Abstract
Women are disproportionately affected by sexually transmitted infections (STIs) throughout life. In addition to their high prevalence in women, STIs have debilitating effects on female reproductive health due to female urogenital anatomy, socio-cultural and economic factors. In this Review, we discuss the prevalence and impact of non-HIV bacterial, viral and parasitic STIs on the reproductive and sexual health of cisgender women worldwide. We analyse factors affecting STI prevalence among transgender women and women in low-income settings, and describe the specific challenges and barriers to improved sexual health faced by these population groups. We also synthesize the latest advances in diagnosis, treatment and prevention of STIs.
Similar content being viewed by others
Main
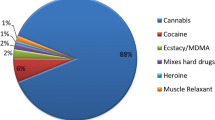
Sexually transmitted infections (STIs) cause reproductive morbidity worldwide. In 2019, the World Health Organization (WHO) estimated that there were 376 million new episodes of chlamydia, gonorrhoea, syphilis and trichomoniasis (Fig. 1)1. In 2019, the United States Centers for Disease Control and Prevention (CDC) reported a nearly 30% increase in chlamydia, gonorrhoea and syphilis between 2015–2019 and a rising incidence of all STIs for the sixth consecutive year2. In the United States in 2018, several STIs were estimated to be more prevalent among women than men, including gonorrhoea, chlamydia and trichomoniasis3. Women often experience complications from STIs, including infertility and chronic pelvic pain, that can have lifelong impact4. STIs can increase peripartum morbidity and mortality in both industrialized areas and in rural and underserved areas of developed countries.
The larger impact of STIs in women compared with men is in part due to the female anatomy (Fig. 2). A woman’s urogenital anatomy is more exposed and vulnerable to STIs compared with the male urogenital anatomy, particularly because the vaginal mucosa is thin, delicate and easily penetrated by infectious agents5. The cervix at the distal end of the vagina leads to the upper genital tract including the uterus, endometrium, fallopian tubes and ovaries. STIs can produce a variety of symptoms and effects at different parts of the female reproductive tract, including genital ulcer disease, vaginitis, pelvic inflammatory disease (PID) and infertility6.
STIs can affect genital and extragenital sites in women. Gonorrhoea and chlamydia typically present as cervicitis. Bacterial vaginosis (BV) and trichomoniasis can also cause cervicitis, but more commonly manifest as vaginitis. HSV and HPV most typically affect the vulva or external genitalia of women.
In this Review, we focus on the impact of non-HIV bacterial, viral and parasitic STIs on the sexual and reproductive health of cisgender women (Table 1). We discuss adverse outcomes of STIs, treatment and prevention, including vaccine development. STIs in transgender women (TGW) are discussed in brief because an exhaustive review of STIs in this population has recently been published7,8. We do not review developments in HIV prevention or treatments in women and refer readers to reviews published elsewhere9,10,11,12,13. Hepatitis B was also excluded as it would merit its own dedicated review.
Viral STIs
HPV
Human papilloma virus (HPV) is a small circular double-stranded DNA papilloma virus that infects cutaneous or mucosal epithelial tissues in humans14. More than 200 genotypes of HPV have been identified, including at least 40 that affect the genitals, and are grouped into high- or low-risk15. Although HPV infection is often asymptomatic and self-limiting, symptoms can include anogenital warts, respiratory papillomatosis, and precancerous or cancerous cervical, penile, vulvar, vaginal, anal and oropharyngeal lesions16. HPV is the most common STI worldwide, with most sexually active people exposed to it during their lifetime17. Among women, HPV prevalence is highest among those in low- and middle-income countries (LMICs), peaking at <25 years old18. While most women clear HPV spontaneously, persistent infection can cause cervical, anal, or head and neck cancer19. Cervical cancer has been a leading cause of mortality among women for decades; in 2012, there were 266,000 HPV-related cervical cancer deaths worldwide, accounting for 8% of all female cancer deaths that year20. Cervical cancer also causes substantial genitourinary morbidity, including radiation treatment-related infertility and urinary or faecal incontinence21. Persistent infection with high-risk HPV types is responsible for 99.7% of cervical squamous cell cancer cases22.
In women with HPV, one factor that increases the risk of progression to cervical cancer is co-infection with a different STI23. HIV, for example, increased the oncogenic potential of HPV, especially in immunosuppressed women24. Women adherent to antiretroviral therapy are less likely to acquire high-risk HPV types, and progression to pre-malignant or malignant lesions is reduced25. In HIV-negative women, persistent HPV increases the risk of acquiring HIV, but the underlying mechanism is unclear23. Persistent HPV and Chlamydia trachomatis co-infection has also been proposed as a cofactor in the progression of cervical malignancy in women, with chronic inflammation as a mediating factor26. For these reasons, primary prevention using HPV vaccination is essential.
HPV vaccine development is one the most important medical achievements of the twenty-first century. Universal HPV vaccination has the potential to prevent between 70% to 90% of HPV-related disease, including anogenital warts and HPV-associated cancers27. The global strategy of the WHO is to vaccinate 90% of females by age 15, in addition to screening and treating older females, with the goal of eliminating cervical cancer in the next century28. There are four available HPV vaccines: Gardasil (Merck, 2006), Ceravrix (GlaxoSmithKline, 2007), Gardasil 9 (Merck, 2014) and Cecolin (Xiamen Innovax Biotech Co., 2021)27. All offer protection against HPV16 and HPV18 high-risk genotypes, which account for 66% of all cervical cancers (Table 2). Gardasil 9 targets 5 additional oncogenic HPV types (HPV31, 33, 45, 52, 58) that account for another 15% of cervical cancers. Gardasil products also offer protection against HPV6 and HPV11, which cause >90% of genital warts16. Cervarix and Cecolin offer protection only against HPV16 and HPV1829.
HPV vaccination programmes have resulted in a profound reduction in pre-malignant and malignant cancers in women30. In England since 2008, HPV immunization has been routinely recommended for girls aged 12–13 years, with a catch-up programme at 14–18 years. A 2019 observational study of this population reported that for those vaccinated at ages 12–13, there was an estimated 87% relative reduction in cervical cancer rates and a 97% risk reduction for cervical intraepithelial neoplasia 3 compared with a reference unvaccinated cohort. Among vaccinated cohorts in the same study, since 2008, investigators estimated 448 fewer cervical cancers and 17,235 fewer cervical intraepithelial neoplasia 3 cases than expected by 201931. The study authors concluded that the immunization programme in England has almost eliminated cervical cancer in women born since 1995. Programmes in Denmark and Sweden have reported similar levels of success30.
These findings show that elimination of cervical cancer in the short term is possible with primary prevention programmes, at least in adequately resourced countries. In other settings, infrastructural and cultural challenges can make establishment of such programmes difficult. Efforts to implement HPV vaccination programmes in all areas are essential, especially to vaccinate girls before sexual debut and complete all doses in the vaccination series32.
