Abstract
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in Wuhan, Hubei Province, China in late December 2019. We re-analysed 640 throat swabs collected from patients in Wuhan with influenza-like-illness from 6 October 2019 to 21 January 2020 and found that 9 of the 640 throat swabs were positive for SARS-CoV-2 RNA by quantitative PCR, suggesting community transmission of SARS-CoV2 in Wuhan in early January 2020.
Similar content being viewed by others
Main
The coronavirus disease 2019 (COVID-19) outbreak, which originated from Wuhan, Hubei Province, China, has spread to all of the provinces of China and 28 other countries1. As of 23 February 2020, more than 77,000 cases of SARS-CoV-2 infection have been confirmed in China and 60% of these were reported in Wuhan. Its causative pathogen is a phylogenetic sister to the severe acute respiratory syndrome coronavirus (SARS-CoV) and has been designated as SARS-CoV-2 (ref. 2). However, although SARS-CoV-2 shares 79.6% sequence identity and the same cell receptor with SARS-CoV3,4, the clinical outcome of SARS-CoV-2 not only includes SARS-like viral pneumonia5, but also covers milder illness, even asymptomatic infection6,7. In fact, analysis by the China CDC indicated that 80.9% of confirmed COVID-19 cases were characterized as the mild or moderate types—that is, without breathing difficulty and hypoxia7.
Wuhan is the largest city in central China, with a resident population of over fourteen million. The rapid increase in reported cases suggests that community transmission of SARS-CoV-2 had established in the city of Wuhan and nearby regions no later than the end of January8. As the rapid molecular diagnostic assay was not available in early January and widespread use was difficult before 23 January 2020, it was difficult to monitor the transmission of SARS-CoV-2 among the community.
To better understand the current epidemic in Wuhan, particularly the status of cases of milder illness, we retrospectively investigated the presence of SARS-CoV-2 among local patients with influenza-like illness (ILI), which were defined as outpatients with a sudden onset of a fever of >38 °C and a cough or sore throat. Sustained sentinel surveillance for ILI cases and their aetiology has been implemented in Wuhan since 2005, based on the National Influenza Surveillance Network of China9. Two representative referral hospitals were selected as sentinel hospitals to reflect the trends in ILI in the local population (Supplementary Fig. 1): the Children’s Hospital of Wuhan, which is the largest paediatric centre in the province, and Wuhan No. 1 Hospital, a major general hospital with over two million outpatient visits per year. The number of ILI cases and total outpatient numbers were reported weekly by the sentinel hospitals, and clinical samples were also collected from ILI patients. In this study, 640 throat swabs collected from ILI patients in the 16-week period between 6 October 2019 (week (W) 40 of 2019; 2019W40 hereafter) and 21 January 2020 (2020W03) were re-analysed.
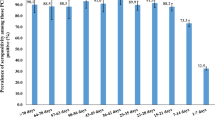
The time period in concern coincided with the winter peak of influenza and other respiratory illnesses. The number of ILI cases in all age groups increased dramatically starting in early December and reached the peak by the New Year (Fig. 1a). In particular, the 5–14 yr group increased over 24-fold during this period (2019W40–W47, 75 cases per week; 2019W52, 1,916 cases). The percentage of ILI patients in all outpatients experienced a similar rise: the average percentage was 1.07% during 2019W40–W47 and soared up to 9.44% in 2020W01. In addition, ILI data for the 2019–2020 winter was significantly higher in comparison to previous years (Fig. 1b,c and Source Data Fig. 1), suggesting the necessity to distinguish between influenza-infected and suspected COVID-19 patients.
a, Number of ILI cases and percentage of outpatients with ILI between 6 October 2019 and 21 January 2020 (2019W40 to 2020W03). The vertical columns scaled on the left y axis report the weekly ILI case numbers and the colour blocks in the columns represent the different age groups of the patients with ILI. The dashed line shows the percentage of outpatients with ILI and is scaled on the right y axis. b, Number of ILI cases that occurred during the winter influenza season of the past three years. c, Percentage of ILI during the winter influenza season of the past three years. b,c, Data from week 40 to week 12 of the following year are presented, except for 2019–2020 as the ILI surveillance was suspended to handle the COVID-19 epidemic.
