Abstract
Reactive oxygen species (ROS) contribute to tissue damage and remodelling mediated by the inflammatory response after injury. Here we show that ROS, which promote axonal dieback and degeneration after injury, are also required for axonal regeneration and functional recovery after spinal injury. We find that ROS production in the injured sciatic nerve and dorsal root ganglia requires CX3CR1-dependent recruitment of inflammatory cells. Next, exosomes containing functional NADPH oxidase 2 complexes are released from macrophages and incorporated into injured axons via endocytosis. Once in axonal endosomes, active NOX2 is retrogradely transported to the cell body through an importin-β1–dynein-dependent mechanism. Endosomal NOX2 oxidizes PTEN, which leads to its inactivation, thus stimulating PI3K–phosporylated (p-)Akt signalling and regenerative outgrowth. Challenging the view that ROS are exclusively involved in nerve degeneration, we propose a previously unrecognized role of ROS in mammalian axonal regeneration through a NOX2–PI3K–p-Akt signalling pathway.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Change history
08 March 2018
In the version of this Article originally published, the affiliations for Roland A. Fleck and José Antonio Del Río were incorrect due to a technical error that resulted in affiliations 8 and 9 being switched. The correct affiliations are: Roland A. Fleck: 8Centre for Ultrastructural Imaging, Kings College London, London, UK. José Antonio Del Río: 2Cellular and Molecular Neurobiotechnology, Institute for Bioengineering of Catalonia, Barcelona, Spain; 9Department of Cell Biology, Physiology and Immunology, Facultat de Biologia, Universitat de Barcelona, Barcelona, Spain; 10Centro de Investigación Biomédica en Red sobre Enfermedades Neurodegenerativas (CIBERNED), Barcelona, Spain. This has now been amended in all online versions of the Article.
References
Tezil, T. & Basaga, H. Modulation of cell death in age-related diseases. Curr. Pharm. Des. 20, 3052–3067 (2014).
Scott, T. L., Rangaswamy, S., Wicker, C. A. & Izumi, T. Repair of oxidative DNA damage and cancer: recent progress in DNA base excision repair. Antioxid. Redox Signal. 20, 708–726 (2014).
Min, J. Y. et al. Staurosporin induces neurite outgrowth through ROS generation in HN33 hippocampal cell lines. J. Neural Transm. 113, 1821–1826 (2006).
Rieger, S. & Sagasti, A. Hydrogen peroxide promotes injury-induced peripheral sensory axon regeneration in the zebrafish skin. PLoS. Biol. 9, e1000621 (2011).
Gauron, C. et al. Sustained production of ROS triggers compensatory proliferation and is required for regeneration to proceed. Sci. Rep. 3, 2084 (2013).
Pirotte, N. et al. Reactive oxygen species in planarian regeneration: an upstream necessity for correct patterning and brain formation. Oxid. Med. Cell. Longev. 2015, 392476 (2015).
Ferreira, F., Luxardi, G., Reid, B. & Zhao, M. Early bioelectric activities mediate redox-modulated regeneration. Development 143, 4582–4594 (2016).
Meda, F. et al. Nerves control redox levels in mature tissues through Schwann cells and hedgehog signaling. Antioxid. Redox Signal. 24, 299–311 (2016).
Liang, R. & Ghaffari, S. Stem cells, redox signaling, and stem cell aging. Antioxid. Redox Signal. 20, 1902–1916 (2014).
Forsberg, K. & Di Giovanni, S. Cross talk between cellular redox status, metabolism, and p53 in neural stem cell biology. Neuroscientist 20, 326–342 (2014).
Le Belle, J. E. et al. Proliferative neural stem cells have high endogenous ROS levels that regulate self-renewal and neurogenesis in a PI3K/Akt-dependant manner. Cell. Stem Cell. 8, 59–71 (2011).
Buch, P. K. et al. In contrast to AAV-mediated Cntf expression, AAV-mediated Gdnf expression enhances gene replacement therapy in rodent models of retinal degeneration. Mol. Ther. 14, 700–709 (2006).
Burgoyne, J. R., Mongue-Din, H., Eaton, P. & Shah, A. M. Redox signaling in cardiac physiology and pathology. Circ. Res. 111, 1091–1106 (2012).