HPV-related anal cancer is also of concern for women, especially those with HIV33. HPV has been linked to 80% of anal cancer cases in the United States34. Women living with HIV have a 7.8-fold higher risk of anal carcinoma in situ and a 10-fold higher risk of anal squamous cell carcinoma compared with women without HIV35,36. In contrast to cervical cancer, it is less clear whether screening for HPV-associated precancerous lesions will impact the incidence of anal cancers. The Anal Cancer HSIL Outcomes Research (ANCHOR) study is an ongoing trial investigating whether treatment of precancerous high-grade squamous intraepithelial lesions (HSIL) is effective in reducing the incidence of anal cancer in people with HIV, including women (NCT02135419). Preliminary results in 4,446 participants demonstrated that removal of HSILs identified on screening anal Papanicolaou smears notably reduced the risk of progression to anal cancer37. Currently, there are no routine screening recommendations for anal cancer for women16.
Detection of high-risk HPV based on cytology screening of precancerous anal lesions is challenging because sensitivity is limited and diagnosis requires the provision of adequate follow-up infrastructure (for example, high-resolution anoscopy). Molecular assays might reduce the number of unnecessary high-resolution anoscopies performed38,39.
HSV
Genital herpes is caused by herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2), which are members of the Herpesviridae family. In 2016, the WHO estimated that up to 192 million people were affected by genital HSV-1 and 491 million people by HSV-240. Although HSV-1 is more commonly associated with oral disease (‘cold sores’), the proportion of sexually transmitted anogenital herpes attributed to HSV-1 has increased over time, especially among women aged 18–30 years old41. HSV-2 is the primary causative agent of genital herpes infections globally42. Although HSV infection is chronic and lifelong, many women experience few or no symptoms. When present, symptoms range from painful genital sores to discomfort that is sometimes misdiagnosed as recurrent vulvovaginal candidiasis. HSV infections can be managed with oral antivirals including suppressive therapy, such as valacylovir (Table 3)16.
One devasting consequence of HSV infection in pregnant women is neonatal herpes. In the U.S., the incidence of neonatal HSV has increased, with 5.3/10,000 infants affected in 2015, up from 3.75/10,000 births in the early 2000s43,44. Neonatal herpes manifests when neonates are infected with HSV during vaginal birth. Neonatal infection can affect the skin, eyes or mouth, but the central nervous system or multiple organs can also become infected; incidence of central nervous system manifestations of neonatal herpes is estimated to be between 1 in 3,000 and 1 in 20,000 live births. Mortality in such cases without treatment is as high as 85%, with a high likelihood of long-term neurological sequalae in those infants who do survive45. Mother-to-child transmission is preventable by elective Caesarian-section delivery in mothers with active herpetic lesions.
HSV-2 infection in women is associated with a threefold increased risk of HIV acquisition and horizontal transmission46,47. One analysis concluded that an estimated 420,000/1.4 million HIV infections (population attributable fraction 29.6% (22.9–37.1)) were attributed to HSV-2 infections worldwide48.
Diagnosis of genital herpes is challenging because characteristic lesions often resolve by the time patients present to care. A presumptive diagnosis can be made by physical examination but should be confirmed with type-specific nucleic acid amplification testing (NAAT) or culture16. The use of HSV serologies is discussed in detail elsewhere16,49.
Episodic and suppressive treatments for HSV do not prevent recurrence. Even if indefinite suppressive antivirals are administered, HSV shedding can still occur50. Lifelong antivirals are not cost effective and perfect adherence can be challenging for patients16. Therefore, there is continued interest in developing vaccines for HSV-2 (Table 2). Despite extensive investigation of many candidate HSV vaccines, none have performed well enough in clinical trials to be brought to the market. In the 1990s, initial studies investigated subunit vaccines, which aimed to select targets that induce immune responses against HSV-251. One such vaccine candidate, Simplirix (GSK), targeted the glycoprotein D subunit (gD), which facilitates host cell entry by HSV. Initial trials demonstrated 74% efficacy in HSV-1/HSV-2 seronegative women with seropositive partners, but these results were not replicated in seronegative men52. Given the promising initial efficacy findings among seronegative women, additional trials were performed in women; however, they largely failed to meet primary endpoints. Most notably, efficacy of the same GSK gD subunit vaccine in the Herpevac trial was only 58% and 20% against HSV-1 and HSV-2, respectively53. The discrepancy in results between these two studies is puzzling, but given that gD is known to elicit a strong immune response, it has been a component in several additional vaccine candidates51,54. A major concern with HSV subunit vaccines is cost, so research and development strategies have pivoted towards cheaper nucleic acid-based vaccine platforms and the potential of live-attenuated vaccines55,56,57. Given the complex immunology of HSV, there is interest in understanding the role of mucosal immunity in the genital tract to aid the development of a successful vaccine against HSV-258.
Bacterial STIs
Syphilis
Syphilis is caused by the spirochaete Treponema pallidum subspecies pallidum. Main symptoms of syphilis include anogenital or oral painless chancres in primary syphilis, diffuse rash in secondary syphilis, aseptic meningitis and pan uveitis59. The impact of syphilis on women has intensified over the past decade. In the United States between 2014 and 2018, rates of primary and secondary syphilis among women doubled and similar trends have been noted globally1,60. Rates of primary and secondary syphilis are lower among US women compared with men who have sex with men (MSM), but cases among heterosexual women increased by 178.6% between 2015 and 2019, suggesting an epidemic mediated by heterosexual transmission60. Increasing primary and secondary syphilis cases among women are also predominant among those of childbearing age60. Therefore, the rising rates of congenital syphilis are not surprising; in 2013, congenital syphilis occurred in 9.2 cases per 100,000 live births and in 2020 increased to 57.3 cases per 100,000 live births60. Tragically, this trajectory has resulted in increasing numbers of syphilitic stillbirths and congenital syphilis-related infant deaths60. Syphilis in pregnancy is the second leading cause of stillbirth globally and has been associated with low birth weight, neonatal infections and preterm delivery61. Congenital syphilis is preventable with early detection and prompt treatment of maternal infection; however, many women lack access to adequate syphilis treatment, even with early diagnosis62. Limited prenatal care and timely syphilis testing are barriers to preventing congenital syphilis, especially in LMICs where prenatal care and syphilis screening resources are limited63. Currently, the CDC and WHO recommend routine serologic screening of pregnant women at their initial prenatal visit, at 28 weeks’ gestation and at the time of delivery in high-prevalence settings, although recommendations vary geographically16,64.
Consequences of untreated syphilis in pregnancy are dire for both mother and neonate. Options for effective treatment are straightforward because syphilis is treatable with penicillin G and antimicrobial resistance is essentially non-existent16. Depending on the stage and site of infection, treatment regimens differ in terms of penicillin dose frequency and route of administration, as discussed elsewhere16. Doxycycline can be given in certain situations to non-pregnant women (that is, in cases of true penicillin allergy) to effectively treat primary, secondary or latent syphilis; however, penicillin G is the only antimicrobial agent that has demonstrated efficacy in preventing congenital syphilis65. Thus, treatment of women with a true penicillin allergy and those who are unable to access penicillin G is challenging. The ideal dosing regimen of penicillin G for syphilis treatment during pregnancy is not clear, but evidence suggests that an additional injection of benzathine penicillin G after the initial dose reduces the risk of congenital syphilis65,66,67.
Chlamydia
Chlamydia trachomatis is an obligate intracellular Gram-negative bacterium that can replicate only inside a host cell68. Although usually asymptomatic in women, C. trachomatis infection can result in reproductive damage, and when untreated, it can be associated with PID, ectopic pregnancy, chronic pelvic pain and tubal infertility. In the U.S., women <25 years account for most infections, so annual screening in this age group is recommended to reduce the frequency of PID and other adverse health outcomes16,60,69. Perinatal maternal Chlamydia infection is associated with preterm birth, stillbirth, low birth weight and neonatal infections such as pneumonia and conjunctivitis69,70,71.
