Abstract
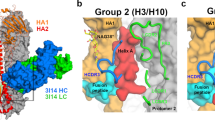
Little is known about the specificities and neutralization breadth of the H7-reactive antibody repertoire induced by natural H7N9 infection in humans. We have isolated and characterized 73 H7-reactive monoclonal antibodies from peripheral B cells from four donors infected in 2013 and 2014. Of these, 45 antibodies were H7-specific, and 17 of these neutralized the virus, albeit with few somatic mutations in their variable domain sequences. An additional set of 28 antibodies, isolated from younger donors born after 1968, cross-reacted between H7 and H3 haemagglutinins in binding assays, and had accumulated significantly more somatic mutations, but were predominantly non-neutralizing in vitro. Crystal structures of three neutralizing and protective antibodies in complex with the H7 haemagglutinin revealed that they recognize overlapping residues surrounding the receptor-binding site of haemagglutinin. One of the antibodies, L4A-14, bound into the sialic acid binding site and made contacts with haemagglutinin residues that were conserved in the great majority of 2016–2017 H7N9 isolates. However, only 3 of the 17 neutralizing antibodies retained activity for the Yangtze River Delta lineage viruses isolated in 2016–2017 that have undergone antigenic change, which emphasizes the need for updated H7N9 vaccines.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding authors upon request. Atomic coordinates for the H7-FabL4A-14, H7-FabL4B-18 and H7-FabL3A-44 complex as well as structure factors have been deposited to the Protein Data Bank under accession codes 6II4, 6II8 and 6II9.
References
Wang, X. et al. Epidemiology of avian influenza A H7N9 virus in human beings across five epidemics in mainland China, 2013–17: an epidemiological study of laboratory-confirmed case series. Lancet Infect. Dis. 17, 822–832 (2017).
Shi, J. et al. H7N9 virulent mutants detected in chickens in China pose an increased threat to humans. Cell Res. 27, 1409–1421 (2017).
Yang, L. et al. Genesis and spread of newly emerged highly pathogenic H7N9 avian viruses in mainland China. J. Virol. 91, e01277-17 (2017).
Zhang, F. et al. Human infections with recently-emerging highly pathogenic H7N9 avian influenza virus in China. J. Infect. 75, 71–75 (2017).
Zhu, W. et al. Biological characterisation of the emerged highly pathogenic avian influenza (HPAI) A(H7N9) viruses in humans, in mainland China, 2016 to 2017. Euro. Surveill. 22, 30533 (2017).
Qi, W. et al. Emergence and adaptation of a novel highly pathogenic H7N9 influenza virus in birds and humans from a 2013 human-infecting low-pathogenic ancestor. J. Virol. 92, e00921-17 (2018).
Gao, R. et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N. Engl. J. Med. 368, 1888–1897 (2013).
Hu, Y. et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 381, 2273–2279 (2013).
Hai, R. et al. Influenza A(H7N9) virus gains neuraminidase inhibitor resistance without loss of in vivo virulence or transmissibility. Nat. Commun. 4, 2854 (2013).
Lin, P. H. et al. Virological, serological, and antiviral studies in an imported human case of avian influenza A(H7N9) virus in Taiwan. Clin. Infect. Dis. 58, 242–246 (2014).
Marjuki, H. et al. Neuraminidase mutations conferring resistance to oseltamivir in influenza A(H7N9) viruses. J. Virol. 89, 5419–5426 (2015).
Imai, M. et al. A highly pathogenic avian H7N9 influenza virus isolated from a human is lethal in some ferrets infected via respiratory droplets. Cell Host Microbe 22, 615–626 (2017).
Subbarao, K. Avian influenza H7N9 viruses: a rare second warning. Cell Res. 28, 1–2 (2018).
Summary of Influenza Risk Assessment Tool (IRAT) Results Web Site (Centers for Disease Control and Prevention, accessed 2 May 2018); https://www.cdc.gov/flu/pandemic-resources/monitoring/irat-virus-summaries.htm.
Wang, D. et al. Two outbreak sources of influenza A (H7N9) viruses have been established in China. J. Virol. 90, 5561–5573 (2016).
Kile, J. C. et al. Update: increase in human infections with novel Asian lineage avian influenza A(H7N9) viruses during the fifth epidemic—China, October 1, 2016–August 7, 2017. MMWR. Morb. Mortal. Wkly Rep. 66, 928–932 (2017).
Gostic, K. M., Ambrose, M., Worobey, M. & Lloyd-Smith, J. O. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science 354, 722–726 (2016).