Wilson, C. et al. A feed-forward mechanism involving the NOX complex and RyR-mediated Ca2+ release during axonal specification. J. Neurosci. 36, 11107–11119 (2016).
D’Autreaux, B. & Toledano, M. B. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Nat. Rev. Mol. Cell Biol. 8, 813–824 (2007).
Holmstrom, K. M. & Finkel, T. Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat. Rev. Mol. Cell Biol. 15, 411–421 (2014).
Spencer, N. Y. & Engelhardt, J. F. The basic biology of redoxosomes in cytokine-mediated signal transduction and implications for disease-specific therapies. Biochemistry 53, 1551–1564 (2014).
Rishal, I. & Fainzilber, M. Axon–soma communication in neuronal injury. Nat. Rev. Neurosci. 15, 32–42 (2014).
Saito, A. & Cavalli, V. Signaling over distances. Mol. Cell. Proteom. 15, 382–393 (2016).
Kretz, A., Kugler, S., Happold, C., Bahr, M. & Isenmann, S. Excess Bcl-XL increases the intrinsic growth potential of adult CNS neurons in vitro. Mol. Cell. Neurosci. 26, 63–74 (2004).
Hausenloy, D. J. Cardioprotection techniques: preconditioning, postconditioning and remote conditioning (basic science). Curr. Pharm. Des. 19, 4544–4563 (2013).
Dezfulian, C., Garrett, M. & Gonzalez, N. R. Clinical application of preconditioning and postconditioning to achieve neuroprotection. Transl. Stroke Res. 4, 19–24 (2013).
Smith, D. S. & Skene, J. H. A transcription-dependent switch controls competence of adult neurons for distinct modes of axon growth. J. Neurosci. 17, 646–658 (1997).
Neumann, S. & Woolf, C. J. Regeneration of dorsal column fibers into and beyond the lesion site following adult spinal cord injury. Neuron 23, 83–91 (1999).
Giridharan, S. S. & Caplan, S. MICAL-family proteins: complex regulators of the actin cytoskeleton. Antioxid. Redox Signal. 20, 2059–2073 (2014).
IJkema-Paassen, J., Jansen, K., Gramsbergen, A. & Meek, M. F. Transection of peripheral nerves, bridging strategies and effect evaluation. Biomaterials 25, 1583–1592 (2004).
Jiang, F., Zhang, Y. & Dusting, G. J. NADPH oxidase-mediated redox signaling: roles in cellular stress response, stress tolerance, and tissue repair. Pharmacol. Rev. 63, 218–242 (2011).
ten Freyhaus, H. et al. Novel Nox inhibitor VAS2870 attenuates PDGF-dependent smooth muscle cell chemotaxis, but not proliferation. Cardiovasc. Res. 71, 331–341 (2006).
Huang, C. K., Zhan, L., Hannigan, M. O., Ai, Y. & Leto, T. L. P47phox-deficient NADPH oxidase defect in neutrophils of diabetic mouse strains, C57BL/6J-m db/db and db/+. J. Leukoc. Biol. 67, 210–215 (2000).
Roepstorff, K. et al. Stimulus-dependent regulation of the phagocyte NADPH oxidase by a VAV1, RAC1, and PAK1 signaling axis. J. Biol. Chem. 283, 7983–7993 (2008).
Sag, C. M. et al. Distinct regulatory effects of myeloid cell and endothelial cell NAPDH oxidase 2 on blood pressure. Circulation 135, 2163–2177 (2017).
Perry, R. B. et al. Subcellular knockout of importin β1 perturbs axonal retrograde signaling. Neuron 75, 294–305 (2012).
Lee, S. R. et al. Reversible inactivation of the tumor suppressor PTEN by H2O2. J. Biol. Chem. 277, 20336–20342 (2002).
Kwon, M. J. et al. CCL2 mediates neuron-macrophage interactions to drive proregenerative macrophage activation following preconditioning injury. J. Neurosci. 35, 15934–15947 (2015).
Kigerl, K. A. et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J. Neurosci. 29, 13435–13444 (2009).