The composition of the vaginal microbiome probably has a role in host defence against chlamydial infection. An optimal vaginal microbiota is dominated by Lactobacillus crispatus, which produces lactic acid that has antimicrobial properties and can inactivate C. trachomatis, decreasing the likelihood of ascension of this pathogen into the upper genital tract72. Women with bacterial vaginosis, defined by a paucity of L. crispatus and other favourable vaginal lactobacilli, and an increased abundance of facultative and strict anaerobes, may have reduced immune defence against C. trachomatis, leading to increased risk of acquiring this pathogen as well as Neisseria gonorrhoeae and Trichomonas vaginalis73.
Prompt diagnosis and treatment are the best approaches to preventing the reproductive morbidity and sequelae associated with chlamydia (Table 3). For decades, single-dose oral azithromycin (2 g) was a first-line treatment option for C. trachomatis, offering the option of directly observed therapy. Recent data suggest that this regimen is inferior to oral doxycycline given twice daily for 7 days, specifically for women and men with urogenital and rectal infection74. Thus, the only currently recommended first-line agent for uncomplicated urogenital or rectal chlamydia is multidose doxycycline16. This change in guidance in 2021 was driven by data related to men with chlamydia; more efficacy studies are needed in women75. However, rectal chlamydial infection has been found to occur in women more frequently than previously thought. In addition to receptive anal sex, auto-inoculation from cervicovaginal chlamydial infection may yield rectal infection76,77. While single-dose azithromycin is efficacious for urogenital C. trachomatis in women, the possibility that concomitant rectal infection that may not be adequately treated with this regimen is concerning78. Single-dose azithromycin is also recommended for the treatment of chlamydia in pregnant women as doxycycline is not safe in pregnancy16.
Currently, no vaccines are available for C. trachomatis79. Given the high rates of re-infection, especially among young women80, vaccines offer the promise of both protecting from disease and reducing antibiotic use, treatment burden, preventing development of antimicrobial resistance in other infections (for example, gonorrhoea) and decreasing reproductive morbidity81,82. A major challenge in C. trachomatis vaccine research has been targeting both humoral and cell-mediated immune responses in infected individuals; complete protection requires activity in both pathways83,84. Comprehensive monitoring of this complicated immune response is difficult. Despite approximately 220 chlamydial vaccine trials having been conducted from 1946 until the present—over seven decades—an effective vaccine remains elusive (Table 2).
Gonorrhoea
Gonorrhoea is caused by N. gonorrhoeae, a Gram-negative diplococcal bacterium. N. gonorrhoeae can yield mucosal infections in epithelia of the urogenital tract and the ectocervix85. Gonorrhoea is extremely common worldwide, with an estimated global annual incidence of 86.9 million adults and a prevalence among women of 0.9%, with the greatest burden among women in LMICs1. Genitourinary gonorrhoea can present in women as cervicitis or urethritis but is mostly asymptomatic86. If untreated, gonococcal infections can result in serious complications such as PID, tubal infertility, ectopic pregnancy and disseminated gonococcal infection87,88,89. Gonorrhoea also facilitates transmission of HIV and other STIs86. Similar to other bacterial STIs, untreated gonorrhoea has been associated with adverse birth outcomes such as preterm birth, low birth weight and premature rupture of membranes90,91. Perinatal exposure to an infected cervix puts neonates at risk for serious complications such as gonococcal sepsis and ophthalmia neonatorum, the latter of which can lead to blindness if untreated92.
When detected in a timely manner, gonorrhoea can be treated and its negative sequelae can be avoided. The landscape of gonorrhoea treatment, however, has been in flux over the past several decades due to the emergence of resistance to multiple antimicrobials among gonococcal isolates worldwide60,93. The Gonococcal Isolate Surveillance Program (GISP) was established in the United States in 1986 to monitor trends in antimicrobial resistance among urethral N. gonorrhoeae isolates. This programme is integral in generating clinical guidance on gonococcal therapy94. Since the generation of GISP, notable gonococcal resistance has emerged to several antimicrobial drug classes, including fluoroquinolones (for example, ciprofloxacin) and macrolides (for example, azithromycin); use of these agents is no longer recommended in national treatment guidelines16,95. The 2021 CDC STI treatment guidelines currently recommend cephalosporins for first-line gonorrhoea treatment, specifically 500 mg intramuscular ceftriaxone for people weighing less than 150 kg16. Oral cephalosporins, such as cefixime, are not recommended as first-line treatment, given many instances of treatment failure and limited efficacy in treating pharyngeal gonococcal infection96,97,98,99,100. While ceftriaxone remains a reliable choice in most situations, there is growing concern for widespread ceftriaxone-resistant gonococcal isolates. Such strains have been reported in Denmark, France, Japan, Thailand and the United Kingdom; alternative treatment options are limited101,102,103,104.
In the past 10 years, several novel anti-gonococcal antimicrobials have been conceptualized and developed105,106,107. One example is zoliflodacin, a single-dose spiropyrimidinetrione antimicrobial that works by inhibiting DNA biosynthesis through blocking gyrase complex cleavage108. In a multicentre Phase 2 trial in the United States, most patients who received zoliflodacin for uncomplicated urogenital and rectal gonococcal infection were successfully treated. Efficacy for treating pharyngeal infections was less impressive, with only 50% and 82% of those who received 2 g and 3 g of zoliflodacin, respectively, achieving cure. Regardless, several studies have shown that zoliflodacin continues to have excellent in vitro activity against multidrug-resistant gonococcal isolates, including those with resistance to extended-spectrum cephalosporins109,110.
Given global increases in antimicrobial resistance, vaccines preventing acquisition of gonorrhoea are urgently needed. Modelling studies have demonstrated that a gonococcal vaccine of moderate efficacy and duration would have a substantial impact on disease prevalence and prevention of adverse reproductive sequelae111. The WHO has named N. gonorrhoeae as a global priority, hence increasing interest and funding have been funnelled into development of candidate gonorrhoea vaccines (Table 2). Fortunately, available tools for other gonococcal species may offer opportunity for N. gonorrhoeae prevention, an approach currently under study. The rMenB+OMV NZ vaccine (Bexsero) was first licensed in the European Union in 2013 and in the United States in 2015 for prevention of meningococcal disease caused by N. meningitidis serogroup B112. An earlier version of a vaccine aimed at a meningococcal B outbreak (MeNZB) was introduced in New Zealand in the early 2000s. A retrospective case-control study revealed that this vaccine programme not only led to a decrease in meningococcal disease, as expected, but had an estimated reduction of future gonorrhoea acquisition of 31% (95% CI: 21–39) in those who received 3 doses of vaccine113. Clinical trials are ongoing to assess the efficacy of Bexsero in preventing urogenital and/or rectal gonorrhoea (NCT 04350138).
