Abstract
Allogeneic haematopoietic cell transplantation (allo-HCT) induces profound shifts in the intestinal bacterial microbiota. The dynamics of intestinal fungi and their impact on clinical outcomes during allo-HCT are not fully understood. Here we combined parallel high-throughput fungal ITS1 amplicon sequencing, bacterial 16S amplicon sequencing and fungal cultures of 1,279 faecal samples from a cohort of 156 patients undergoing allo-HCT to reveal potential trans-kingdom dynamics and their association with patient outcomes. We saw that the overall density and the biodiversity of intestinal fungi were stable during allo-HCT but the species composition changed drastically from day to day. We identified a subset of patients with fungal dysbiosis defined by culture positivity (n = 53) and stable expansion of Candida parapsilosis complex species (n = 19). They presented with distinct trans-kingdom microbiota profiles, characterized by a decreased intestinal bacterial biomass. These patients had worse overall survival and higher transplant-related mortality independent of candidaemia. This expands our understanding of the clinical significance of the mycobiota and suggests that targeting fungal dysbiosis may help to improve long-term patient survival.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Fungal ITS1 and bacterial 16S amplicon sequences specific to this paper are deposited in NCBI SRA under Bioproject PRJNA746305. Samples, sequences and their accession numbers are provided in the Supplementary Data. Clinical and laboratory data used for the analyses in this manuscript are listed in the Supplementary Data. Additional requests for clinical data and materials will be reviewed by MSKCC to determine if they are subject to intellectual property or confidentiality obligations. Data and materials that can be shared will be released via a material transfer or data-sharing agreements and can be requested from the corresponding author.
Code availability
Denoising and taxonomic annotation pipelines were customized as reported49. All analyses were performed in R using base R and publicly available packages. Analysis code can be requested from T.R. (e-mail: rollingt@mskcc.org).
Change history
30 March 2022
In the version of the Supplementary Data initially published in this article, decimals were missing in the second column of the “qpcr_results” tab, and have now been restored.
References
Mellinghoff, S. C. et al. Primary prophylaxis of invasive fungal infections in patients with haematological malignancies: 2017 update of the recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society for Haematology and Medical Oncology (DGHO). Ann. Hematol. 97, 197–207 (2018).
Ullmann, A. J. et al. Infectious diseases in allogeneic haematopoietic stem cell transplantation: prevention and prophylaxis strategy guidelines 2016. Ann. Hematol. 95, 1435–1455 (2016).
Tomblyn, M. et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol. Blood Marrow Transpl. 15, 1143–1238 (2009).
Slavin, M. A. et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation—a prospective, randomized, double-blind study. J. Infect. Dis. 171, 1545–1552 (1995).
Goodman, J. L. et al. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N. Engl. J. Med. 326, 845–851 (1992).
van Burik, J. A. et al. Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin. Infect. Dis. 39, 1407–1416 (2004).
Peled, J. U. et al. Microbiota as predictor of mortality in allogeneic hematopoietic-cell transplantation. N. Engl. J. Med. 382, 822–834 (2020).
Morjaria, S. et al. Antibiotic-induced shifts in fecal microbiota density and composition during hematopoietic stem cell transplantation. Infect. Immun. 87, e00206–19 (2019).
Holler, E. et al. Metagenomic analysis of the stool microbiome in patients receiving allogeneic stem cell transplantation: loss of diversity is associated with use of systemic antibiotics and more pronounced in gastrointestinal graft-versus-host disease. Biol. Blood Marrow Transpl. 20, 640–645 (2014).
Taur, Y. et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin. Infect. Dis. 55, 905–914 (2012).
Ubeda, C. et al. Vancomycin-resistant Enterococcus domination of intestinal microbiota is enabled by antibiotic treatment in mice and precedes bloodstream invasion in humans. J. Clin. Invest. 120, 4332–4341 (2010).
Stein-Thoeringer, C. K. et al. Lactose drives Enterococcus expansion to promote graft-versus-host disease. Science 366, 1143–1149 (2019).
Stoma, I. et al. Compositional flux within the intestinal microbiota and risk for bloodstream infection with gram-negative bacteria. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa068 (2020).
Tamburini, F. B. et al. Precision identification of diverse bloodstream pathogens in the gut microbiome. Nat. Med. 24, 1809–1814 (2018).
Zhai, B. et al. High-resolution mycobiota analysis reveals dynamic intestinal translocation preceding invasive candidiasis. Nat. Med. 26, 59–64 (2020).
