. et al. Microfluidic co-culture of pancreatic tumor spheroids with stellate cells as a novel 3D model for investigation of stroma-mediated cell motility and drug resistance. J. Exp. Clin. Cancer Res. 37, 4 (2018).
Jeong, S.-Y., Lee, J.-H., Shin, Y., Chung, S. & Kuh, H.-J. Co-culture of tumor spheroids and fibroblasts in a collagen matrix-incorporated microfluidic chip mimics reciprocal activation in solid tumor microenvironment. PLOS ONE 11, e0159013 (2016).
Rizvi, I. et al. Flow induces epithelial-mesenchymal transition, cellular heterogeneity and biomarker modulation in 3D ovarian cancer nodules. Proc. Natl Acad. Sci. USA 110, E1974–E1983 (2013).
Sung, K. E. et al. Transition to invasion in breast cancer: a microfluidic in vitro model enables examination of spatial and temporal effects. Integr. Biol. 3, 439–450 (2011).
Ramaswamy, S., Ross, K. N., Lander, E. S. & Golub, T. R. A molecular signature of metastasis in primary solid tumors. Nat. Genet. 33, 49–54 (2003).
Hsu, T. H. et al. Analysis of the paracrine loop between cancer cells and fibroblasts using a microfluidic chip. Lab Chip 11, 1808–1814 (2011).
Li, R. et al. Macrophage-secreted TNFα and TGFβ1 influence migration speed and persistence of cancer cells in 3D tissue culture via independent pathways. Cancer Res. 77, 279–290 (2017).
Erdogan, B. et al. Cancer-associated fibroblasts promote directional cancer cell migration by aligning fibronectin. J. Cell Biol. 216, 3799–3816 (2017).
Wang, S. et al. Study on invadopodia formation for lung carcinoma invasion with a microfluidic 3D culture device. PLOS ONE 8, e56448 (2013).
Huang, C. P. et al. Engineering microscale cellular niches for three-dimensional multicellular co-cultures. Lab Chip 9, 1740–1748 (2009).
Bai, J. et al. Contact-dependent carcinoma aggregate dispersion by M2a macrophages via ICAM-1 and β2 integrin interactions. Oncotarget 6, 25295–25307 (2015).
Ao, M. et al. Stretching fibroblasts remodels fibronectin and alters cancer cell migration. Sci. Rep. 5, 8334 (2015).
Zervantonakis, I. K. et al. Three-dimensional microfluidic model for tumor cell intravasation and endothelial barrier function. Proc. Natl Acad. Sci. USA 109, 13515–13520 (2012).
Reymond, N., D’Água, B. B. & Ridley, A. J. Crossing the endothelial barrier during metastasis. Nat. Rev. Cancer 13, 858–870 (2013).
Tang, Y. et al. A biomimetic microfluidic tumor microenvironment platform mimicking the EPR effect for rapid screening of drug delivery systems. Sci. Rep. 7, 9359 (2017).
Sun, Y. et al. CXCL12-CXCR4 axis promotes the natural selection of breast cancer cell metastasis. Tumour Biol. 35, 7765–7773 (2014).
Song, J. W. et al. Microfluidic endothelium for studying the intravascular adhesion of metastatic breast cancer cells. PLOS ONE 4, e5756 (2009).
Regmi, S., Fu, A. & Luo, K. Q. High shear stresses under exercise condition destroy circulating tumor cells in a microfluidic system. Sci. Rep. 7, 39975 (2017).
Boussommier-Calleja, A. et al. The effects of monocytes on tumor cell extravasation in a 3D vascularized microfluidic model. Biomaterials https://doi.org/10.1016/j.biomaterials.2018.03.005 (2018).
Yousem, S. A & Beasley, M. B. Bronchioloalveolar carcinoma: a review of current concepts and evolving issues. Arch. Pathol. Lab. Med. 131, 1027–1032 (2007).