Parasitic STIs
Trichomoniasis
Globally, trichomoniasis has an enormous impact on women as the most common non-viral STI1. It is caused by the parasitic protozoan Trichomonas vaginalis, and results in vaginal discharge and dysuria when symptomatic114. T. vaginalis has also been associated with adverse birth outcomes (for example, preterm birth, low birth weight, preterm rupture of membranes)115 and an increased risk of HIV acquisition and transmission, PID and cervical cancer related to HPV infection116,117,118,119. Despite these significant health impacts, has been viewed as a nuisance infection and investigation has been limited until recent years. Globally, trichomoniasis is not currently reportable120,121. Marked racial and geographic disparities have also been described in relation to T. vaginalis infection. In the United States, according to the most recent National Health and Nutrition Examination Survey data, the overall prevalence of T. vaginalis in women in the United States is 1.8%122, being 6.8% among black women compared with 0.4% among women of other racial/ethnic backgrounds122. The global epidemiology of trichomoniasis is less well-defined, but one systematic review including men and women noted a prevalence range of 3.9%–24.6% in LMICs from Latin America and Southern Africa123.
Diagnosis of T. vaginalis has greatly improved in women (and men) over the past decade with the use of highly sensitive and specific NAAT tests124,125,126,127. Treatment recommendations for women with T. vaginalis have been largely unchanged for decades, with 5-nitroimidazoles such as metronidazole (MTZ) and tinidazole (TDZ) remaining mainstays of therapy (Table 3). Guidelines published by the WHO in June 2021 recommend treatment with either a single dose of MTZ (2 g orally) or twice-daily dose of MTZ (500 mg orally) for 7 days128. In LMIC and other resource-limited settings where adherence to a multidose MTZ regimen may be difficult, a single-dose treatment option may be advantageous. Accumulating data suggest, however, that single-dose treatment with MTZ for women may not be optimal129,130. A recent multicentre randomized controlled trial in the United States compared the multidose oral MTZ regimen to the single-dose regimen among HIV-negative women. Participants who received the multidose regimen were significantly less likely to re-test positive for T. vaginalis at 1 month compared with women in the single-dose group; adherence among both groups were similar130. Thus, the multidose oral MTZ regimen is now the recommended regimen for all women; this update may influence future global guidelines moving forward16. Notably, MTZ is safe for pregnant women at all stages of pregnancy131. Therefore, to prevent adverse birth outcomes associated with this infection, prompt treatment is essential115,131.
Due to limited clinical trial data in men, the single 2 g dose of oral MTZ remains the recommended treatment regimen for T. vaginalis in men16. This is the first time there has been a discrepancy in the treatment of an STI based on gender. Such a situation could lead to complicated public health logistics in partner treatment of infected women and additional studies are needed to discover the optimal treatment regimen for men132. Women are re-infected by their male sex partners if they are either not treated or are inadequately treated for trichomoniasis133.
Oral secnidazole (SEC) was recently approved by the US Food and Drug Administration (FDA) for treatment of T. vaginalis in both men and women. Given its microbiologic cure rate of 92.2% in a randomized double-blind placebo-controlled delayed-treatment study, SEC offers a promising new single-dose treatment option for trichomoniasis134.
STI prevention challenges and disparities in minority populations
Gender minority women
STI prevention poses challenges for women in general, but some populations face additional barriers to sexual healthcare (Table 4). Gender minority women, including transgender women (TGW), or people who were assigned male sex at birth but whose gender identity is female, are at high risk of acquiring STIs through engagement in sexual behaviours such as commercial sex work and condomless anal receptive intercourse135. Consequently, STIs disproportionally affect TGW; an estimated 14% of TGW in the United States are living with HIV136, and global bacterial STI prevalence has been reported to be as high as 50%, 19% and 25% for syphilis, gonorrhoea and chlamydia, respectively8,135,136. These high rates may be related to the limited engagement of TGW with effective sexual health services—for example, regular HIV/STI screening—and underutilization of pre-exposure prophylaxis137,138. This lack of engagement arises from a suite of factors, including stigma, mistrust of the healthcare system, limited trans-affirming clinical services, previous sexual trauma or competing healthcare priorities such as hormone replacement therapy for gender-affirming therapy139,140.
Given the combination of this population’s unique sexual health needs and mistrust of the medical establishment, community-driven patient-centred prevention efforts are necessary. One qualitative study assessing attitudes related to HIV prevention among TGW in the Southeastern United States found that limited trans-affirming sexual health resources are a major barrier to engaging in care141. In addition, an individualized approach to affirming sexual history-taking should be employed by providers when caring for TGW. More broadly, another driver of sexual health disparities among TGW is their limited representations in research studies and clinical trials in the field. Data for TGW are often aggregated together with those of cisgender MSM and thus difficult to interpret. Study design and trial recruitment planning efforts must be made to appropriately report data on TGW.
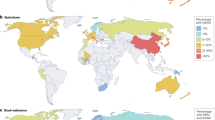
Women in LMICs
Women living in LMICs face additional STI prevention challenges largely due to limited healthcare infrastructure, availability of sexual health resources and misogynistic cultural attitudes towards sexuality142. African countries have been particularly impacted, with the most recent WHO STI global prevalence estimates reporting the highest rates worldwide for gonorrhoea, trichomoniasis and syphilis among women in the region1. In addition, until very recently, distribution of HPV vaccines has been largely limited to European and North American nations, with LMICs receiving little support until approximately 2019. Even when HPV vaccines were introduced in many LMICs, uptake of the full series has been limited due to logistical challenges, highlighting an enormous, missed opportunity to curtail the rates of cervical cancer worldwide32.
Affordable STI testing that can be performed at the point-of-care is an important tool that needs to be made available to women in LMICs. Concurrent availability and accessibility of appropriate treatment for STIs are also essential. Clinics or other community settings need to provide confidential diagnostics and treatment to mitigate restricted access owing to stigma and the potential for gender-based violence that sometimes occurs when male sexual partners find out about sexual health diagnoses. Vaccines against STIs such as C. trachomatis and HSV-2 also hold great promise for women of LMICs, offering both disease prevention and a reduction in the need for diagnosis and treatment. Continued pursuit of safe and effective STI vaccines should be prioritized.
Conclusion
Women are disproportionately affected by STIs throughout their lives compared with men. This is mainly owing to the higher efficiency of male-to-female transmission of STIs and the biology of the female reproductive tract. In addition, the social and structural barriers to women realizing full sexual health include limited availability of HPV immunization in many parts of the world, barriers to contraception access, lack of confidential evaluation and counselling services, and lack of STI diagnostics. Finally, women are generally less well-resourced, both financially and socially, than men. This restricts their access to the resources required for sexual safety such as comprehensive sexual healthcare and HIV/STI prevention services, and the financial security that is fundamental to sexual health. Ensuring access to diagnostics and therapies on its own will not address the yawning gap in sexual health between men and women but would be a good start.
References
Rowley, J. et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull. World Health Organ. 97, 548–562 (2019).
Reported STDs reach all-time high for 6th consecutive year. CDC (3 April 2021); https://www.cdc.gov/nchhstp/newsroom/2021/2019-std-surveillance-report-press-release.html
Kreisel, K. M. et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex. Transm. Dis. https://doi.org/10.1097/OLQ.0000000000001355 (2021).
Rietmeijer, C. A. et al. Report from the national academies of sciences, engineering and medicine–STI: adopting a sexual health paradigm–a synopsis for sti practitioners, clinicians, and researchers. Sex. Transm. Dis. https://doi.org/10.1097/olq.0000000000001552 (2021).
