Abstract
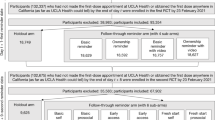
The influenza (‘flu’) vaccination is low cost1 and effective, typically reducing the likelihood of infection by 50–60%2. It is recommended for nearly everyone older than 6 months of age3; yet, only 40% of Americans are immunized each year. Vaccination rates are higher among at-risk groups, such as those ≥65 years of age, but still only 6 in 10 receive it4. There have been numerous attempts to improve vaccination rates using strategies such as school-based programmes, financial incentives and reminders, but these have generally had limited success5,6,7. Of the attempts that are successful, most are expensive—limiting scalability—and have not been evaluated in the elderly8. Conversely, lower-cost interventions, such as mailed information, hold promise for a scalable solution, but their limited effectiveness may result from how they have been designed. We randomly assigned 228,000 individuals ≥66 years of age to one of five versions of letters intended to motivate vaccination, including versions with an implementation intention prompt and an enhanced active choice implementation prompt. We found that a single mailed letter significantly increased influenza vaccination rates compared with no letter. However, there was no difference in vaccination rates across the four different letters tailored with behavioural science techniques.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Restrictions apply to the availability of the raw data, which were used under data use agreements for the current study and therefore cannot be shared publicly. However, data may be available upon reasonable request and permission of the vendor.
References
CDC Vaccine Price List (CDC, 2018); https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html
Vaccine Effectiveness—How Well Does the Flu Vaccine Work? (CDC, 2017); https://www.cdc.gov/flu/about/qa/vaccineeffect.html
Advisory Committee on Immunization Practices (ACIP) Recommendations and Immunization Schedules (CDC, 2012); http://www.cdc.gov/vaccines/acip/recs/index.html
Flu Vaccination Coverage, United States, 2015–16 Influenza Season (CDC, 2016); https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.html
Briss, P. A. et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The task force on community preventive services. Am. J. Prev. Med. 18, 97–140 (2000).
Jacob, V. et al. Increasing coverage of appropriate vaccinations: a community guide systematic economic review. Am. J. Prev. Med. 50, 797–808 (2016).
Stinchfield, P. K. Practice-proven interventions to increase vaccination rates and broaden the immunization season. Am. J. Med. 121, S11–S21 (2008).
Arthur, A. J. et al. Improving uptake of influenza vaccination among older people: a randomised controlled trial. Br. J. Gen. Pract. 52, 717–722 (2002).
Social and Behavioral Sciences Team Social and Behavioral Sciences Team Annual Report (Office of Science and Technology Policy, 2015); https://sbst.gov/download/2015%20SBST%20Annual%20Report.pdf
Milkman, K. L., Beshears, J., Choi, J. J., Laibson, D. & Madrian, B. C. Using implementation intentions prompts to enhance influenza vaccination rates. Proc. Natl Acad. Sci. USA 108, 10415–10420 (2011).
Gollwitzer, P. Implementation intentions: strong effects of simple plans. Am. Psychol. 54, 493–503 (1999).
Keller, P., Harlam, B., Loewenstein, G. & Volpp, K. Enhanced active choice: a new method to motivate behavior change. J. Consum. Psychol. 21, 376–383 (2011).
O’Keefe, D. J. in The International Encyclopedia of Communication (ed. Donsbach, W.) https://doi.org/10.1002/9781405186407.wbiece011.pub2 (John Wiley and Sons, 2013).
Bleich, S. N., Gudzune, K. A., Bennett, W. L., Jarlenski, M. P. & Cooper, L. A. How does physician BMI impact patient trust and perceived stigma? Prev. Med. 57, 120–124 (2013).
Herrett, E. et al. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open 6, e010069 (2016).
Regan, A. K., Bloomfield, L., Peters, I. & Effler, P. V. Randomized controlled trial of text message reminders for increasing influenza vaccination. Ann. Fam. Med. 15, 507–514 (2017).
Cutrona, S. L. et al. Improving rates of outpatient influenza vaccination through ehr portal messages and interactive automated calls: a randomized controlled trial. J. Gen. Intern. Med. 33, 659–667 (2018).
Jacobson Vann, J. C., Jacobson, R. M., Coyne-Beasley, T., Asafu-Adjei, J. K. & Szilagyi, P. G. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst. Rev. 1, CD003941 (2018).