Christie, K. J., Webber, C. A., Martinez, J. A., Singh, B. & Zochodne, D. W. PTEN inhibition to facilitate intrinsic regenerative outgrowth of adult peripheral axons. J. Neurosci. 30, 9306–9315 (2010).
Liu, K. et al. PTEN deletion enhances the regenerative ability of adult corticospinal neurons. Nat. Neurosci. 13, 1075–1081 (2010).
Hawkins, P. T., Davidson, K. & Stephens, L. R. The role of PI3Ks in the regulation of the neutrophil NADPH oxidase. Biochem. Soc. Symp. 74, 59–67 (2007).
Landry, W. D. & Cotter, T. G. ROS signalling, NADPH oxidases and cancer. Biochem. Soc. Trans. 42, 934–938 (2014).
Old, E. A. et al. Monocytes expressing CX3CR1 orchestrate the development of vincristine-induced pain. J. Clin. Invest. 124, 2023–2036 (2014).
Floriddia, E. M. et al. p53 regulates the neuronal intrinsic and extrinsic responses affecting the recovery of motor function following spinal cord injury. J. Neurosci. 32, 13956–13970 (2012).
Laurindo, F. R., Fernandes, D. C. & Santos, C. X. Assessment of superoxide production and NADPH oxidase activity by HPLC analysis of dihydroethidium oxidation products. Methods Enzymol. 441, 237–260 (2008).
Zhang, X., Goncalves, R. & Mosser, D. M. The isolation and characterization of murine macrophages. Curr. Protoc. Immunol. 83, 14.1.1–14.1.14 (2008).
Shin, J. E. Dual leucine zipper kinase is required for retrograde injury signaling and axonal regeneration. Neuron 74, 1015–1022 (2012).
Ueyama, T. et al. Superoxide production at phagosomal cup/phagosome through βI protein kinase C during FcγR-mediated phagocytosis in microglia. J. Immunol. 173, 4582–4589 (2004).
Ueyama, T. et al. Cooperation of p40phox with p47phox for Nox2-based NADPH oxidase activation during Fcγ Receptor (FcγR)-mediated phagocytosis. J. Biol. Chem. 286, 40693–40705 (2011).
Tuszynski, M. H. & Steward, O. Concepts and methods for the study of axonal regeneration in the CNS. Neuron 74, 777–791 (2012).
Acknowledgements
We acknowledge financial support from the Leverhulme Trust (S.D.G.); the Hertie Foundation (S.D.G.); Wings for Life (S.D.G. and M.F.); the DFG (S.D.G.); start-up funds from the Division of Brain Sciences, Imperial College London (S.D.G.); the European Research Council (Neurogrowth, M.F.); Minerva Foundation (M.F.) and the Israel Science Foundation (M.F.); and the British Heart Foundation (A.M.S.). The research was supported by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (S.D.G.). M.F. is the incumbent of the Chaya Professorial Chair in Molecular Neuroscience at the Weizmann Institute of Science. We thank M. Malcangio and E. Old (King’s College) for providing the Cx3cr1-null mice; W. M. Nauseef (University of Iowa) for critically discussing this manuscript; and G. Vizcay-Barrena at the Centre for Ultrastructural Imaging, King’s College London for technical support. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
A.H. performed and designed experiments, performed data analysis and wrote the manuscript; F.D.V. performed and designed experiments and performed data analysis; I.P. performed and designed experiments and performed data analysis; L.Z. performed experiments; E.T. performed experiments; G.K. performed experiments; T.H. performed experiments and edited the manuscript; M.C.D. performed data analysis; R.B.-T.P. performed experiments; C.X.C.S. performed experiments; A.N.K. designed experiments and provided technical support; R.A.F. designed experiments and provided technical support; J.A.D.R. supervised experiments and edited the manuscript; T.C. performed data analysis; V.L. supervised experiments and edited the manuscript; J.L.B. contributed to manuscript writing; A.M.S. supervised experiments and edited the manuscript; M.F. supervised experiments and edited the manuscript; S.D.G. designed experiments, performed data analysis and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A correction to this article is available online at https://doi.org/10.1038/s41556-018-0063-x.
Integrated supplementary information
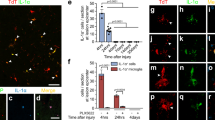
Supplementary Figure 1 ROS after nerve injury.