CDC Fact Sheet: 10 Ways STDs Impact Women Differently from Men (Centers for Disease Control and Prevention, 2011); https://www.cdc.gov/std/health-disparities/stds-women-042011.pdf
Smolarczyk, K. et al. The impact of selected bacterial sexually transmitted diseases on pregnancy and female fertility. Int. J. Mol. Sci. 22, 2170 (2021).
Van Gerwen, O. T., Aryanpour, Z., Selph, J. P. & Muzny, C. A. Anatomical and sexual health considerations among transfeminine individuals who have undergone vaginoplasty: a review. Int. J. STD AIDS 33, 106–113 (2022).
Van Gerwen, O. T. et al. Prevalence of sexually transmitted infections and human immunodeficiency virus in transgender persons: a systematic review. Transgend. Health 5, 90–103 (2020).
Deese, J. et al. Recent advances and new challenges in cisgender women’s gynecologic and obstetric health in the context of HIV. Clin. Obstet. Gynecol. 64, 475–490 (2021).
Hodges-Mameletzis, I. et al. Pre-exposure prophylaxis for HIV prevention in women: current status and future directions. Drugs 79, 1263–1276 (2019).
O’Leary, A. Women and HIV in the twenty-first century: how can we reach the UN 2030 goal? AIDS Educ. Prev. 30, 213–224 (2018).
Heumann, C. L. Biomedical approaches to HIV prevention in women. Curr. Infect. Dis. Rep. 20, 11 (2018).
Kharsany, A. B. & Karim, Q. A. HIV infection and AIDS in Sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J. 10, 34–48 (2016).
Burk, R. D., Harari, A. & Chen, Z. Human papillomavirus genome variants. Virology 445, 232–243 (2013).
Burd, E. M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 16, 1–17 (2003).
Workowski, K. A. et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm. Rep. 70, 1–187 (2021).
Human Papilloma Virus Statistics (Centers for Disease Control and Prevention, 2021); https://www.cdc.gov/std/hpv/stats.htm
Bruni, L. et al. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 202, 1789–1799 (2010).
Brianti, P., De Flammineis, E. & Mercuri, S. R. Review of HPV-related diseases and cancers. New Microbiol. 40, 80–85 (2017).
de Martel, C., Plummer, M., Vignat, J. & Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 141, 664–670 (2017).
Serrano, B., Brotons, M., Bosch, F. X. & Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 47, 14–26 (2018).
Walboomers, J. M. et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 189, 12–19 (1999).
Liu, G. et al. Prevalent HPV infection increases the risk of HIV acquisition in African women: advancing the argument for HPV immunization. AIDS https://doi.org/10.1097/qad.0000000000003004 (2021).
Liu, G., Sharma, M., Tan, N. & Barnabas, R. V. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS 32, 795–808 (2018).
Kelly, H., Weiss, H. A., Benavente, Y., de Sanjose, S. & Mayaud, P. Association of antiretroviral therapy with high-risk human papillomavirus, cervical intraepithelial neoplasia, and invasive cervical cancer in women living with HIV: a systematic review and meta-analysis. Lancet HIV 5, e45–e58 (2018).
Smith, J. S. et al. Evidence for Chlamydia trachomatis as a human papillomavirus cofactor in the etiology of invasive cervical cancer in Brazil and the Philippines. J. Infect. Dis. 185, 324–331 (2002).
Wang, R. et al. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 471, 88–102 (2020).
Cervical Cancer Elimination Initiative (WHO, 2022); https://www.who.int/initiatives/cervical-cancer-elimination-initiative
Monie, A., Hung, C.-F., Roden, R. & Wu, T. C. Cervarix: a vaccine for the prevention of HPV 16, 18-associated cervical cancer. Biologics 2, 97–105 (2008).
Lei, J. et al. HP V vaccination and the risk of invasive cervical cancer. N. Eng. J. Med. 383, 1340–1348 (2020).
Falcaro, M. et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet https://doi.org/10.1016/s0140-6736(21)02178-4 (2021).
Bruni, L. et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev. Med. 144, 106399 (2021).
Clifford, G. M. et al. Toward a unified anal cancer risk scale. Int. J. Cancer 148, 38–47 (2021). A meta-analysis of anal cancer incidence by risk group.
Chin-Hong, P. V. & Palefsky, J. M. Human papillomavirus anogenital disease in HIV-infected individuals. Dermatol. Ther. 18, 67–76 (2005).
Frisch, M., Biggar, R. J. & Goedert, J. J. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J. Natl Cancer Inst. 92, 1500–1510 (2000).
Silverberg, M. J. et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin. Infect. Dis. 54, 1026–1034 (2012).
Palefsky, J. et al. Treatment of anal high-grade squamous intraepithelial lesions to prevent anal cancer. N. Engl. J. Med. 386, 2273–2282 (2022).
Ellsworth, G. B. et al. Xpert HPV as a screening tool for anal histologic high-grade squamous intraepithelial lesions in women living with HIV. J. Acquir. Immune Defic. Syndr. 87, 978–984 (2021).
Chiao, E. Y. et al. Screening strategies for the detection of anal high-grade squamous intraepithelial lesions in women living with HIV. AIDS 34, 2249–2258 (2020).
Herpes Simplex Virus (WHO, 2022); https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Bernstein, D. I. et al. Epidemiology, clinical presentation, and antibody response to primary infection with herpes simplex virus type 1 and type 2 in young women. Clin. Infect. Dis. 56, 344–351 (2012).
James, C. et al. Herpes simplex virus: global infection prevalence and incidence estimates, 2016. Bull. World Health Organ. 98, 315–329 (2020).
Mahant, S. et al. Neonatal herpes simplex virus infection among medicaid-enrolled children: 2009–2015. Pediatrics https://doi.org/10.1542/peds.2018-3233 (2019).
Kimberlin, D. W. Neonatal herpes simplex infection. Clin. Microbiol. Rev. 17, 1–13 (2004).
Kimberlin, D. Herpes simplex virus, meningitis and encephalitis in neonates. Herpes 11, 65a–76a (2004).
Masese, L. et al. Changes in the contribution of genital tract infections to HIV acquisition among Kenyan high-risk women from 1993 to 2012. AIDS 29, 1077–1085 (2015).
Freeman, E. E. et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS 20, 73–83 (2006).
Looker, K. J. et al. Global and regional estimates of the contribution of herpes simplex virus type 2 infection to HIV incidence: a population attributable fraction analysis using published epidemiological data. Lancet Infect. Dis. 20, 240–249 (2020).
Feltner, C. et al. Serologic screening for genital herpes: an updated evidence report and systematic review for the US preventive services task force. JAMA 316, 2531–2543 (2016).
Venturino, E., Shoukat, A. & Moghadas, S. M. Dynamics of HSV-2 infection with a therapeutic vaccine. Heliyon 6, e04368 (2020).
Kim, H. C. & Lee, H. K. Vaccines against genital herpes: where are we? Vaccines https://doi.org/10.3390/vaccines8030420 (2020).
Stanberry, L. R. et al. Glycoprotein-D–adjuvant vaccine to prevent genital herpes. N. Engl. J. Med. 347, 1652–1661 (2002).
Belshe, R. B. et al. Efficacy results of a trial of a herpes simplex vaccine. N. Engl. J. Med. 366, 34–43 (2012).
