Abstract
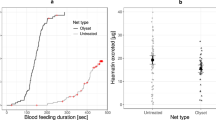
Insecticide-treated bed nets reduce malaria transmission by limiting contact between mosquito vectors and human hosts when mosquitoes feed during the night. However, malaria vectors can also feed in the early evening and in the morning when people are not protected. Here, we explored how the timing of blood feeding interacts with environmental temperature to influence the capacity of Anopheles mosquitoes to transmit the human malaria parasite Plasmodium falciparum. In laboratory experiments, we found no effect of biting time itself on the proportion of mosquitoes that became infectious (vector competence) at constant temperature. However, when mosquitoes were maintained under more realistic fluctuating temperatures, there was a significant increase in competence for mosquitoes feeding in the evening (18:00), and a significant reduction in competence for those feeding in the morning (06:00), relative to those feeding at midnight (00:00). These effects appear to be due to thermal sensitivity of malaria parasites during the initial stages of parasite development within the mosquito, and the fact that mosquitoes feeding in the evening experience cooling temperatures during the night, whereas mosquitoes feeding in the morning quickly experience warming temperatures that are inhibitory to parasite establishment. A transmission dynamics model illustrates that such differences in competence could have important implications for malaria prevalence, the extent of transmission that persists in the presence of bed nets, and the epidemiological impact of behavioural resistance. These results indicate that the interaction of temperature and feeding behaviour could be a major ecological determinant of the vectorial capacity of malaria mosquitoes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Code availability
The code used for modelling in this study is available at https://github.com/jamiegriffin/Malaria_simulation. Any changes to this code are described within this paper.
References
Bhatt, S. et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526, 207–211 (2015).
Churcher, T. S., Lissenden, N., Griffin, J. T., Worrall, E. & Ranson, H. The impact of pyrethroid resistance of the efficacy and effectiveness of bednets for malaria control in Africa. eLife 5, e16090 (2016).
Ranson, H. & Lissenden, N. Insecticide resistance in African Anopheles mosquitoes: a worsening situation that needs urgent action to maintain malaria control. Trends Parasitol. 32, 187–196 (2016).
Hemingway, J. et al. Averting a malaria disaster: will insecticide resistance derail malaria control? Lancet 387, 1785–1788 (2016).
Moiroux, N. et al. Changes in Anopheles funestus biting behavior following universal coverage of long-lasting insecticidal nets in Benin. J. Infect. Dis. 206, 1622–1629 (2012).
Russell, T. et al. Increased proportions of outdoor feeding among residual malaria vector populations following increased use of insecticide-treated nets in rural Tanzania. Malar. J. 10, 80 (2011).
Thomsen, E. K. et al. Mosquito behavior change after distribution of bednets results in decreased protection against malaria exposure. J. Infect. Dis. 215, 790–797 (2017).
Carrasco, D. et al. Behavioural adaptations of mosquito vectors to insecticide control. Curr. Opin. Insect Sci. 34, 48–54 (2019).
Protopopoff, N. et al. Effectiveness of a long-lasting piperonyl butoxide-treated insecticidal net and indoor residual spray interventions, separately and together, against malaria transmitted by pyrethroid-resistant mosquitoes: a cluster, randomised controlled, two-by-two factorial design trial. Lancet 391, 1577–1588 (2018).
Uragayala, S. et al. Village-scale (phase III) evaluation of the efficacy and residual activity of SumiShield® 50 WG (Clothianidin 50%, w/w) for indoor spraying for the control of pyrethroid-resistant Anopheles culicifacies Giles in Karnataka State, India. Trop. Med. Int. Health 23, 605–615 (2018).
Mashauri, F. M. et al. Indoor residual spraying with micro-encapsulated pirimiphos-methyl (Actellic® 300CS) against malaria vectors in the Lake Victoria basin, Tanzania. PLoS ONE 12, e0176982 (2017).
Bayili, K. et al. Evaluation of efficacy of Interceptor® G2, a long-lasting insecticide net coated with a mixture of chlorfenapyr and alpha-cypermethrin, against pyrethroid resistant Anopheles gambiae s.l. in Burkina Faso. Malar. J. 16, 190 (2017).
Tiono, A. B. et al. Efficacy of Olyset Duo, a bednet containing pyriproxyfen and permethrin, versus a permethrin-only net against clinical malaria in an area with highly pyrethroid-resistant vectors in rural Burkina Faso: a cluster-randomised controlled trial. Lancet 392, 569–580 (2018).