Ekiert, D. C. et al. A highly conserved neutralizing epitope on group 2 influenza A viruses. Science 333, 843–850 (2011).
Guo, L. et al. Human antibody responses to avian influenza A(H7N9) virus, 2013. Emerg. Infect. Dis. 20, 192–200 (2014).
Dunand, C. J. et al. Preexisting human antibodies neutralize recently emerged H7N9 influenza strains. J. Clin. Invest. 125, 1255–1268 (2015).
Kallewaard, N. L. et al. Structure and function analysis of an antibody recognizing all influenza A subtypes. Cell 166, 596–608 (2016).
Yamayoshi, S. et al. Human protective monoclonal antibodies against the HA stem of group 2 HAs derived from an H3N2 virus-infected human. J. Infect. 76, 177–185 (2018).
Stadlbauer, D. et al. Vaccination with a recombinant H7 hemagglutinin-based influenza virus vaccine induces broadly reactive antibodies in humans. mSphere 2, e00502-17 (2017).
Stadlbauer, D., Nachbagauer, R., Meade, P. & Krammer, F. Universal influenza virus vaccines: what can we learn from the human immune response following exposure to H7 subtype viruses? Front. Med. 11, 471–479 (2017).
Andrews, S. F. et al. Preferential induction of cross-group influenza A hemagglutinin stem-specific memory B cells after H7N9 immunization in humans. Sci. Immunol. 2, eaan2676 (2017).
Wang, Z. et al. Recovery from severe H7N9 disease is associated with diverse response mechanisms dominated by CD8+ T cells. Nat. Commun. 6, 6833 (2015).
Baz, M. et al. Nonreplicating influenza A virus vaccines confer broad protection against lethal challenge. mBio 6, e01487-15 (2015).
Sutton, T. C. et al. Protective efficacy of influenza group 2 hemagglutinin stem-fragment immunogen vaccines. NPJ Vaccines 2, 35 (2017).
Sobhanie, M. et al. Evaluation of the safety and immunogenicity of a candidate pandemic live attenuated influenza vaccine (pLAIV) against influenza A(H7N9). J. Infect. Dis. 213, 922–929 (2016).
Dunand, C. J. et al. Both neutralizing and non-neutralizing human H7N9 influenza vaccine-induced monoclonal antibodies confer protection. Cell Host Microbe 19, 800–813 (2016).
Powell, T. J., Silk, J. D., Sharps, J., Fodor, E. & Townsend, A. R. Pseudotyped influenza A virus as a vaccine for the induction of heterotypic immunity. J. Virol. 86, 13397–13406 (2012).
Burke, D. F. & Smith, D. J. A recommended numbering scheme for influenza A HA subtypes. PLoS ONE 9, e112302 (2014).
Thornburg, N. J. et al. H7N9 influenza virus neutralizing antibodies that possess few somatic mutations. J. Clin. Invest. 126, 1482–1494 (2016).
Matrosovich, M., Matrosovichm, T., Carr, J., Roberts, N. A. & Klenk, H. D. Overexpression of the alpha-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77, 8418–8425 (2003).
Wiley, D. C. & Skehel, J. J. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu. Rev. Biochem. 56, 365–394 (1987).
Chen, C. et al. Structural insight into a human neutralizing antibody against influenza virus H7N9. J. Virol. 92, e01850-17 (2018).
Shi, Y. et al. Structures and receptor binding of hemagglutinins from human-infecting H7N9 influenza viruses. Science 342, 243–247 (2013).
Ohshima, N. et al. Naturally occurring antibodies in humans can neutralize a variety of influenza virus strains, including H3, H1, H2, and H5. J. Virol. 85, 11048–11057 (2011).
Lee, P. S. et al. Receptor mimicry by antibody F045-092 facilitates universal binding to the H3 subtype of influenza virus. Nat. Commun. 5, 3614 (2014).
McCarthy, K. R. et al. Memory B cells that cross-react with Group 1 and Group 2 influenza A viruses are abundant in adult human repertoires. Immunity 48, 174–184 (2018).
Ekiert, D. C. et al. Cross-neutralization of influenza A viruses mediated by a single antibody loop. Nature 489, 526–532 (2012).
Huang, K. Y. et al. Focused antibody response to influenza linked to antigenic drift. J. Clin. Invest. 125, 2631–2645 (2015).
Smith, K. et al. Rapid generation of fully human monoclonal antibodies specific to a vaccinating antigen. Nat. Protoc. 4, 372–384 (2009).
Xiao, J. H. et al. Characterization of influenza virus pseudotyped with Ebolavirus glycoprotein. J. Virol. 92, e00941-17 (2018).