Abe, M. Targeting the interplay between myeloma cells and the bone marrow microenvironment in myeloma. Int. J. Hematol. 94, 334–343 (2011).
Zhang, W., Lee, W. Y., Siegel, D. S., Tolias, P. & Zilberberg, J. Patient-specific 3D microfluidic tissue model for multiple myeloma. Tissue Eng. Part C 20, 663–670 (2014).
Pak, C. et al. MicroC(3): an ex vivo microfluidic cis-coculture assay to test chemosensitivity and resistance of patient multiple myeloma cells. Integr. Biol. 7, 643–654 (2015).
Macedo, F. et al. Bone metastases: an overview. Oncol. Rev. 11, 321 (2017).
Bersini, S. et al. A microfluidic 3D in vitro model for specificity of breast cancer metastasis to bone. Biomaterials 35, 2454–2461 (2014). This study uses a microfluidic plattform to investigate the specificity of human breast cancer metastasis to the bone revealing the involvement of breast cancer cell receptor CXCR2 and the bone-secreted chemokine CXCL5 in cancer cell extravasation.
Mastro, A. M. & Vogler, E. A. A three-dimensional osteogenic tissue model for the study of metastatic tumor cell interactions with bone. Cancer Res. 69, 4097–4100 (2009).
Krishnan, V., Vogler, E. A., Sosnoski, D. M. & Mastro, A. M. In vitro mimics of bone remodeling and the vicious cycle of cancer in bone. J. Cell. Physiol. 229, 453–462 (2014).
Talukdar, S. & Kundu, S. C. Engineered 3D silk-based metastasis models: Interactions between human breast adenocarcinoma, mesenchymal stem cells and osteoblast-like cells. Adv. Funct. Mater. 23, 5249–5260 (2013).
Xu, H. et al. A dynamic in vivo-like organotypic blood-brain barrier model to probe metastatic brain tumors. Sci. Rep. 6, 36670 (2016).
Chen, Y. A. et al. Generation of oxygen gradients in microfluidic devices for cell culture using spatially confined chemical reactions. Lab Chip 11, 3626–3633 (2011).
Ying, L. et al. Cancer associated fibroblast-derived hepatocyte growth factor inhibits the paclitaxel-induced apoptosis of lung cancer A549 cells by up-regulating the PI3K/Akt and GRP78 signaling on a microfluidic platform. PLOS ONE 10, 1–15 (2015).
Faley, S. L. et al. Microfluidic single cell arrays to interrogate signalling dynamics of individual, patient-derived hematopoietic stem cells. Lab Chip 9, 2659–2664 (2009).
Xu, Z. et al. Application of a microfluidic chip-based 3D co-culture to test drug sensitivity for individualized treatment of lung cancer. Biomaterials 34, 4109–4117 (2013).
Bai, J., Tu, T.-Y., Kim, C., Thiery, J. P. & Kamm, R. D. Identification of drugs as single agents or in combination to prevent carcinoma dissemination in a microfluidic 3D environment. Oncotarget 6, 36603–36614 (2015).
Sobrino, A. et al. 3D microtumors in vitro supported by perfused vascular networks. Sci. Rep. 6, 31589 (2016). This study uses a microfluidic platform with vascularized microtumours to reveal that dual target angiogenesis inhibitors are more effective to regress the vasculature than single target inhibitors.
Walsh, C. L. et al. A multipurpose microfluidic device designed to mimic microenvironment gradients and develop targeted cancer therapeutics. Lab Chip 9, 545–554 (2009).
Pavesi, A. et al. Engineering a 3D microfluidic culture platform for tumor-treating field application. Sci. Rep. 6, 26584 (2016).
Jarvis, M. et al. Microfluidic co-culture devices to assess penetration of nanoparticles into cancer cell mass. Bioeng. Transl Med. 2, 268–277 (2017).