Gatton, M. L. et al. The importance of mosquito behavioural adaptations to malaria control in Africa. Evolution 67, 1218–1230 (2013).
Killeen, G. F. Characterizing, controlling and eliminating residual malaria transmission. Malar. J. 13, 330 (2014).
Sherrard-Smith, E. et al. Mosquito feeding behavior and how it influences residual malaria transmission across Africa. Proc. Natl Acad. Sci. USA 116, 15086–15095 (2019).
Durnez, L. & Coosemans, M. Residual Transmission of Malaria: an Old Issue for New Approaches (Intech, 2013).
Lambrechts, L. Quantitative genetics of Aedes aegypti vector competence for Dengue viruses: towards a new paradigm? Trends Parasitol. 27, 111–114 (2011).
Baton, L. A. & Ranford-Cartwright, L. C. Spreading the seeds of million-murdering death: metamorphoses of malaria in the mosquito. Trends Parasitol. 21, 573–580 (2005).
Beier, J. C. Malaria parasite development in mosquitoes. Annu. Rev. Entomol. 43, 519–543 (1998).
Lefevre, T., Vantaux, A., Dabire, K. R., Mouline, K. & Cohuet, A. Non-genetic determinants of mosquito competence for malaria parasites. PLoS Pathog. 9, e1003365 (2013).
Westwood, M. L. et al. The evolutionary ecology of circadian rhythms in infection. Nat. Ecol. Evol. 3, 552–560 (2019).
Rund, S. S. C., O’Donnell, A. J., Gentile, J. E. & Reece, S. E. Daily rhythms in mosquitoes and their consequences for malaria transmission. Insects 7, E14 (2016).
Rund, S. S. C., Hou, T. Y., Ward, S. M., Collins, F. H. & Duffield, G. E. Genome-wide profiling of diel and circadian gene expression in the malaria vector Anopheles gambiae. Proc. Natl Acad. Sci. USA 108, E421–E430 (2011).
Blanford, J. I. et al. Implications of temperature variation for malaria parasite development across Africa. Sci. Rep. 3, 1300 (2013).
Glunt, K. D., Blanford, J. I. & Paaijmans, K. P. Chemicals, climate, and control: increasing the effectiveness of malaria vector control tools by considering relevant temperatures. PLoS Pathog. 9, e1003602 (2013).
Paaijmans, K. P. et al. Downscaling reveals diverse effects of anthropogenic climate warming on the potential for local environments to support malaria transmission. Clim. Change 125, 479–488 (2014).
Thomas, S. et al. Microclimate variables of the ambient environment deliver the actual estimates of the extrinsic incubation period of Plasmodium vivax and Plasmodium falciparum: a study from a malaria-endemic urban setting, Chennai in India. Malar. J. 17, 201 (2018).
Eling, W., Hooghof, J., van de Vegte-Bolmer, M., Sauerwein, R. & van Gemert, G.-J. Tropical temperatures can inhibit development of the human malaria parasite Plasmodium falciparum in the mosquito. Proc. Exp. Appl. Entomol. 12, 151–156 (2001).
Noden, B. H., Kent, M. D. & Beier, J. C. The impact of variations in temperature on early Plasmodium falciparum development in Anopheles stephensi. Parasitology 111, 539–545 (1995).
Murdock, C. C., Moller-Jacobs, L. L. & Thomas, M. B. Complex environmental drivers of immunity and resistance in malaria mosquitoes. Proc. R. Soc. B Biol. Sci. 280, 20132030 (2013).
Gillies, M. T. & De Meillon, B. The Anophelinae of Africa South of the Sahara (Ethiopian Zoogeographical Region) 2nd edn (South African Institute for Medical Research, 1968).
Paaijmans, K. P. et al. Influence of climate on malaria transmission depends on daily temperature variation. Proc. Natl Acad. Sci. USA 107, 15135–15139 (2010).
Paaijmans, K. P., Read, A. F. & Thomas, M. B. Understanding the link between malaria risk and climate. Proc. Natl Acad. Sci. USA 106, 13844–13849 (2009).
Ohm, J. R. et al. Rethinking the extrinsic incubation period of malaria parasites. Parasites Vectors 11, 178 (2018).