Martínez-Sobrido, L. et al. Hemagglutinin-pseudotyped green fluorescent protein-expressing influenza viruses for the detection of influenza virus neutralizing antibodies. J. Virol. 84, 2157–2163 (2010).
Rowe, T. et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J. Clin. Microbiol. 37, 937–943 (1999).
Peacock, T. et al. Antigenic mapping of an H9N2 avian influenza virus reveals two discrete antigenic sites and a novel mechanism of immune escape. Sci. Rep. 6, 18745 (2016).
Zhang, W. et al. Crystal structure of the swine-origin A (H1N1)-2009 influenza A virus hemagglutinin (HA) reveals similar antigenicity to that of the 1918 pandemic virus. Protein Cell 1, 459–467 (2010).
Aad, G. et al. Search for new particles in two-jet final states in 7Â TeV proton-proton collisions with the ATLAS detector at the LHC. Phys. Rev. Lett. 105, 161801 (2010).
Yang, J.-R. et al. Characterization of influenza A (H7N9) viruses isolated from human cases imported into Taiwan. PLoS ONE 10, e0119792 (2015).
Acknowledgements
The authors acknowledge support from the laboratories that provided the sequences of reference antibody MEDI885221 for the comparisons in the tables and figures. The authors also acknowledge the BD FACSAria cell sorter service provided by the Core Instrument Center of Chang Gung University, and C. Waugh for FACS sorting B cells and MDCK-SIAT1 cell lines at WIMM Oxford. These studies were funded by the Townsend-Jeantet Charitable Trust (registered charity no. 1011770), the Emergency Technology Research Issue on Prevention and Control for Human infection with A (H7N9) Avian Influenza Virus (10600100000015001206), the Strategic Priority Research Program of the Chinese Academy of Sciences (CAS) (XDB29010000), the National Science and Technology Major Project (2018ZX10101004), the Human Immunology Unit (MRC), Oxford University, Chang Gung Medical Research Program (CMRPG3G0921, CMRPG3G0922) and the Ministry of Science and Technology of Taiwan (MOST 104-2320-B-182A-002-MY2, MOST 105-2320-B-182A-008- and MOST 107-2321-B-182A-003-). G.F.G. is supported partly as a leading principal investigator of the NSFC Innovative Research Group (81621091). Y.S. is supported by the Excellent Young Scientist Program from the National Natural Science Foundation of China (81622031), the Excellent Young Scientist Program of CAS and the Youth Innovation Promotion Association CAS (2015078).
Author information
Authors and Affiliations
Contributions
K.-Y.A.H., G.F.G., Y.S. and A.R.T. conceived and designed the study. K.-Y.A.H., P.R., H.J., B.W., L.S., T.D., Y.-M.L., P.C., M.I., M.-C.W., Z.C., R.S., C.-C.H., J.-H.Y., J.Q., T.-Y.L., A.L., T.J.P., J.-T.J., C.M., G.F.G., Y.S. and A.R.T. carried out the experiments. K.-Y.A.H., P.R., H.J., B.W., L.S., T.D., Y.-M.L., J.-T.J., C.M., G.F.G., Y.S. and A.R.T. performed data analysis and figure/table preparation. K.-Y.A.H., P.R., G.F.G., Y.S. and A.R.T. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figures 1–8, Supplementary Tables 1–6.
Supplementary Table 1
Binding and neutralizing activities of of 73 H7-reactive monoclonal antibodies isolated from donors.
Supplementary table 2
Details of 73 H7-reactive monoclonal antibodies variable domain sequences isolated from donors.
Rights and permissions
About this article
Cite this article
Huang, KY.A., Rijal, P., Jiang, H. et al. Structure–function analysis of neutralizing antibodies to H7N9 influenza from naturally infected humans. Nat Microbiol 4, 306–315 (2019). https://doi.org/10.1038/s41564-018-0303-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-018-0303-7
This article is cited by
-
A protective measles virus-derived vaccine inducing long-lasting immune responses against influenza A virus H7N9
npj Vaccines (2023)
-
Nanobodies mapped to cross-reactive and divergent epitopes on A(H7N9) influenza hemagglutinin using yeast display
Scientific Reports (2021)
-
Designing a multi-epitope vaccine to provoke the robust immune response against influenza A H7N9
Scientific Reports (2021)
-
Avian influenza A (H7N9) virus: from low pathogenic to highly pathogenic
Frontiers of Medicine (2021)
-
Two doses of SARS-CoV-2 vaccination induce robust immune responses to emerging SARS-CoV-2 variants of concern
Nature Communications (2021)