Abstract
Insulin resistance is a risk factor for obesity and diabetes and predisposes individuals to Staphylococcus aureus colonization; however, the contribution of S. aureus to insulin resistance remains unclear. Here, we show that S. aureus infection causes impaired glucose tolerance via secretion of an insulin-binding protein extracellular domain of LtaS, eLtaS, which blocks insulin-mediated glucose uptake. Notably, eLtaS transgenic mice (eLtaStrans) exhibited a metabolic syndrome similar to that observed in patients, including increased food and water consumption, impaired glucose tolerance and decreased hepatic glycogen synthesis. Furthermore, transgenic mice showed significant metabolic differences compared to their wild-type counterparts, particularly for the early insulin resistance marker α-hydroxybutyrate. We subsequently developed a full human monoclonal antibody against eLtaS that blocked the interaction between eLtaS and insulin, which effectively restored glucose tolerance in eLtaStrans and S. aureus-challenged mice. Thus, our results reveal a mechanism for S. aureus-induced insulin resistance.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Wilcox, G. Insulin and insulin resistance. Clin. Biochem. Rev. 26, 19–39 (2005).
Reaven, G. M. The metabolic syndrome: is this diagnosis necessary? Am. J. Clin. Nutr. 83, 1237–1247 (2006).
Saltiel, A. R. & Kahn, C. R. Insulin signalling and the regulation of glucose and lipid metabolism. Nature 414, 799–806 (2001).
Samuel, V. T. & Shulman, G. I. Mechanisms for insulin resistance: common threads and missing links. Cell 148, 852–871 (2012).
Cefalu, W. T. Insulin resistance: cellular and clinical concepts. Exp. Biol. Med. 226, 13–26 (2001).
Fabbrini, E. et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl Acad. Sci. USA 106, 15430–15435 (2009).
Ozcan, U. et al. Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science 313, 1137–1140 (2006).
Foster, T. J. Immune evasion by staphylococci. Nat. Rev. Microbiol. 3, 948–958 (2005).
Jenkins, A. et al. Differential expression and roles of Staphylococcus aureus virulence determinants during colonization and disease. mBio 6, e02272-14 (2015).
Wertheim, H. F. et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 5, 751–762 (2005).
Olsen, K. et al. Obesity and Staphylococcus aureus nasal colonization among women and men in a general population. PLoS ONE 8, e63716 (2013).
Smith, J. A. & O’Connor, J. J. Nasal carriage of Staphylococcus aureus in diabetes mellitus. Lancet 2, 776–777 (1966).
Tuazon, C. U., Perez, A., Kishaba, T. & Sheagren, J. N. Staphylococcus aureus among insulin-injecting diabetic patients. An increased carrier rate. JAMA 231, 1272 (1975).
van Belkum, A. et al. Co-evolutionary aspects of human colonisation and infection by Staphylococcus aureus. Infect. Genet. Evol. 9, 32–47 (2009).
Lipsky, B. A. et al. Diagnosis and treatment of diabetic foot infections. Clin. Infect. Dis. 39, 885–910 (2004).
Smit, J. et al. Diabetes and risk of community-acquired Staphylococcus aureus bacteremia: a population-based case–control study. Eur. J. Endocrinol. 174, 631–639 (2016).
Vu, B. G. et al. Chronic superantigen exposure induces systemic inflammation, elevated bloodstream endotoxin, and abnormal glucose tolerance in rabbits: possible role in diabetes. mBio 6, e02554 (2015).
Grundling, A. & Schneewind, O. Synthesis of glycerol phosphate lipoteichoic acid in Staphylococcus aureus. Proc. Natl Acad. Sci. USA 104, 8478–8483 (2007).
Wormann, M. E., Reichmann, N. T., Malone, C. L., Horswill, A. R. & Grundling, A. Proteolytic cleavage inactivates the Staphylococcus aureus lipoteichoic acid synthase. J. Bacteriol. 193, 5279–5291 (2011).
Lu, D. et al. Structure-based mechanism of lipoteichoic acid synthesis by Staphylococcus aureus LtaS. Proc. Natl Acad. Sci. USA 106, 1584–1589 (2009).
Taniguchi, C. M., Emanuelli, B. & Kahn, C. R. Critical nodes in signalling pathways: insights into insulin action. Nat. Rev. Mol. Cell Biol. 7, 85–96 (2006).
Liu, Y. et al. MAE4, an eLtaS monoclonal antibody, blocks Staphylococcus aureus virulence. Sci. Rep. 5, 17215 (2015).
Chang, L., Chiang, S. H. & Saltiel, A. R. Insulin signaling and the regulation of glucose transport. Mol. Med. 10, 65–71 (2004).
Intasai, N., Arooncharus, P., Kasinrerk, W. & Tayapiwatana, C. Construction of high-density display of CD147 ectodomain on VCSM13 phage via gpVIII: effects of temperature, IPTG, and helper phage infection-period. Protein Expr. Purif. 32, 323–331 (2003).
Bryant, N. J., Govers, R. & James, D. E. Regulated transport of the glucose transporter GLUT4. Nat. Rev. Mol. Cell Biol. 3, 267–277 (2002).
Govers, R., Coster, A. C. & James, D. E. Insulin increases cell surface GLUT4 levels by dose dependently discharging GLUT4 into a cell surface recycling pathway. Mol. Cell. Biol. 24, 6456–6466 (2004).