Bernstein, D. I. et al. Therapeutic vaccine for genital herpes simplex virus-2 infection: findings from a randomized trial. J. Infect. Dis. 215, 856–864 (2017).
Dropulic, L. K. et al. A randomized, double-blinded, placebo-controlled, phase 1 study of a replication-defective herpes simplex virus (HSV) type 2 vaccine, HSV529, in adults with or without HSV infection. J. Infect. Dis. 220, 990–1000 (2019).
Chandra, J. et al. Immune responses to a HSV-2 polynucleotide immunotherapy COR-1 in HSV-2 positive subjects: a randomized double blinded phase I/IIa trial. PLoS ONE 14, e0226320 (2019).
Veselenak, R. L. et al. A Vaxfectin(®)-adjuvanted HSV-2 plasmid DNA vaccine is effective for prophylactic and therapeutic use in the guinea pig model of genital herpes. Vaccine 30, 7046–7051 (2012).
Roth, K., Ferreira, V. H. & Kaushic, C. HSV-2 vaccine: current state and insights into development of a vaccine that targets genital mucosal protection. Microb. Pathog. 58, 45–54 (2013).
Peeling, R. W. et al. Syphilis. Nat. Rev. Dis. Primers 3, 17073 (2017).
Sexually Transmitted Disease Surveillance 2019 (Centers for Disease Control and Prevention, accessed 1 December 2021); https://www.cdc.gov/std/statistics/2019/default.htm
Data on Syphilis (WHO, 2021); https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-syphilis
Wu, M. X. et al. Congenital syphilis on the rise: the importance of testing and recognition. Med. J. Aust. 215, 345–346.e1 (2021).
Hopkins, A. O. et al. Evaluation of the WHO/CDC Syphilis Serology Proficiency Programme to support the global elimination of mother-to-child transmission of syphilis: an observational cross-sectional study, 2008–2015. BMJ Open 10, e029434 (2020).
WHO Guideline on Syphilis Screening and Treatment for Pregnant Women (WHO, 2017).
Wendel, G. D. Jr. et al. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin. Infect. Dis. 35, S200–S209 (2002).
Walker, G. J. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst. Rev. 2001, Cd001143 (2001).
Alexander, J. M., Sheffield, J. S., Sanchez, P. J., Mayfield, J. & Wendel, G. D. Jr. Efficacy of treatment for syphilis in pregnancy. Obstet. Gynecol. 93, 5–8 (1999).
Witkin, S. S. et al. Chlamydia trachomatis: the persistent pathogen. Clin. Vaccine Immunol. 24, e00203-17 (2017).
He, W., Jin, Y., Zhu, H., Zheng, Y. & Qian, J. Effect of Chlamydia trachomatis on adverse pregnancy outcomes: a meta-analysis. Arch. Gynecol. Obstet. 302, 553–567 (2020).
Hammerschlag, M. R. Chlamydial and gonococcal infections in infants and children. Clin. Infect. Dis. 53, S99–S102 (2011).
Hammerschlag, M. R., Chandler, J. W., Alexander, E. R., English, M. & Koutsky, L. Longitudinal studies on chlamydial infections in the first year of life. Pediatr. Infect. Dis. 1 (1982).
Gong, Z., Luna, Y., Yu, P. & Fan, H. Lactobacilli inactivate Chlamydia trachomatis through lactic acid but not H2O2. PLoS ONE 9, e107758 (2014).
Brotman, R. M. et al. Bacterial vaginosis assessed by gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J. Infect. Dis. 202, 1907–1915 (2010).
Dukers-Muijrers, N. et al. Treatment effectiveness of azithromycin and doxycycline in uncomplicated rectal and vaginal Chlamydia trachomatis infections in women: a multicenter observational study (FemCure). Clin. Infect. Dis. 69, 1946–1954 (2019).
Kissinger, P. J. et al. Azithromycin treatment failure for Chlamydia trachomatis among heterosexual men with nongonococcal urethritis. Sex. Transm. Dis. 43, 599–602 (2016).
Gratrix, J. et al. Evidence for increased Chlamydia case finding after the introduction of rectal screening among women attending 2 Canadian sexually transmitted infection clinics. Clin. Infect. Dis. 60, 398–404 (2015).
Rank, R. G. & Yeruva, L. An alternative scenario to explain rectal positivity in Chlamydia-infected individuals. Clin. Infect. Dis. 60, 1585–1586 (2015).
Lazenby, G. B., Korte, J. E., Tillman, S., Brown, F. K. & Soper, D. E. A recommendation for timing of repeat Chlamydia trachomatis test following infection and treatment in pregnant and nonpregnant women. Int. J. STD AIDS 28, 902–909 (2017).
Phillips, S., Quigley, B. L. & Timms, P. Seventy years of Chlamydia vaccine research – limitations of the past and directions for the future. Front. Microbiol. https://doi.org/10.3389/fmicb.2019.00070 (2019).
Whittington, W. L. et al. Determinants of persistent and recurrent Chlamydia trachomatis infection in young women: results of a multicenter cohort study. Sex. Transm. Dis. 28, 117–123 (2001).
Owusu-Edusei, K. Jr. et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex. Transm. Dis. 40, 197–201 (2013).
Unemo, M. et al. Sexually transmitted infections: challenges ahead. Lancet Infect. Dis. 17, e235–e279 (2017).
Williams, D. M., Grubbs, B. & Schachter, J. Primary murine Chlamydia trachomatis pneumonia in B-cell-deficient mice. Infect. Immun. 55, 2387–2390 (1987).
Ramsey, K. H., Soderberg, L. & Rank, R. G. Resolution of chlamydial genital infection in B-cell-deficient mice and immunity to reinfection. Infect. Immun. 56, 1320–1325 (1988).
Quillin, S. J. & Seifert, H. S. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat. Rev. Microbiol. 16, 226–240 (2018).
Hook, E. W. in Sexually Transmitted Diseases (eds Sparling, P. F. et al.) 451–466 (McGraw-Hill, 1999).
Brunham, R. C., Gottlieb, S. L. & Paavonen, J. Pelvic inflammatory disease. N. Engl. J. Med. 372, 2039–2048 (2015).
Reekie, J. et al. Risk of pelvic inflammatory disease in relation to chlamydia and gonorrhea testing, repeat testing, and positivity: a population-based cohort study. Clin. Infect. Dis. 66, 437–443 (2017).
Farley, T. A., Cohen, D. A. & Elkins, W. Asymptomatic sexually transmitted diseases: the case for screening. Prev. Med. 36, 502–509 (2003).
Gao, R. et al. Association of maternal sexually transmitted infections with risk of preterm birth in the United States. JAMA Netw. Open 4, e2133413 (2021).
Vallely, L. M. et al. Adverse pregnancy and neonatal outcomes associated with Neisseria gonorrhoeae: systematic review and meta-analysis. Sex. Transm. Infect. 97, 104–111 (2021).
Unemo, M. et al. Gonorrhoea. Nat. Rev. Dis. Primers 5, 79 (2019).
Multi-Drug Resistant Gonorrhoea (WHO, 2021); https://www.who.int/news-room/fact-sheets/detail/multi-drug-resistant-gonorrhoea
Schwarcz, S. K. et al. National surveillance of antimicrobial resistance in Neisseria gonorrhoeae. The Gonococcal Isolate Surveillance Project. JAMA 264, 1413–1417 (1990).