Marr, K. A. et al. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Blood 96, 2055–2061 (2000).
van der Velden, W. J. et al. Role of the mycobiome in human acute graft-versus-host disease. Biol. Blood Marrow Transpl. 19, 329–332 (2013).
Jain, U. et al. Debaryomyces is enriched in Crohn’s disease intestinal tissue and impairs healing in mice. Science 371, 1154–1159 (2021).
Limon, J. J. et al. Malassezia is associated with Crohn’s disease and exacerbates colitis in mouse models. Cell Host Microbe 25, 377–388(2019).
Leonardi, I. et al. Fungal trans-kingdom dynamics linked to responsiveness to fecal microbiota transplantation (FMT) therapy in ulcerative colitis. Cell Host Microbe 27, 823–829 (2020).
Sorror, M. L. et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106, 2912–2919 (2005).
Liu, C. M. et al. FungiQuant: a broad-coverage fungal quantitative real-time PCR assay. BMC Microbiol. 12, 255 (2012).
Chao, A., Chazdon, R. L., Colwell, R. K. & Shen, T. J. A new statistical approach for assessing similarity of species composition with incidence and abundance data. Ecol. Lett. 8, 148–159 (2005).
Faith, J. J. et al. The long-term stability of the human gut microbiota. Science 341, 1237439 (2013).
Nilsson, R. H. et al. Mycobiome diversity: high-throughput sequencing and identification of fungi. Nat. Rev. Microbiol. 17, 95–109 (2019).
Copelan, E. et al. A scheme for defining cause of death and its application in the T cell depletion trial. Biol. Blood Marrow Transpl. 13, 1469–1476 (2007).
Nash, A. K. et al. The gut mycobiome of the Human Microbiome Project healthy cohort. Microbiome 5, 153 (2017).
Auchtung, T. A. et al. Investigating colonization of the healthy adult gastrointestinal tract by fungi. mSphere 3, e00092-18 (2018).
Ikeda, F. et al. Antifungal activity of micafungin against Candida and Aspergillus spp. isolated from pediatric patients in Japan. Med Mycol. 47, 145–148 (2009).
Marti-Carrizosa, M., Sanchez-Reus, F., March, F., Canton, E. & Coll, P. Implication of Candida parapsilosis FKS1 and FKS2 mutations in reduced echinocandin susceptibility. Antimicrob. Agents Chemother. 59, 3570–3573 (2015).
Pfaller, M. A. et al. Correlation of MIC with outcome for Candida species tested against caspofungin, anidulafungin, and micafungin: analysis and proposal for interpretive MIC breakpoints. J. Clin. Microbiol. 46, 2620–2629 (2008).
Weber, D. et al. Microbiota disruption induced by early use of broad-spectrum antibiotics is an independent risk factor of outcome after allogeneic stem cell transplantation. Biol. Blood Marrow Transpl. 23, 845–852 (2017).
Shono, Y. et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci. Transl. Med. 8, 339ra371 (2016).
Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature 486, 207–214 (2012).
Koh, A. Y., Kohler, J. R., Coggshall, K. T., Van Rooijen, N. & Pier, G. B. Mucosal damage and neutropenia are required for Candida albicans dissemination. PLoS Pathog. 4, e35 (2008).
Garcia, C. et al. The human gut microbial metabolome modulates fungal growth via the TOR signaling pathway. mSphere https://doi.org/10.1128/mSphere.00555-17 (2017).
Fan, D. et al. Activation of HIF-1alpha and LL-37 by commensal bacteria inhibits Candida albicans colonization. Nat. Med. 21, 808–814 (2015).
Santus, W., Devlin, J.R. & Behnsen, J. Crossing kingdoms: how the mycobiota and fungal-bacterial interactions impact host health and disease. Infect. Immun. https://doi.org/10.1128/IAI.00648-20 (2021).
Allonsius, C. N. et al. Interplay between Lactobacillus rhamnosus GG and Candida and the involvement of exopolysaccharides. Microb. Biotechnol. 10, 1753–1763 (2017).
Graham, C. E., Cruz, M. R., Garsin, D. A. & Lorenz, M. C. Enterococcus faecalis bacteriocin EntV inhibits hyphal morphogenesis, biofilm formation, and virulence of Candida albicans. Proc. Natl Acad. Sci. USA 114, 4507–4512 (2017).
Taur, Y. et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood 124, 1174–1182 (2014).
