Abstract
Chlamydia trachomatis, an obligate intracellular human pathogen, is a major cause of sexually transmitted diseases. Infections often occur without symptoms, a feature that has been attributed to the ability of the pathogen to evade the host immune response. We show here that C. trachomatis paralyses the host immune system by preventing the activation of polymorphic nuclear leukocytes (PMNs). PMNs infected with Chlamydia fail to produce neutrophil extracellular traps and the bacteria are able to survive in PMNs for extended periods of time. We have identified the secreted chlamydial protease-like activating factor (CPAF) as an effector mediating the evasion of the innate immune response since CPAF-deficient Chlamydia activate PMNs and are subsequently efficiently killed. CPAF suppresses the oxidative burst and interferes with chemical-mediated activation of neutrophils. We identified formyl peptide receptor 2 (FPR2) as a target of CPAF. FPR2 is cleaved by CPAF and released from the surface of PMNs. In contrast to previously described subversion mechanisms that mainly act on already activated PMNs, we describe here details of how Chlamydia actively paralyses PMNs, including the formation of neutrophil extracellular traps, to evade the host’s innate immune response.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 (2004).
Murphy, P. M. et al. A structural homologue of the N-formyl peptide receptor. Characterization and chromosome mapping of a peptide chemoattractant receptor family. J. Biol. Chem. 267, 7637–7643 (1992).
Kretschmer, D. et al. Human formyl peptide receptor 2 senses highly pathogenic Staphylococcus aureus. Cell Host Microbe 7, 463–473 (2010).
von Kockritz-Blickwede, M., Blodkamp, S. & Nizet, V. Interaction of bacterial exotoxins with neutrophil extracellular traps: impact for the infected host. Front. Microbiol. 7, 402 (2016).
Paavonen, J. & Eggert-Kruse, W. Chlamydia trachomatis: impact on human reproduction. Hum. Reprod. Update 5, 433–447 (1999).
Fleming, D. T. & Wasserheit, J. N. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex. Transm. Infect. 75, 3–17 (1999).
Vonck, R. A., Darville, T., O’Connell, C. M. & Jerse, A. E. Chlamydial infection increases gonococcal colonization in a novel murine coinfection model. Infect. Immun. 79, 1566–1577 (2011).
Herweg, J. A. & Rudel, T. Interaction of Chlamydiae with human macrophages. FEBS J. 283, 608–618 (2016).
Fischer, A. & Rudel, T. Subversion of cell-autonomous host defense by Chlamydia infection. Curr. Top. Microbiol. Immunol. https://doi.org/10.1007/82_2016_13 (2016).
Dicker, L. W., Mosure, D. J., Berman, S. M. & Levine, W. C. Gonorrhea prevalence and coinfection with chlamydia in women in the United States, 2000. Sex. Transm. Dis. 30, 472–476 (2003).
Criss, A. K. & Seifert, H. S. A bacterial siren song: intimate interactions between Neisseria and neutrophils. Nat. Rev. Microbiol. 10, 178–190 (2012).
Huang, Z. et al. Structural basis for activation and inhibition of the secreted chlamydia protease CPAF. Cell Host Microbe 4, 529–542 2008).
Saka, H. A. et al. Quantitative proteomics reveals metabolic and pathogenic properties of Chlamydia trachomatis developmental forms. Mol. Microbiol. 82, 1185–1203 (2011).
Chen, D. et al. Autoprocessing and self-activation of the secreted protease CPAF in Chlamydia-infected cells. Microb. Pathog. 49, 164–173 (2010).
Yang, Z., Tang, L., Zhou, Z., & Zhong, G. Autoprocessing and self-activation of the secreted protease CPAF in Chlamydia-infected cells. Microb. Pathog. 49, 164–173 (2010).
Tang, L. et al. Chlamydia-secreted protease CPAF degrades host antimicrobial peptides. Microbes Infect. 17, 402–408 (2015).
Yang, Z. et al. The Chlamydia-secreted protease CPAF promotes chlamydial survival in the mouse lower genital tract. Infect. Immun. 84, 2697–2702 (2016).
Snavely, E. A. et al. Reassessing the role of the secreted protease CPAF in Chlamydia trachomatis infection through genetic approaches. Pathog. Dis. 71, 336–351 (2014).
Frazer, L. C., O’Connell, C. M., Andrews, C. W. Jr, Zurenski, M. A. & Darville, T. Enhanced neutrophil longevity and recruitment contribute to the severity of oviduct pathology during Chlamydia muridarum infection. Infect. Immun. 79, 4029–4041 (2011).
Reeves, E. P. et al. Killing activity of neutrophils is mediated through activation of proteases by K+ flux. Nature 416, 291–297 (2002).