Michaelidis, C. I., Zimmerman, R. K., Nowalk, M. P. & Smith, K. J. Cost-effectiveness of programs to eliminate disparities in elderly vaccination rates in the United States. BMC Public Health 14, 718 (2014).
Reminder Systems and Strategies for Increasing Childhood Vaccination Rates (CDC, 2017); https://www.cdc.gov/vaccines/hcp/admin/reminder-sys.html
Kim, M. & Yoo, B. K. Cost-effectiveness analysis of a television campaign to promote seasonal influenza vaccination among the elderly. Value Health 18, 622–630 (2015).
Shoup, J. A. et al. Effectiveness and cost of influenza vaccine reminders for adults with asthma or chronic obstructive pulmonary disease. Am. J. Manag. Care 21, e405–e413 (2015).
Anderson, L. J. et al. The cost of interventions to increase influenza vaccination: a systematic review. Am. J. Prev. Med. 54, 299–315 (2018).
VIII. Privacy—Telephone Consumer Protection Act. FDIC Compliance Examination Manual (Federal Deposit Insurance Corporation, 2016); https://www.fdic.gov/regulations/compliance/manual/index.html
Kuerbis, A., van Stolk-Cooke, K. & Muench, F. An exploratory study of mobile messaging preferences by age: middle-aged and older adults compared to younger adults. J. Rehabil. Assist. Technol. Eng. 4, 1–10 (2017).
Mobile Fact Sheet (Pew Research Center, 2018); http://www.pewinternet.org/fact-sheet/mobile/
Lochner, K. A., Wynne, M. A., Wheatcroft, G. H., Worrall, C. M. & Kelman, J. A. Medicare claims versus beneficiary self-report for influenza vaccination surveillance. Am. J. Prev. Med. 48, 384–391 (2015).
Alemayehu, B. & Warner, K. E. The lifetime distribution of health care costs. Health Serv. Res. 39, 627–642 (2004).
Kahan, B. C., Jairath, V., Doré, C. J. & Morris, T. P. The risks and rewards of covariate adjustment in randomized trials: an assessment of 12 outcomes from 8 studies. Trials 15, 139 (2014).
Lee, P. H. Covariate adjustments in randomized controlled trials increased study power and reduced biasedness of effect size estimation. J. Clin. Epidemiol. 76, 137–146 (2016).
Rothman, K. J. No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46 (1990).
Wason, J. M. S., Stecher, L. & Mander, A. P. Correcting for multiple-testing in multi-arm trials: is it necessary and is it done? Trials 15, 364 (2014).
McAlister, F. A. The “number needed to treat” turns 20—and continues to be used and misused. CMAJ 179, 549–553 (2008).
Acknowledgements
This project would not have been possible without the collaboration of the White House’s Social and Behavioral Sciences Team (SBST), the General Service Administration’s Office of Evaluation Sciences, the National Vaccine Program Office and the Centers for Medicare and Medicaid Services (CMS) at the US Department of Health and Human Services. We especially thank G. Brill, M. Donneyong, B. Gellin, T. A. Johnson, B. Luca and B. Sivak. We also thank The Laura and John Arnold Foundation for generous financial support. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. This work was supported by an unrestricted grant from the Laura and John Arnold Foundation.
Author information
Authors and Affiliations
Contributions
D.Y. and N.K.C. contributed to the study conception and design and interpretation of the results. J.C.L. prepared and analysed the data. D.Y. and J.C.L. contributed to manuscript drafting. N.K.C. and R.G. provided interpretation of the results and critical manuscript revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Information
Supplementary Figure 1, Supplementary Tables 1–5
Rights and permissions
About this article
Cite this article
Yokum, D., Lauffenburger, J.C., Ghazinouri, R. et al. Letters designed with behavioural science increase influenza vaccination in Medicare beneficiaries. Nat Hum Behav 2, 743–749 (2018). https://doi.org/10.1038/s41562-018-0432-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-018-0432-2
This article is cited by
-
The impact of using reinforcement learning to personalize communication on medication adherence: findings from the REINFORCE trial
npj Digital Medicine (2024)
-
Last-mile delivery increases vaccine uptake in Sierra Leone
Nature (2024)
-
Evidence from a statewide vaccination RCT shows the limits of nudges
Nature (2022)
-
Improving postal survey response using behavioural science: a nested randomised control trial
BMC Medical Research Methodology (2021)
-
A message of the majority with scientific evidence encourages young people to show their prosocial nature in COVID-19 vaccination
Scientific Reports (2021)