Jenq, R. R. et al. Intestinal blautia Is associated with reduced death from graft-versus-host disease. Biol. Blood Marrow Transpl. 21, 1373–1383 (2015).
Findley, K. et al. Topographic diversity of fungal and bacterial communities in human skin. Nature 498, 367–370 (2013).
Gaitanis, G., Magiatis, P., Hantschke, M., Bassukas, I. D. & Velegraki, A. The Malassezia genus in skin and systemic diseases. Clin. Microbiol. Rev. 25, 106–141 (2012).
Taur, Y. et al. Reconstitution of the gut microbiota of antibiotic-treated patients by autologous fecal microbiota transplant. Sci. Transl. Med. 10, eaap9489 (2018).
Nilsson, R. H. et al. The UNITE database for molecular identification of fungi: handling dark taxa and parallel taxonomic classifications. Nucleic Acids Res. 47, D259–D264 (2019).
Benson, D. A. et al. GenBank. Nucleic Acids Res. 45, D37–D42 (2017).
McMurdie, P. J. & Holmes, S. Phyloseq: a bioconductor package for handling and analysis of high-throughput phylogenetic sequence data. Biocomputing 2012, 235–246 (2011).
Rolling, T., Zhai, B., Frame, J. V., Hohl, T. M. & Taur, Y. Customization of a dada2-based pipeline for fungal Internal Transcribed Spacer 1 (ITS 1) amplicon datasets. Preprint at bioRxiv https://doi.org/10.1101/2021.07.19.452952 (2021).
Acknowledgements
This work was supported by Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) grant no. RO-5328/1-2 (to T.R.), National Institutes of Health (NIH) grant nos. R01 AI093808 (T.M.H.), R21 AI105617 (T.M.H.), R21 AI156157 (T.M.H.), U01 AI124275 (J.B.X.), R01 AI137269 (J.B.X. and Y.T.), K08 HL143189 (J.U.P.), R01 CA228358 (M.R.M.v.d.B.), R01 CA228308 (M.R.M.v.d.B.), P01 CA023766 (M.R.M.v.d.B.), R01 HL125571 (M.R.M.v.d.B.), R01 HL123340 (M.R.M.v.d.B.), P01 AG052359 (Project 2, M.R.M.v.d.B.), a Takeda Science Foundation-Fellowship (K.Y.M.), an Investigator in the Pathogenesis of Infectious Diseases Award from the Burroughs Wellcome Fund (T.M.H.), the Ludwig Center for Cancer Immunotherapy (T.M.H.), a Tri-Institutional Stem Cell Initiative award no. 2016-013 (M.R.M.v.d.B.), the Lymphoma Foundation (M.R.M.v.d.B.), the Parker Institute for Cancer Immunotherapy at MSKCC (M.R.M.v.d.B., K.A.M. and J.U.P.), the Susan and Peter Solomon Divisional Genomics Program (T.M.H. and M.R.M.v.d.B.) and the DKMS (K.A.M.). All authors were supported by NIH P30 CA008748 (Cancer Center Core Grant).
Author information
Authors and Affiliations
Contributions
The study was conceived by T.R., B.Z. and T.M.H. Clinical data were collected by D.M.P., M.A.P., M.R.M.v.d.B., K.A.M., J.U.P., Y.T. and T.M.H. Data analysis and visualization were conducted by T.R., with assistance from B.Z., J.B.X., Y.T. and J.U.P. Sample processing was done by T.R., B.Z., M.G., N.T., K.Y.M., E.F., L.A.A. and R.J.W. The manuscript was written by T.R. and T.M.H. All co-authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.U.P. reports research funding, intellectual property fees and travel reimbursement from Seres Therapeutics and consulting fees from DaVolterra, CSL Behring and from Maat Pharma. He has filed intellectual property applications related to the microbiome (reference nos. 62/843,849, 62/977,908 and 15/756,845). M.R.M.v.d.B. has received research support from Seres Therapeutics; he has consulted, received honorarium from or participated in advisory boards for Seres Therapeutics, WindMIL Therapeutics, Rheos, Frazier Healthcare Partners, Nektar Therapeutics, Notch Therapeutics, Forty Seven Inc., Priothera, Ceramedix, Lygenesis, Pluto Immunotherapeutics, Magenta Therapeutics, Merck & Co., Inc. and DKMS Medical Council (Board); and he has IP Licensing with Seres Therapeutics, Juno Therapeutics and stock options from Seres and Notch Therapeutics. T.M.H. has participated in a scientific advisory board for Boehringer-Ingelheim Inc.