Waite, J. L., Suh, E., Lynch, P. A. & Thomas, M. B. Exploring the lower thermal limits for development of the human malaria parasite, Plasmodium falciparum. Biol. Lett. 15, 20190275 (2019).
Griffin, J. T. et al. Reducing Plasmodium falciparum malaria transmission in Africa: a model-based evaluation of intervention strategies. PLoS Med. 7, e1000324 (2010).
White, M. T. et al. Modelling the impact of vector control interventions on Anopheles gambiae population dynamics. Parasites Vectors 4, 153 (2011).
Griffin, J. T., Ferguson, N. M. & Ghani, A. C. Estimates of the changing age-burden of Plasmodium falciparum malaria disease in sub-Saharan Africa. Nat. Commun. 5, 3136 (2014).
Griffin, J. T. et al. Gradual acquisition of immunity to severe malaria with increasing exposure. Proc. R. Soc. B Biol. Sci. 282, 20142657 (2015).
Killeen, G. F. et al. Made-to-measure malaria vector control strategies: rational design based on insecticide properties and coverage of blood resources for mosquitoes. Malar. J. 13, 146 (2014).
Janko, M. M., Churcher, T. S., Emch, M. E. & Meshnick, S. R. Strengthening long-lasting insecticidal nets effectiveness monitoring using retrospective analysis of cross-sectional, population-based surveys across sub-Saharan Africa. Sci. Rep. 8, 17110 (2018).
Kirby, M. J. & Lindsay, S. W. Responses of adult mosquitoes of two sibling species, Anopheles arabiensis and A. gambiae s.s. (Diptera: Culicidae), to high temperatures. Bull. Entomol. Res. 94, 441–448 (2004).
Benoit, J. B. et al. Drinking a hot blood meal elicits a protective heat shock response in mosquitoes. Proc. Natl Acad. Sci. USA 108, 8026–8029 (2011).
Lahondere, C. & Lazzari, C. R. Mosquitoes cool down during blood feeding to avoid overheating. Curr. Biol. 22, 40–45 (2012).
Ferguson, H. M. et al. Selection of mosquito life-histories: a hidden weapon against malaria? Malar. J. 11, 106 (2012).
Murdock, C. C., Paaijmans, K. P., Cox-Foster, D., Read, A. F. & Thomas, M. B. Rethinking vector immunology: the role of environmental temperature in shaping resistance. Nat. Rev. Microbiol. 10, 869–876 (2012).
Murdock, C. C., Blanford, S., Hughes, G. L., Rasgon, J. L. & Thomas, M. B. Temperature alters Plasmodium blocking by Wolbachia. Sci. Rep. 4, 3932 (2014).
Lyons, C. L., Coetzee, M., Terblanche, J. S. & Chown, S. L. Thermal limits of wild and laboratory strains of two African malaria vector species, Anopheles arabiensis and Anopheles funestus. Malar. J. 11, 226 (2012).
Sternberg, E. D. & Thomas, M. B. Local adaptation to temperature and the implications for vector-borne diseases. Trends Parasitol. 30, 115–122 (2014).
Siddons, L. B. Observations on the influence of atmospheric temperature and humidity on the infectivity of Anopheles culicifacies Giles. J. Malar. Inst. India 5, 375–388 (1944).
Knowles, R. & Basu, B. C. Laboratory studies on the infectivity of Anopheles stephensi. J. Malar. Inst. India 5, 1–29 (1943).
Okech, B. A. et al. Resistance of early midgut stages of natural Plasmodium falciparum parasites to high temperatures in experimentally infected Anopheles gambiae (Diptera: Culicidae). J. Parasitol. 90, 764–768 (2004).
Bradley, J. et al. Predicting the likelihood and intensity of mosquito infection from sex specific Plasmodium falciparum gametocyte density. eLife 7, e34463 (2018).
Pathak, A. K., Shiau, J. C., Thomas, M. B. & Murdock, C. Field relevant variation in ambient temperature modifies density-dependent establishment of Plasmodium falciparum gametocytes in mosquitoes. Front. Microbiol. 10, 2651 (2019).
Schneider, P. et al. Adaptive plasticity in the gametocyte conversion rate of malaria parasites. PLoS Pathog. 14, e1007371 (2018).
Schneider, P. et al. Adaptive periodicity in the infectivity of malaria gametocytes to mosquitoes. Proc. R. Soc. B Biol. Sci. 285, 20181876 (2018).