Terrell-Hall, T. B., Nounou, M. I., El-Amrawy, F., Griffith, J. I. G. & Lockman, P. R. Trastuzumab distribution in an in-vivo and in-vitro model of brain metastases of breast cancer. Oncotarget 8, 83734–83744 (2017).
Pavesi, A. et al. A 3D microfluidic model for preclinical evaluation of TCR-engineered T cells against solid tumors. JCI Insight 2, 89762 (2017). This study describes the development of a microdevice platform that enables the investigation of factors that can alter antitumour efficacy of adoptive T cell function in 3D.
Lee, S. W. L. et al. Characterizing the role of monocytes in T cell cancer immunotherapy using a 3D microfluidic model. Front. Immunol. 9, 416 (2018).
Joyce, J. A. & Fearon, D. T. T cell exclusion, immune privilege, and the tumor microenvironment. Science 348, 74–80 (2015).
Prantil-Baun, R. et al. Physiologically based pharmacokinetic and pharmacodynamic analysis enabled by microfluidically linked organs-on-chips. Annu. Rev. Pharmacol. Toxicol. 58, 37–64 (2018).
Zhang, B. & Radisic, M. Organ-on-a-chip devices advance to market. Lab Chip 17, 2395–2420 (2017).
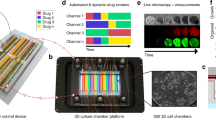
Lanz, H. L. et al. Therapy response testing of breast cancer in a 3D high-throughput perfused microfluidic platform. BMC Cancer 17, 709 (2017).
Holton, A. B. et al. Microfluidic biopsy trapping device for the real-time monitoring of tumor microenvironment. PLOS ONE 12, e0169797 (2017).
Domansky, K. et al. Clear castable polyurethane elastomer for fabrication of microfluidic devices. Lab Chip 13, 3956–3964 (2013).
Domansky, K. et al. SEBS elastomers for fabrication of microfluidic devices with reduced drug absorption by injection molding and extrusion. Microfluid. Nanofluid. 21, 107 (2017).
van Midwoud, P. M., Janse, A., Merema, M. T., Groothuis, G. M. M. & Verpoorte, E. Comparison of biocompatibility and adsorption properties of different plastics for advanced microfluidic cell and tissue culture models. Anal. Chem. 84, 3938–3944 (2012).
Homan, K. A. et al. Bioprinting of 3D convoluted renal proximal tubules on perfusable chips. Sci. Rep. 6, 34845 (2016).
Marx, U. et al. Biology-inspired microphysiological system approaches to solve the prediction dilemma of substance testing. ALTEX 33, 272–321 (2016).
Skardal, A., Shupe, T. & Atala, A. Organoid-on-a-chip and body-on-a-chip systems for drug screening and disease modeling. Drug Discov. Today 21, 1399–1411 (2016).
Edington, C. D. et al. Interconnected microphysiological systems for quantitative biology and pharmacology studies. Sci. Rep. 8, 4530 (2018).
Oleaga, C. et al. Multi-organ toxicity demonstration in a functional human in vitro system composed of four organs. Sci. Rep. 6, 20030 (2016).
Vernetti, L. et al. Functional coupling of human microphysiology systems: intestine, liver, kidney proximal tubule, blood-brain barrier and skeletal muscle. Sci. Rep. 7, 42296 (2017).
Lee, H. et al. A pumpless multi-organ-on-a-chip (MOC) combined with a pharmacokinetic-pharmacodynamic (PK-PD) model. Biotechnol. Bioeng. 114, 432–443 (2016).
Sung, J. H., Kam, C. & Shuler, M. L. A microfluidic device for a pharmacokinetic-pharmacodynamic (PK-PD) model on a chip. Lab Chip 10, 446–455 (2010).
Eduati, F. et al. A microfluidics platform for combinatorial drug screening on cancer biopsies. Nat. Commun. 9, 2434 (2018).
Acknowledgements
This work was supported by the Wyss Institute for Biologically Inspired Engineering at Harvard University and Defense Advanced Research Projects Agency (DARPA) under Cooperative Agreement Number W911NF-12-2-0036. The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of DARPA or the US Government.