Additional information
Peer review information Nature Microbiology thanks Scott Filler and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
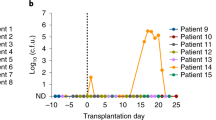
Extended Data Fig. 1 Impact of culture positivity and TPN administration on fungal and bacterial microbiota dynamics during allo-HCT, related to Fig. 1.
(a) Comparison of fungal density per gram of stool (n = 246 pre-transplant samples and n = 978 post-transplant samples) and (b) fungal diversity (n = 251 pre-transplant samples and n = 1028 post-transplant samples) between the pre- (days -10 to -1) and the post-transplant period (days 0 to 30). (c) Comparison of bacterial density per gram of stool (n = 241 pre-transplant samples and n = 976 post-transplant samples) and (d) diversity (n = 245 pre-transplant samples and n = 939 post-transplant samples) between the pre- and post-transplant period. Statistical tests (a–d): Two-sided P-values issued from generalized estimating equations with patient ID as cluster variable are shown. The upper whisker represents the maximum value or the 75th percentile value plus 1.5 times the IQR, whichever is larger. The lower whisker represents the minimum value or the 25th percentile value minus 1.5 times the IQR.
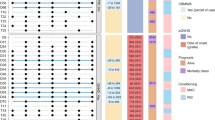
Extended Data Fig. 2 Taxonomic composition and relation to culture positivity, related to Fig. 3.
(a) Taxonomic composition of culture-positive samples by ITS (top ribbon) and species cultured from the respective samples (bottom ribbon). (b) Comparison of fungal similarity (1 − Chao–Jaccard index) according to presence of fungal domination status of the earliest sample. Each dot represents a sample pair of an individual patient collected one day apart (n = 516 sample pairs). (c) Comparison of fungal similarity (1 − Chao–Jaccard index) according to the taxa responsible for fungal domination in the earliest samples. Each dot represents a sample pair of an individual patient collected one day apart (n = 88 sample pairs). (b–c) Two-sided p-values issued from generalized estimating equations with patient ID as cluster variable without accounting for multiple comparisons are shown. The upper whisker represents the maximum value or the 75th percentile value plus 1.5 times the IQR, whichever is larger. The lower whisker represents the minimum value or the 25th percentile value minus 1.5 times the IQR.
Extended Data Fig. 3 Supplementary data for clinical outcomes and the fungal intestinal mycobiota, related to Fig. 5.
(a) Overall survival and (b) transplant-related mortality in relation to a relative abundance of C. parapsilosis complex ≥ 82% within the pre-engraftment period (days 0 to the first day of an absolute neutrophil count > 500/mm3). (a) Kaplan–Meier curves tested by two-sided log-rank test. (b) Cumulative incidence curves with relapse and progression of primary disease as competing interest. Differences tested by two-sided Gray’s test. (c) Overall survival and (d) transplant-related mortality in relation to domination by C. albicans within the pre-engraftment period (days 0 to the first day of an absolute neutrophil count > 500/mm3). (c) Kaplan–Meier curves tested by two-sided log-rank test. (d) Cumulative incidence curves with relapse and progression of primary disease as competing interest. Differences tested by two-sided Gray’s test. (a–d) Numbers below the graphs correspond to the number of patients (still) at risk at the specific time point.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2.
Supplementary Data
Source data of patients and samples including accession numbers.
Rights and permissions
About this article
Cite this article
Rolling, T., Zhai, B., Gjonbalaj, M. et al. Haematopoietic cell transplantation outcomes are linked to intestinal mycobiota dynamics and an expansion of Candida parapsilosis complex species. Nat Microbiol 6, 1505–1515 (2021). https://doi.org/10.1038/s41564-021-00989-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-021-00989-7
This article is cited by
-
Insights into gut microbiomes in stem cell transplantation by comprehensive shotgun long-read sequencing
Scientific Reports (2024)
-
Invasive candidiasis
Nature Reviews Disease Primers (2024)
-
Candida parapsilosis complex in the clinical setting
Nature Reviews Microbiology (2024)
-
Bacteria and bacteriophage consortia are associated with protective intestinal metabolites in patients receiving stem cell transplantation
Nature Cancer (2024)
-
Immune responses to human fungal pathogens and therapeutic prospects
Nature Reviews Immunology (2023)