Update to CDC’s sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb. Mortal. Wkly Rep. 56, 332–336 (2007).
Allen, V. G. et al. Neisseria gonorrhoeae treatment failure and susceptibility to cefixime in Toronto, Canada. JAMA 309, 163–170 (2013).
Unemo, M., Golparian, D., Potočnik, M. & Jeverica, S. Treatment failure of pharyngeal gonorrhoea with internationally recommended first-line ceftriaxone verified in Slovenia, September 2011. Euro Surveill. 17 (2012).
Unemo, M., Golparian, D. & Hestner, A. Ceftriaxone treatment failure of pharyngeal gonorrhoea verified by international recommendations, Sweden, July 2010. Euro Surveill. 16, 19792 (2011).
van Dam, A. P. et al. Verified clinical failure with cefotaxime 1g for treatment of gonorrhoea in the Netherlands: a case report. Sex. Transm. Infect. 90, 513–514 (2014).
Lewis, D. A. et al. Phenotypic and genetic characterization of the first two cases of extended-spectrum-cephalosporin-resistant Neisseria gonorrhoeae infection in South Africa and association with cefixime treatment failure. J. Antimicrob. Chemother. 68, 1267–1270 (2013).
Kueakulpattana, N. et al. Multidrug-resistant Neisseria gonorrhoeae infection in heterosexual men with reduced susceptibility to ceftriaxone, first report in Thailand. Sci. Rep. 11, 21659 (2021).
Lee, K. et al. Clonal expansion and spread of the ceftriaxone-resistant Neisseria gonorrhoeae strain FC428, identified in Japan in 2015, and closely related isolates. J. Antimicrob. Chemother. 74, 1812–1819 (2019).
Terkelsen, D. et al. Multidrug-resistant Neisseria gonorrhoeae infection with ceftriaxone resistance and intermediate resistance to azithromycin, Denmark, 2017. Euro Surveill. 22, 17–00659 (2017).
de Curraize, C. et al. Ceftriaxone-resistant Neisseria gonorrhoeae isolates (2010 to 2014) in France characterized by using whole-genome sequencing. Antimicrob. Agents Chemother. 60, 6962–6964 (2016).
Jacobsson, S. et al. In vitro activity of the novel triazaacenaphthylene gepotidacin (GSK2140944) against MDR Neisseria gonorrhoeae. J. Antimicrobial. Chemother. 73, 2072–2077 (2018).
Jacobsson, S. et al. In vitro activity of the novel Pleuromutilin lefamulin (BC-3781) and effect of efflux pump inactivation on multidrug-resistant and extensively drug-resistant Neisseria gonorrhoeae. Antimicrob. Agents Chemother. 61, 11 (2017).
Jacobsson, S. et al. In vitro activity of the novel oral antimicrobial SMT-571, with a new mechanism of action, against MDR and XDR Neisseria gonorrhoeae: future treatment option for gonorrhoea? J. Antimicrobial. Chemother. 74, 1591–1594 (2019).
Taylor, S. N. et al. Single-dose zoliflodacin (ETX0914) for treatment of urogenital gonorrhea. N. Engl. J. Med. 379, 1835–1845 (2018).
Le, W. et al. Susceptibility trends of zoliflodacin against multidrug-resistant Neisseria gonorrhoeae clinical isolates in Nanjing, China, 2014 to 2018. Antimicrob. Agents Chemother. https://doi.org/10.1128/aac.00863-20 (2021).
Unemo, M. et al. High susceptibility to zoliflodacin and conserved target (GyrB) for zoliflodacin among 1209 consecutive clinical Neisseria gonorrhoeae isolates from 25 European countries, 2018. J. Antimicrob. Chemother. 76, 1221–1228 (2021).
Craig, A. P. et al. The potential impact of vaccination on the prevalence of gonorrhea. Vaccine 33, 4520–4525 (2015).
Ruiz García, Y. et al. Looking beyond meningococcal B with the 4CMenB vaccine: the Neisseria effect. NPJ Vaccines 6, 130–130 (2021).
Petousis-Harris, H. et al. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhoea in New Zealand: a retrospective case-control study. Lancet 390, 1603–1610 (2017).
Meites, E. et al. A review of evidence-based care of symptomatic Trichomoniasis and asymptomatic Trichomonas vaginalis Infections. Clin. Infect. Dis. 61, S837–S848 (2015).
Van Gerwen, O. T. et al. Trichomoniasis and adverse birth outcomes: a systematic review and meta-analysis. BJOG 128, 1907–1915 (2021).
Kissinger, P. & Adamski, A. Trichomoniasis and HIV interactions: a review. Sex. Trans. Infect. 89, 426–433 (2013).
Yang, M. et al. Co-infection with Trichomonas vaginalis increases the risk of cervical intraepithelial neoplasia grade 2-3 among HPV16 positive female: a large population-based study. BMC Infect. Dis. 20, 642 (2020).
Yang, S. et al. Trichomonas vaginalis infection-associated risk of cervical cancer: a meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 228, 166–173 (2018).
Moodley, P. et al. Trichomonas vaginalis is associated with pelvic inflammatory disease in women infected with human immunodeficiency virus. Clin. Infect. Dis. 34, 519–522 (2002).
Muzny, C. A. Why does Trichomonas vaginalis continue to be a "neglected" sexually transmitted infection? Clin. Infect. Dis. 67, 218–220 (2018).
Hoots, B. E. et al. A trich-y question: should Trichomonas vaginalis infection be reportable? Sex Transm. Dis. 40, 113–116 (2013).
Patel, E. U. et al. Prevalence and correlates of Trichomonas vaginalis infection among men and women in the United States. Clin. Infect. Dis. 67, 211–217 (2018).
Joseph Davey, D. L. et al. Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015: a systematic review. Sex. Trans. Dis. 43, 450–458(2016).
Schwebke, J. R. et al. Molecular testing for Trichomonas vaginalis in women: results from a prospective U.S. clinical trial. J. Clin. Microbiol. 49, 4106–4111 (2011).
Van Der Pol, B. et al. Detection of Trichomonas vaginalis DNA by use of self-obtained vaginal swabs with the BD ProbeTec Qx assay on the BD Viper system. J. Clin. Microbiol. 52, 885–889 (2014).
Van Der Pol, B. et al. Clinical performance of the BD CTGCTV2 assay for the BD MAX System for detection of Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis infections. Sex. Trans. Dis. 48, 134–140 (2021).
Van Der Pol, B. A profile of the cobas® TV/ MG test for the detection of Trichomonas vaginalis and Mycoplasma genitalium. Exp. Rev. Molec. Diag. 20, 381–386 (2020).
Guidelines for the Management of Symptomatic Sexually Transmitted Infections (World Health Organization, 2021).
Howe, K. & Kissinger, P. J. Single-dose compared with multidose metronidazole for the treatment of trichomoniasis in women: a meta-analysis. Sex. Trans. Dis. 44, 29–34 (2017).
Kissinger, P. et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: an open-label, randomised controlled trial. Lancet Infect. Dis. 18, 1251–1259 (2018).
Mann, J. R. et al. Treatment of trichomoniasis in pregnancy and preterm birth: an observational study. J. Womens Health 18, 493–497 (2009).