Daley, J. M., Thomay, A. A., Connolly, M. D., Reichner, J. S. & Albina, J. E. Use of Ly6G-specific monoclonal antibody to deplete neutrophils in mice. J. Leukoc. Biol. 83, 64–70 (2008).
Brinkmann, V. & Zychlinsky, A. Neutrophil extracellular traps: is immunity the second function of chromatin? J. Cell Biol. 198, 773–783 2012).
Pettit, E. J. & Hallett, M. B. Two distinct Ca2+ storage and release sites in human neutrophils. J. Leukoc. Biol. 63, 225–232 (1998).
Bednar, M. M., Jorgensen, I., Valdivia, R. H. & McCafferty, D. G. Chlamydia protease-like activity factor (CPAF): characterization of proteolysis activity in vitro and development of a nanomolar affinity CPAF zymogen-derived inhibitor. Biochemistry 50, 7441–7443 (2011).
Bae, Y. S. et al. Identification of peptides that antagonize formyl peptide receptor-like 1-mediated signaling. J. Immunol. 173, 607–614 (2004).
Jorgensen, I. et al. The Chlamydia protease CPAF regulates host and bacterial proteins to maintain pathogen vacuole integrity and promote virulence. Cell Host Microbe 10, 21–32 (2011).
Gray, R. D. et al. Activation of conventional protein kinase C (PKC) is critical in the generation of human neutrophil extracellular traps. J. Inflamm. 10, 12 (2013).
Hakkim, A. et al. Activation of the Raf–MEK–-ERK pathway is required for neutrophil extracellular trap formation. Nat. Chem. Biol. 7, 75–77 (2011).
von Kockritz-Blickwede, M. & Nizet, V. Innate immunity turned inside-out: antimicrobial defense by phagocyte extracellular traps. J. Mol. Med 87, 775–783 (2009).
Buchholz, K. R. & Stephens, R. S. The extracellular signal-regulated kinase/mitogen-activated protein kinase pathway induces the inflammatory factor interleukin-8 following Chlamydia trachomatis infection. Infect. Immun. 75, 5924–5929 (2007).
Darville, T. & Hiltke, T. J. Pathogenesis of genital tract disease due to Chlamydia trachomatis. J. Infect. Dis. 201, S114–S125 (2010).
Bai, H. et al. Intranasal inoculation of Chlamydia trachomatis mouse pneumonitis agent induces significant neutrophil infiltration which is not efficient in controlling the infection in mice. Immunology 114, 246–254 (2005).
Barteneva, N., Theodor, I., Peterson, E. M. & de la Maza, L. M. Role of neutrophils in controlling early stages of a Chlamydia trachomatis infection. Infect. Immun. 64, 4830–4833 (1996).
Tan, M. & Sutterlin, C. The Chlamydia protease CPAF: caution, precautions and function. Pathog. Dis. 72, 7–9 (2014).
Prince, L. R., Whyte, M. K., Sabroe, I., & Parker, L. C. The role of TLRs in neutrophil activation. Curr. Opin. Pharmacol. 11, 397–403 2011).
Al-Younes, H. M., Rudel, T., Brinkmann, V., Szczepek, A. J. & Meyer, T. F. Low iron availability modulates the course of Chlamydia pneumoniae infection. Cell. Microbiol. 3, 427–437 (2001).
Christophe, T. et al. The synthetic peptide Trp-Lys-Tyr-Met-Val-Met-NH2 specifically activates neutrophils through FPRL1/lipoxin A4 receptors and is an agonist for the orphan monocyte-expressed chemoattractant receptor FPRL2. J. Biol. Chem. 276, 21585–21593 (2001).
Dahlgren, C. et al. The synthetic chemoattractant Trp-Lys-Tyr-Met-Val-DMet activates neutrophils preferentially through the lipoxin A(4) receptor. Blood 95, 1810–1818 (2000).
Chen, K. et al. A critical role for the g protein-coupled receptor mFPR2 in airway inflammation and immune responses. J. Immunol. 184, 3331–3335 (2010).
Hattar, K. et al. Subthreshold concentrations of anti-proteinase 3 antibodies (c-ANCA) specifically prime human neutrophils for fMLP-induced leukotriene synthesis and chemotaxis. J. Leukoc. Biol. 69, 89–97 (2001).
Swamydas, M., Luo, Y., Dorf, M. E. & Lionakis, M. S. Isolation of mouse neutrophils. Curr. Protoc. Immunol. 110, 3.20.21–3.20.15 (2015).
Gonzalez, A. S., Bardoel, B. W., Harbort, C. J. & Zychlinsky, A. Induction and quantification of neutrophil extracellular traps. Methods Mol. Biol. 1124, 307–318 (2014).