Author information
Authors and Affiliations
Contributions
Both A.S.-P. and B.A.H. researched and compiled the data from the literature and drafted a first draft of the manuscript. D.E.I. edited and revised the manuscript, working with the other authors.
Corresponding author
Ethics declarations
Competing interests
D.E.I. is a founder of, holds equity in and chairs the scientific advisory board of Emulate Inc. A.S.-P. and B.A.H. declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Matrigel
-
A commercial product containing an extracellular matrix hydrogel composed of tumour-derived basement membrane proteins used for cell culture.
- Fluid shear stress
-
Physical drag forces created by fluid flow parallel to the surface of a material, such as the apical membrane of the endothelium in a blood vessel.
- Hydrostatic pressure
-
Pressure exerted by a fluid owing to gravity, a pressurized reservoir, pump or centrifugal force.
- Peristaltic deformations
-
Cyclic muscular contractions and relaxations within the wall of an organ, such as the intestine.
- Barth syndrome
-
A rare genetic disorder characterized by weakened heart and muscles, low white blood cell count and short statue.
- Chronic obstructive pulmonary disease
-
A chronic inflammatory lung disease involving chronic bronchitis and/or emphysema that causes obstructed airflow in the lungs, resulting in difficulties in breathing.
- Epithelial–mesenchymal transition
-
(EMT). A process in which epithelial cells take on a mesenchymal phenotype and lose their polarity and cell–cell contacts, which is associated with increased migratory and invasive capacity.
- Matrix metalloproteinases
-
Enzymes that degrade extracellular matrix.
- Minimal residual disease
-
The few surviving tumour cells that remain in tissues after complete remission is achieved through a successful therapeutic intervention; these cells are thought to be responsible for relapse of cancer.
- Sacrificial materials
-
Substances that are deposited within other materials to form a solid gel and can later be solubilized to create hollow compartments, such as microfluidic channels, within a structure.
- Arteriovenous malformation
-
An abnormal connection between blood vessels mainly in the brain or spine disrupting normal blood flow and oxygen circulation.
- Laminar flow
-
A flow regime in which fluid flows in parallel layers with no disruption between the layers and a constant velocity at any point in the fluid.
- Pneumatic micro-valves
-
Air controlled valves at the micrometre scale for the regulation of system pressure, as well as the control of flow rate and direction.
- Invadopodia
-
Dynamic actin-rich cell membrane protrusions that can be associated with cancer cell invasion.
- M2A macrophages
-
A subpopulation of alternatively activated macrophages that are associated with a T helper 2 cell immune response and are induced as a result of stimulation by the cytokines interleukin-4 (IL-4) and IL-13 or during fungal and helminth infections.
- Endosteal surface
-
A layer covering the endosteum, which is a thin membranous tissue containing bone stem cells, blood vessels and connective tissue fibres that coats the inside of long bones and surrounds the bone marrow-filled medullary cavity.
Rights and permissions
About this article
Cite this article
Sontheimer-Phelps, A., Hassell, B.A. & Ingber, D.E. Modelling cancer in microfluidic human organs-on-chips. Nat Rev Cancer 19, 65–81 (2019). https://doi.org/10.1038/s41568-018-0104-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41568-018-0104-6
This article is cited by
-
Application status and optimization suggestions of tumor organoids and CAR-T cell co-culture models
Cancer Cell International (2024)
-
Vascular network-inspired fluidic system (VasFluidics) with spatially functionalizable membranous walls
Nature Communications (2024)
-
Organoids in virology
npj Viruses (2024)
-
YAP/TEAD involvement in resistance to paclitaxel chemotherapy in lung cancer
Molecular and Cellular Biochemistry (2024)
-
Vascularized tumor models for the evaluation of drug delivery systems: a paradigm shift
Drug Delivery and Translational Research (2024)