Fleig, W. E., Enderle, D., Steudter, S., Nother-Fleig, G. & Ditschuneit, H. Regulation of basal and insulin-stimulated glycogen synthesis in cultured hepatocytes. Inverse relationship to glycogen content. J. Biol. Chem. 262, 1155–1160 (1987).
Miller, T. B. Jr, Garnache, A. K., Cruz, J., McPherson, R. K. & Wolleben, C. Regulation of glycogen metabolism in primary cultures of rat hepatocytes. Restoration of acute effects of insulin and glucose in cells from diabetic rats. J. Biol. Chem. 261, 785–790 (1986).
Dimitriadis, G. et al. Evaluation of glucose transport and its regulation by insulin in human monocytes using flow cytometry. Cytometry A 64, 27–33 (2005).
Gall, W. E. et al. α-Hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS ONE 5, e10883 (2010).
Felig, P., Marliss, E. & Cahill, G. F. Jr. Plasma amino acid levels and insulin secretion in obesity. N. Engl. J. Med. 281, 811–816 (1969).
Felig, P., Wahren, J., Hendler, R. & Brundin, T. Splanchnic glucose and amino acid metabolism in obesity. J. Clin. Invest. 53, 582–590 (1974).
Prada, P. O. et al. l-Glutamine supplementation induces insulin resistance in adipose tissue and improves insulin signalling in liver and muscle of rats with diet-induced obesity. Diabetologia 50, 1949–1959 (2007).
Lynch, C. J. & Adams, S. H. Branched-chain amino acids in metabolic signalling and insulin resistance. Nat. Rev. Endocrinol. 10, 723–736 (2014).
Liang, R. et al. Acylation of exenatide by glycolic acid and its anti-diabetic activities in db/db mice. Pharm. Res. 31, 1958–1966 (2014).
Liu, Z., Jeppesen, P. B., Gregersen, S., Bach Larsen, L. & Hermansen, K. Chronic exposure to proline causes aminoacidotoxicity and impaired beta-cell function: studies in vitro. Rev. Diabet. Stud. 13, 66–78 (2016).
den Ouden, H. et al. Metabolomic biomarkers for personalised glucose lowering drugs treatment in type 2 diabetes. Metabolomics 12, 27 (2016).
Chen, H. H. et al. The metabolome profiling and pathway analysis in metabolic healthy and abnormal obesity. Int. J. Obes. 39, 1241–1248 (2015).
Kwon, H. & Pessin, J. E. Adipokines mediate inflammation and insulin resistance. Front. Endocrinol. 4, 71 (2013).
Weiss, R. et al. Prediabetes in obese youth: a syndrome of impaired glucose tolerance, severe insulin resistance, and altered myocellular and abdominal fat partitioning. Lancet 362, 951–957 (2003).
Nathan, D. M. et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30, 753–759 (2007).
Tuomilehto, J. et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 344, 1343–1350 (2001).
Gerstein, H. C. et al. Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: a systematic overview and meta-analysis of prospective studies. Diabetes Res. Clin. Pract. 78, 305–312 (2007).
Lipsky, B. A., Pecoraro, R. E., Chen, M. S. & Koepsell, T. D. Factors affecting staphylococcal colonization among NIDDM outpatients. Diabetes Care 10, 483–486 (1987).
Ran, F. A. et al. Genome engineering using the CRISPR–Cas9 system. Nat. Protoc. 8, 2281–2308 (2013).
Fehniger, T. A. et al. Fatal leukemia in interleukin 15 transgenic mice follows early expansions in natural killer and memory phenotype CD8+ T cells. J. Exp. Med. 193, 219–231 (2001).
Feng, B. et al. Metabolic profiling analysis of a d-galactosamine/lipopolysaccharide-induced mouse model of fulminant hepatic failure. J. Proteome Res. 6, 2161–2167 (2007).
Acknowledgements
We thank H. Wu, Q. Wu and Y. Wu (Beijing Institute of Basic Medical Sciences) for technical support on preparation of the frozen tissue sections. This work was supported by grants from the National Natural Science Foundation of China (http://www.nsfc.gov.cn) (31370170) and the Natural Science Foundation of Beijing (http://bjnsf.bjkw.gov.cn/) (7142119). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.L., F.-J.L. and Z.-C.G. acquired, analysed and interpreted the data. F.-T.D., J.-H.C., Y.-P.G., D.L. and D.-P.H. provided administrative, technical and material support. J.Y. and C.-H.L. analysed the data. C.-M.M. provided material support. J.-N.F. and B.-F.S. supervised the study. G.Y. conceived and designed the study, obtained funding and prepared the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
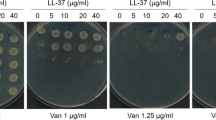
Supplementary Figures 1–17, Supplementary Table 1
Rights and permissions
About this article
Cite this article
Liu, Y., Liu, FJ., Guan, ZC. et al. The extracellular domain of Staphylococcus aureus LtaS binds insulin and induces insulin resistance during infection. Nat Microbiol 3, 622–631 (2018). https://doi.org/10.1038/s41564-018-0146-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-018-0146-2
This article is cited by
-
Staphylococcus aureus blocks insulin function
Nature Microbiology (2018)
-
Role for S. aureus in insulin resistance
Nature Reviews Endocrinology (2018)