Githeko, A. K. et al. Confirmation that Plasmodium falciparum has asperiodic infectivity to Anopheles gambiae. Med. Vet. Entomol. 7, 373–376 (1993).
Magesa, S. M., Mdira, Y. K., Akida, J. A., Bygbjerg, I. C. & Jakobsen, P. H. Observations on the periodicity of Plasmodium falciparum gametocytes in natural human infections. Acta Trop. 76, 239–246 (2000).
Ferguson, H. M. et al. Ecology: a prerequisite for malaria elimination and eradication. PLoS Med. 7, e1000303 (2010).
Thomas, M. B. et al. Lessons from agriculture for the sustainable management of malaria vectors. PLoS Med. 9, e1001262 (2012).
Lefevre, T. et al. Transmission traits of malaria parasites within the mosquito: genetic variation, phenotypic plasticity, and consequences for control. Evol. Appl. 11, 456–469 (2018).
Stratman-Thomas, W. K. The influence of temperature on Plasmodium vivax. Am. J. Trop. Med. Hyg. S1–S20, 703–715 (1940).
Ball, G. H. & Chao, J. Temperature stresses on the mosquito phase of Plasmodium relictum. J. Parasitol. 50, 748–752 (1964).
Vanderberg, J. P. & Yoeli, M. Effects of temperature on sporogonic development of Plasmodium berghei. J. Parasitol. 52, 559–564 (1966).
Simoes, M. L., Caragata, E. P. & Dimopoulos, G. Diverse host and restriction factors regulate mosquito–pathogen interactions. Trends Parasitol. 34, 603–616 (2018).
Riehle, M. M. et al. Natural malaria infection in Anopheles gambiae is regulated by a single genomic control region. Science 312, 577–579 (2006).
Molina-Cruz, A. et al. Plasmodium evasion of mosquito immunity and global malaria transmission: the lock-and-key theory. Proc. Natl Acad. Sci. USA 112, 15178–15183 (2015).
Van Tol, S. & Dimopoulos, G. in Progress in Mosquito Research Vol. 51 (ed. Raikhel, A. S.) 243–291 (Academic Press and Elsevier Science, 2016).
Wang, S. B. et al. Driving mosquito refractoriness to Plasmodium falciparum with engineered symbiotic bacteria. Science 357, 1399–1402 (2017).
Cirimotich, C. M. et al. Natural microbe-mediated refractoriness to Plasmodium infection in Anopheles gambiae. Science 332, 855–858 (2011).
Bugoro, H. et al. Bionomics of the malaria vector Anopheles farauti in Temotu Province, Solomon Islands: issues for malaria elimination. Malar. J. 10, 133 (2011).
Geissbuhler, Y. et al. Interdependence of domestic malaria prevention measures and mosquito–human interactions in urban Dar es Salaam, Tanzania. Malar. J. 6, 126 (2007).
Russell, T. L. et al. Frequent blood feeding enables insecticide-treated nets to reduce transmission by mosquitoes that bite predominately outdoors. Malar. J. 15, 156 (2016).
Seyoum, A. et al. Human exposure to anopheline mosquitoes occurs primarily indoors, even for users of insecticide-treated nets in Luangwa Valley, South-East Zambia. Parasites Vectors 5, 101 (2012).
Bayoh, M. N. et al. Persistently high estimates of late night, indoor exposure to malaria vectors despite high coverage of insecticide treated nets. Parasites Vectors 7, 380 (2014).
Killeen, G. F. et al. Quantifying behavioural interactions between humans and mosquitoes: evaluating the protective efficacy of insecticidal nets against malaria transmission in rural Tanzania. BMC Infect. Dis. 6, 161 (2006).
Mordecai, E. A. et al. Optimal temperature for malaria transmission is dramatically lower than previously predicted. Ecol. Lett. 16, 22–30 (2013).
Shapiro, L. L. M., Murdock, C. C., Jacobs, G. R., Thomas, R. J. & Thomas, M. B. Larval food quantity affects the capacity of adult mosquitoes to transmit human malaria. Proc. R. Soc. B Biol. Sci. 283, 20160298 (2016).
Parton, W. J. & Logan, J. A. A model for diurnal variation in soil and air temperature. Agric. Meteorol. 23, 205–216 (1981).