Muzny, C. A., Richter, S. & Kissinger, P. Is It time to stop using single-dose oral metronidazole for the treatment of trichomoniasis in women? Sex. Trans. Dis. 46, e57–e59 (2019).
Van Gerwen, O. T. et al. Epidemiology, natural history, diagnosis, and treatment of Trichomonas vaginalis in men. Clin. Infect. Dis. 73, 1119–1124 (2021).
Muzny, C. A. et al. Efficacy and safety of single oral dosing of secnidazole for trichomoniasis in women: results of a phase 3, randomized, double-blind, placebo-controlled, delayed-treatment study. Clin. Infect. Dis. 73, e1282–e1289 (2021).
Herbst, J. H. et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 12, 1–17 (2008).
HIV Infection Risk, Prevention, and Testing Behaviors Among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 23 U.S. Cities, 2017 (CDC, 2019).
Sullivan, P. S. et al. Trends in the use of oral emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis against HIV infection, United States, 2012-2017. Ann. Epidemiol. 28, 833–840 (2018).
Pitasi, M. A. et al. HIV testing among transgender women and men - 27 states and guam, 2014-2015. MMWR Morb. Mortal. Wkly Rep. 66, 883–887 (2017).
Phillips, G. II et al. Utilization and avoidance of sexual health services and providers by YMSM and transgender youth assigned male at birth in Chicago. AIDS Care 31, 1282–1289 (2019).
Fisher, C. B. et al. Perceived barriers to HIV prevention services for transgender youth. LGBT Health 5, 350–358 (2018).
Van Gerwen, O. T. et al. ‘It's behaviors, not identity’: attitudes and beliefs related to HIV risk and pre-exposure prophylaxis among transgender women in the Southeastern United States. PLoS ONE 17, e0262205 (2022).
van der Ham, M. et al. Gender inequality and the double burden of disease in low-income and middle-income countries: an ecological study. BMJ Open 11, e047388 (2021).
Petca, A. et al. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp. Ther. Med. 20, 186–186 (2020).
Sun-Kuie, T., Tew-Hongw, H. & Soo-Kim, L.-T. Is genital human papillomavirus infection always sexually transmitted? Aust. N. Z. J. Obstet. Gynaecol. 30, 240–242 (1990).
Hong, Y., Li, S.-Q., Hu, Y.-L. & Wang, Z.-Q. Survey of human papillomavirus types and their vertical transmission in pregnant women. BMC. Infect. Dis. 13, 109 (2013).
Graham, S. V. The human papillomavirus replication cycle, and its links to cancer progression: a comprehensive review. Clin. Sci. 131, 2201–2221 (2017).
Schiffer, J. T. et al. Herpes simplex virus-2 transmission probability estimates based on quantity of viral shedding. J. R. Soc. Interface 11, 20140160 (2014).
Kriebs, J. M. Understanding herpes simplex virus: transmission, diagnosis, and considerations in pregnancy management. J. Midwifery Womens Health 53, 202–208 (2008).
Ribes, J. A. et al. Six-year study of the incidence of herpes in genital and nongenital cultures in a central Kentucky medical center patient population. J. Clin. Microbiol. 39, 3321–3325 (2001).
Cliffe, A. R. & Wilson, A. C. Restarting lytic gene transcription at the onset of herpes simplex virus reactivation. J. Virol. 91, 2 (2017).
Stoltey, J. E. & Cohen, S. E. Syphilis transmission: a review of the current evidence. Sex. Health 12, 103–109 (2015).
Ko, W. J. et al. Successful prevention of syphilis transmission from a multiple organ donor with serological evidence of syphilis. Transplant. Proc. 30, 3667–3668 (1998).
Raguse, J. D. et al. Occupational syphilis following scalpel injury. Ann. Intern. Med. 156, 475–476 (2012).
Peeling, R. W. et al. Syphilis. Nat. Rev. Dis. Primers 3, 17073 (2017).
Chlamydia CDC Fact Sheet (CDC, accessed 7 Feb 2022); https://www.cdc.gov/std/chlamydia/stdfact-chlamydia.htm
Elwell, C., Mirrashidi, K. & Engel, J. Chlamydia cell biology and pathogenesis. Nat. Rev. Microbiol. 14, 385–400 (2016).
Gonorrhea CDC Fact Sheet (CDC, accessed 7 February 2022); https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea-detailed.htm
Quillin, S. J. & Seifert, H. S. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat. Rev. Microbiol. 16, 226–240 (2018).
Burch, T. A., Rees, C. W. & Reardon, L. V. Epidemiological studies on human trichomoniasis. Am. J. Trop. Med. Hyg. 8, 312–318 (1959).
Crucitti, T. et al. Non-sexual transmission of Trichomonas vaginalis in adolescent girls attending school in Ndola, Zambia. PLoS ONE 6, e16310 (2011).
Peterson, K. & Drame, D. Iatrogenic transmission of Trichomonas vaginalis by a traditional healer. Sex. Trans. Infect. 86, 353–354 (2010).
Edwards, T. et al. Trichomonas vaginalis: clinical relevance, pathogenicity and diagnosis. Crit. Rev. Microbiol. 42, 406–417 (2016).
Acknowledgements
We thank N. J. Van Wagoner for advice on the HSV vaccinology section of this paper and M. Kawai from the UAB Center of Clinical and Translational Sciences for assistance in creating figures. O.T.V.G. acknowledges the Doris Duke Charitable Foundation COVID-19 Fund to Retain Clinician Scientists (Grant No. 2021255) and the UAB COVID-19 CARES Retention Program (CARES at UAB).
Author information
Authors and Affiliations
Contributions
O.T.V.G. led efforts in the literature review and writing of this manuscript. C.A.M. and J.M.M. contributed to the final version of the manuscript. All authors conceived the main conceptual ideas for the manuscript together.
Corresponding author
Ethics declarations
Competing interests
O.T.V.G. has received research grant support from Gilead Sciences, Inc. and Abbott Molecular, and serves on the scientific advisory board for Scynexis. C.A.M. has received research grant support from Lupin Pharmaceuticals, Gilead Sciences, Inc. and Abbott Molecular, is a consultant for Cepheid, Scynexis, Lupin Pharmaceuticals, PhagoMed and BioFire Diagnostics, and has received honoraria from Elsevier, Abbott Molecular, Cepheid, Becton Dickinson, Roche Diagnostics and Lupin. J.M. serves on scientific advisory committees for Merck and Gilead, has received research grant support from Becton Dickinson and GlaxoSmithKline, and serves as a scientific advisor for OSEL.
Peer review
Peer review information
Nature Microbiology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Van Gerwen, O.T., Muzny, C.A. & Marrazzo, J.M. Sexually transmitted infections and female reproductive health. Nat Microbiol 7, 1116–1126 (2022). https://doi.org/10.1038/s41564-022-01177-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-022-01177-x
This article is cited by
-
A systematic review of the association between history of sexually transmitted infections and subsequent condom use in adolescents
BMC Public Health (2024)
-
Prevalence of five treatable sexually transmitted infections among women in Lower River region of The Gambia
BMC Infectious Diseases (2023)
-
Women Want Choices: Opinions from the Share.Learn.Shape Global Internet Survey About Multipurpose Prevention Technology (MPT) Products in Development
AIDS and Behavior (2023)