Karunakaran, K., Mehlitz, A. & Rudel, T. Evolutionary conservation of infection-induced cell death inhibition among Chlamydiales. PLoS ONE 6, e22528 (2011).
de Haas, C. J. et al. Chemotaxis inhibitory protein of Staphylococcus aureus, a bacterial antiinflammatory agent. J. Exp. Med . 199, 687–695 (2004).
Yamazaki, T., Kawai, C., Yamauchi, A. & Kuribayashi, F. A highly sensitive chemiluminescence assay for superoxide detection and chronic granulomatous disease diagnosis. Trop. Med. Health 39, 41–45 (2011).
Fu, H. et al. Ligand recognition and activation of formyl peptide receptors in neutrophils. J. Leukoc. Biol. 79, 247–256 (2006).
Karlsson, J., Fu, H., Boulay, F., Bylund, J. & Dahlgren, C. The peptide Trp-Lys-Tyr-Met-Val-D-Met activates neutrophils through the formyl peptide receptor only when signaling through the formylpeptide receptor like 1 is blocked. A receptor switch with implications for signal transduction studies with inhibitors and receptor antagonists. Biochem. Pharmacol. 71, 1488–1496 (2006).
Onnheim, K., Bylund, J., Boulay, F., Dahlgren, C. & Forsman, H. Tumour necrosis factor (TNF)-α primes murine neutrophils when triggered via formyl peptide receptor-related sequence 2, the murine orthologue of human formyl peptide receptor-like 1, through a process involving the type I TNF receptor and subcellular granule mobilization. Immunology 125, 591–600 (2008).
Karunakaran, K., Subbarayal, P., Vollmuth, N. & Rudel, T. Chlamydia-infected cells shed Gp96 to prevent chlamydial re-infection. Mol. Microbiol 98, 694–711 (2015).
Durr, M. C. et al. Neutrophil chemotaxis by pathogen-associated molecular patterns - formylated peptides are crucial but not the sole neutrophil attractants produced by Staphylococcus aureus. Cell. Microbiol. 8, 207–217 (2006).
Acknowledgements
We thank D. Kretschmer and A. Peschel (Univeristy of Tübingen) for providing the HL60 cell lines and HL60 expressing FPR1 and FPR2. We thank R. Valdivia and E. Snavely (Duke University) for the CPAF-deficient and complemented strain of Chlamydia, G. Zhong (University of Texas) for the CPAF antibody and P. Lüningschrör (University of Würzburg) for the mouse synectin plasmid. We are grateful to O. Söhnlein (LMU Munich) for providing the FPR2-KO mice. C. Gehrig and D. Bunsen supported the scanning and transmission electron microscopy analyses. We acknowledge J. Sühlfleisch, N. Vollmuth and H. Czotscher for technical assistance. We thank S. Gorski, R. Sivadasan and A. Demuth for critically reading the manuscript. K.R. was supported by funds of the Frauenbüro, University of Würzburg. S.D. was funded by the Career Development Fellowship from the Graduate School of Life Sciences, University of Würzburg. This work was supported by Deutsche Forschungsgemeinschaft - GRK 2157 to T.R.
Author information
Authors and Affiliations
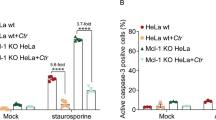
Contributions
K.R., S.D. and T.R. conceived and designed the study. K.R. performed all of the experiments, except for the experiments shown in Figs. 3a,b and 4f, which were carried out by S.D. Data analysis was performed by K.R and S.D. B.K.P. provided active and inactive recombinant CPAF. K.R. and T.R. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figures 1–8
Rights and permissions
About this article
Cite this article
Rajeeve, K., Das, S., Prusty, B.K. et al. Chlamydia trachomatis paralyses neutrophils to evade the host innate immune response. Nat Microbiol 3, 824–835 (2018). https://doi.org/10.1038/s41564-018-0182-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-018-0182-y
This article is cited by
-
Intracellular lifestyle of Chlamydia trachomatis and host–pathogen interactions
Nature Reviews Microbiology (2023)
-
Identification of differentially expressed genes and signaling pathways in human conjunctiva and reproductive tract infected with Chlamydia trachomatis
Human Genomics (2021)
-
Neutrophil chemoattractant receptors in health and disease: double-edged swords
Cellular & Molecular Immunology (2020)
-
Increase of leucocyte-derived extracellular traps (ETs) in semen samples from human acute epididymitis patients—a pilot study
Journal of Assisted Reproduction and Genetics (2020)
-
Pathogenic Interplay Between Chlamydia trachomatis and Neisseria gonorrhoeae that Influences Management and Control Efforts—More Questions than Answers?
Current Clinical Microbiology Reports (2019)