The patients with ILI participating in this study comprised 315 males and 325 females, ranging in age from 9 months to 87 yr (median age, 8 yr; mean age, 22.7 yr). SARS-CoV-2 RNA was detected in nine patient specimens (Table 1 and Extended Data Fig. 1), all of which were collected in January 2020 (2020W01–W03) when the seasonal influenza (mainly A/H3 and B/Victoria) remained active; however, no coinfection was detected.
The basic demographic information and illness timeline of the nine patients infected with SARS-CoV-2 is listed in Extended Data Fig. 2. The gender ratio was 1.25 (five males versus four females), and they were all adults (age range: 35–71 yr). These demographic features are consistent with other available reports regarding patients with COVID-19 (refs. 5,7,10). The onset date of the earliest case was 4 January 2020, one week after the outbreak was reported by hospitals11. The average gap between onset and seeking medical help was 1.7 d, which is shorter than a previous report on early diagnosed cases that typically have pneumonia5,11. Although the weekly sample size was small, it seems that COVID-19 was gradually expanding among the ILI cases during January. In the last week of observation, the frequency of SARS-CoV-2-positive cases had exceeded that of influenza virus among the group of patients older than 30 yr (Table 1). This finding is consistent with the recent epidemiological estimations about the early transmission dynamics of SARS-CoV-2 (refs. 11,12). Interestingly, the nine patients with COVID-19 came from six different districts of the Wuhan metropolitan and surrounding areas (Supplementary Fig. 1), which provided additional evidence for community transmission in this region.
According to its definition, the clinical manifestation of ILI overlaps with the mild/moderate type of COVID-19, which is defined as both non-pneumonia and pneumonia cases without dyspnoea and hypoxia7. The ILI surveillance samples thus provided us a unique opportunity to investigate the early expansion of SARS-CoV-2 in the local population. A main concern was the representativeness of these samples. The two sentinel hospitals in Wuhan were both highly reputable public hospitals with large catchment populations. They were located downtown and could be easily accessed from the whole metropolitan area through public transportation (Supplementary Fig. 1). In addition, China has achieved universal basic health insurance in the lack of hierarchical medical system13, making large public hospitals the priority choice of patients, which minimized the selection of symptom severity in this study.
There is some discussion regarding the reliability of the SARS-CoV-2 quantitative PCR test and the applicability of upper respiratory tract specimens, including throat swab14,15; however, in this study, the possibility of false negative results will not weaken the main finding that SARS-CoV-2 was present in January in patients with ILI. As the epidemic developed rapidly, the ILI surveillance in Wuhan was suspended in 2020W04, because both the CDC virology laboratory and the sentinel hospitals were reformed to focus on handling the explosive medical needs of COVID-19. By the time this manuscript was revised, the number of cases confirmed daily in Wuhan had begun to decline following one month of traffic restrictions. There is an urgent need for a systematic population serological investigation to reveal the full status as well as the history of COVID-19.
In summary, our work adds information to the understanding of the early stage of the current epidemic. The detection of SARS-CoV-2 cases among local patients with ILI suggests that community transmission was established in Wuhan early in January. Concerning the recent outbreaks happening on the Diamond Princess Cruise ship and Daequ, South Korea, we suggest strengthening the pathogen surveillance of ILI cases in all regions facing the danger of SARS-CoV-2 community transmission.
Methods
Sample and information collection
The ILI statistics and throat swab samples for this study were collected during the routine ILI surveillance of two national influenza sentinel hospitals in Wuhan. A patient was identified as an ILI case in the outpatient department of both hospitals if they had a sudden onset of a fever >38 °C as well as a cough or sore throat, according to the latest National Influenza Surveillance Plan16. The number of ILI cases and total outpatient numbers were collected weekly. Clinical samples of patients with ILI were also collected if the patient had a fever for less than 3 d and had not been treated with antiviral drugs. After verbal informed consent was obtained from parents or caretakers of underage patients, throat swabs were collected from patients with ILI in 3.5 ml viral transport medium and delivered to the Wuhan Center for Disease Prevention and Control for laboratory diagnosis of the influenza virus. Each sentinel hospital was required to collect 20 ILI samples every calendar week.