Detinova, T. Age-grouping methods in Diptera of medical importance with special reference to some vectors of malaria. Monogr. Ser. World Health Organ. 47, 13–91 (1962).
Shapiro, L. L. M., Whitehead, S. A. & Thomas, M. B. Quantifying the effects of temperature on mosquito and parasite traits that determine the transmission potential of human malaria. PLoS. Biol. 15, e2003489 (2017).
Walker, P. G. T., Griffin, J. T., Ferguson, N. M. & Ghani, A. C. Estimating the most efficient allocation of interventions to achieve reductions in Plasmodium falciparum malaria burden and transmission in Africa: a modelling study. Lancet Glob. Health 4, E474–E484 (2016).
Winskill, P., Slater, H. C., Griffin, J. T., Ghani, A. C. & Walker, P. G. T. The US President’s Malaria Initiative, Plasmodium falciparum transmission and mortality: a modelling study. PLoS Med. 14, e1002448 (2017).
Slater, H. C., Walker, P. G. T., Bousema, T., Okell, L. C. & Ghani, A. C. The potential impact of adding ivermectin to a mass treatment intervention to reduce malaria transmission: a modelling study. J. Infect. Dis. 210, 1972–1980 (2014).
Huho, B. et al. Consistently high estimates for the proportion of human exposure to malaria vector populations occurring indoors in rural Africa. Int. J. Epidemiol. 42, 235–247 (2013).
Wat’senga, F. et al. Nationwide insecticide resistance status and biting behaviour of malaria vector species in the Democratic Republic of Congo. Malar. J. 17, 129 (2018).
Reddy, M. R. et al. Outdoor host seeking behaviour of Anopheles gambiae mosquitoes following initiation of malaria vector control on Bioko Island, Equatorial Guinea. Malar. J. 10, 184 (2011).
Cooke, M. K. et al. ‘A bite before bed’: exposure to malaria vectors outside the times of net use in the highlands of western Kenya. Malar. J. 14, 259 (2015).
Garske, T., Ferguson, N. M. & Ghani, A. C. Estimating air temperature and its influence on malaria transmission across Africa. PLoS ONE 8, e56487 (2013).
West, B., Welch, K. & Galecki, A. Linear Mixed Models: a Practical Guide Using Statistical Software 2nd edn (Chapman & Hall, 2007).
Gill, J. & King, G. What to do when your hessian is not invertible: alternatives to model respecification in nonlinear estimation. Sociol. Methods Res. 33, 54–87 (2004).
Suh, E. et al. Dryad Data from: The influence of feeding behaviour and temperature on the capacity of mosquitoes to transmit malaria. (Dryad Digital Repository, 2020); https://doi.org/10.5061/dryad.b2rbnzsb5
Acknowledgements
We thank D. C. Soergel, J. L. Teeple and F. Ware-Gilmore for technical assistance, and D. A. Kennedy, E. D. Sternberg and L. Ge for advice on statistical analyses. This study was supported by NIH NIAID grant R01AI110793 and National Science Foundation Ecology and Evolution of Infectious Diseases grant DEB-1518681. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
E.S., J.L.W., E.S.-S., T.S.C. and M.B.T. designed the research. E.S., J.L.W., N.L.D. and E.S.-S. performed the research. E.S., M.K.G., E.S.-S. and T.S.C. analysed the data. E.S., E.S.-S., T.S.C. and M.B.T. wrote the manuscript with input from M.K.G., J.L.W. and N.L.D.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–7 and Tables 1–13.
Rights and permissions
About this article
Cite this article
Suh, E., Grossman, M.K., Waite, J.L. et al. The influence of feeding behaviour and temperature on the capacity of mosquitoes to transmit malaria. Nat Ecol Evol 4, 940–951 (2020). https://doi.org/10.1038/s41559-020-1182-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41559-020-1182-x
This article is cited by
-
Seasonal assessment on the effects of time of night, temperature and humidity on the biting profile of Anopheles farauti in north Queensland, Australia using a population naive to malaria vector control pressures
Malaria Journal (2023)
-
Effects of different feeding methods and hosts on the fecundity and blood-feeding behavior of Aedes aegypti and Aedes albopictus (Diptera: Culicidae)
Biologia (2023)
-
The effect of climate change on malaria transmission in the southeast of Iran
International Journal of Biometeorology (2022)