Detection of SARS-CoV-2 and influenza virus by real-time PCR with reverse transcription
We performed a commercial quantitative PCR assay (BioGerm) approved by the China CDC and National Medical Products Administration to detect the presence of SARS-CoV-2 in the throat swab specimens of patients with ILI. The targets of this assay were both the ORF1ab and N gene of SARS-CoV-2, and the detection limit was 1,000 copies ml−1. The nucleic acids used in the SARS-CoV-2 detection were initially extracted from 200 μl of throat swabs medium using a PANA9600E automated nucleic acid extraction system (Tianlong). They had being employed for the detection and subtyping of influenza virus17, and were well kept at −70 °C before the SARS-CoV-2 experiments. All assays have been established in our laboratory and the procedures were performed following the manufacturers’ instructions. For the specific primers and probes used in the influenza virus detection, refer to Supplementary Table 1.
Approval for patient recruitment
This study was reviewed and approved by the Ethics Committee of the Wuhan Center for Disease Prevention and Control. Verbal informed consent was obtained from parents or caretakers of underage patients.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Source data for Fig. 1 are provided with the paper.
References
Coronavirus Disease 2019 (COVID-19) Situation Report 33 (World Health Organization, 2020).
Gorbalenya, A. E. et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 5, 536–544 (2020).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506 (2020).
Chan, J. F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395, 514–523 (2020).
The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly 2, 113–122 (2020).
Epidemic Update and Risk Assessment of 2019 Novel Coronavirus (Chinese Center for Disease Control and Prevention, 2020).
Yang, P. et al. Review of an influenza surveillance system, Beijing, People’s Republic of China. Emerg. Infect. Dis. 15, 1603–1608 (2009).
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069 (2020).
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 323, 1199–1207 (2020).
Wu, J. T., Leung, K. & Leung, G. M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 395, 689–697 (2020).
Li, L. & Fu, H. China’s health care system reform: progress and prospects. Int. J. Health Plann. Manage. 32, 240–253 (2017).
Wang, M. et al. Clinical diagnosis of 8274 samples with 2019-novel coronavirus in Wuhan. Preprint at medRxiv https://doi.org/10.1101/2020.02.12.20022327 (2020).
Zou, L. et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 382, 1177–1179 (2020).
Shi, W. et al. Co-circulation and persistence of multiple A/H3N2 influenza variants in China. Emerg. Microbes Infect. 8, 1157–1167 (2019).
Peng, J. et al. The epidemiology and etiology of influenza-like illness in Chinese children from 2008 to 2010. J. Med. Virol. 84, 672–678 (2012).
Acknowledgements
We thank the doctors who were responsible for collecting specimens at the Children’s Hospital of Wuhan and Wuhan No. 1 Hospital. This work was supported by the Emergency Scientific Research Project for COVID-19 from Wuhan City to M.-Q.L.
Author information
Authors and Affiliations
Contributions
W.-H.K. analysed the data and prepared the manuscript. Y.L. and M.-W.P. conducted the experiments for the detection of influenza and SARS-CoV-2. D.-G.K. and X.-B.Y. collected the specimens and epidemic information. L.W. analysed the data and critically revised the manuscript. M.-Q.L. conducted the SARS-CoV-2 detection, analysed the data and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1
Demographic information of tested ILI patients collected in Wuhan between 6 October 2019 and 21 January 2020 (2019W40 to 2020W03).
Extended Data Fig. 2
Demographic information and illness timeline of nine SARS-CoV-2 infected ILI patients in Wuhan.
Supplementary information
Supplementary Information
Supplementary Table 1 and Supplementary Fig. 1.
Source data
Source Data Fig. 1
Source data for Fig. 1.
Rights and permissions
About this article
Cite this article
Kong, WH., Li, Y., Peng, MW. et al. SARS-CoV-2 detection in patients with influenza-like illness. Nat Microbiol 5, 675–678 (2020). https://doi.org/10.1038/s41564-020-0713-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-020-0713-1
This article is cited by
-
CNN-IKOA: convolutional neural network with improved Kepler optimization algorithm for image segmentation: experimental validation and numerical exploration
Journal of Big Data (2024)
-
Interventions to support mental health in people with long COVID: a scoping review
BMC Public Health (2023)
-
Exploring the pharmacological aspects of natural phytochemicals against SARS-CoV-2 Nsp14 through an in silico approach
In Silico Pharmacology (2023)
-
Dual-mode SERS-based lateral flow assay strips for simultaneous diagnosis of SARS-CoV-2 and influenza a virus
Nano Convergence (2022)
-
The clinical association between Periodontitis and COVID-19
Clinical Oral Investigations (2022)