A. DHE fluorescence increases in DRG neurons 12 hours after SNC and remains elevated until 24 hours but not at 3 or 7 days compared to sham. Nerve delivery of NAC at the time of the crush blocks DHE fluorescence increase in DRG after SNC. Scale bar: 150µm B. Bar graphs show quantification of DHE fluorescence intensity after sham, SNC or SNC+NAC compared to Sham for each time point. Data is expressed as mean fold change of fluorescence intensity ± s.e.m. normalized vs Sham 12h. N= 3 animals per condition. (***p<0.001) indicate significant difference with respect to Sham 12h (ANOVA followed by Bonferroni test, p<0.0001). C. Hydro-Cy3 fluorescence increases in DRG neurons 12 hours after SNC while nerve delivery of NAC or DPI at the time of the crush block Hydro-Cy3 fluorescence increase in DRG 12 hours after SNC. Scale bar: 150µm. D. Bar graphs show quantification of Hydro-Cy3 fluorescence intensity after sham, SNC, SNC+NAC or SNC+DPI compared to Sham. Data is expressed as mean fold change of fluorescence intensity ± s.e.m. normalized vs Sham. N= 6 animals per condition. (***p=0.0005) indicate significant difference with respect to Sham (ANOVA followed by Bonferroni test, p<0.0001). Source data for B and D are provided in Supplementary Table 5.
Supplementary Figure 2 ROS control DRG neurite outgrowth including after a conditioning sciatic nerve lesion.
A. Shown is that NAC blocks DRG neurite outgrowth mediated by a conditioning lesion (SNC) (TUJ1 immunostaining, 12h), while mitoTEMPO does not. H2O2 phenocopies DRG regenerative growth elicited by SNC. Scale bar: 50µm. B. Bar graphs display average DRG neurite length after SNC, NAC, mitoTEMPO and H2O2. N= 3 animals per condition in triplicate. Mean neurite length per cell ± s.e.m. (***p<0.0001) Indicate significant difference with respect to Sham (ANOVA followed by Bonferroni test, p<0.0001). C. Delivery of H2O2 in the neurite compartment of a microfuidics cell culture chamber elicits DRG neurite outgrowth (TUJ1 immunostaining, 12h). Scale bar: 250µm D. Bar graphs display average DRG neurite length after H2O2. Mean fold change ± s.e.m. of average neurite length normalized vs Veh. N= 3 experiments per condition. (*p=0.0163) indicate significant difference with respect to Veh (ANOVA followed by Bonferroni test, p=0.0193). E. DRG outgrowth assay on a PDL/laminin or myelin substrate (12 hours) after SNC or ex vivo delivery of NAC+SNC or of H2O2 onto the sciatic nerve. Shown is an increase in DRG outgrowth (immunostaining for TUJ1) after SNC, which is phenocopied by H2O2 and inhibited by NAC. Scale bar: 50µm. F. Bar graphs show neurite length of DRG neurons. N=3 animals per condition in triplicate. Mean neurite length per cell ± s.e.m. (**p<0.01, ***p<0.001) indicate significant difference with respect to Sham or Sham vehicle (ANOVA followed by Bonferroni test, p<0.0001). Source data for B, D and F are provided in Supplementary Table 5.
Supplementary Figure 3 p47phox is induced in the nerve and DRG neurons after sciatic injury.
A-B. Representative immunofluorescence for p47phox (p47) in a sham (A) and injured-SNC (B) nerve 2h after surgery shows intense immunolabelling after injury (B) in a NF-200 positive sciatic nerve, while a very low signal is detectable in sham (A). Scale bar: 500µm b-b2. Shown is immunlabelling for p47phox in CD11b positive immune cells after SNC. Scale bar: 150µm C-F. Representative co-immunofluorescence for p-p47phox and NF-200 (C) or p-p47phox and ICAM-1 (D), showing very low expression of p-p47phox in the sciatic nerve (C) and in endothelial cells (D). p-p47phox is strongly co-expressed with NF-200 in the sciatic nerve 2h after SNC (E), and with ICAM-1+ endothelial cells (arrows, F) and within the nerve (F and inset Fi-high magnification). Scale bar: 300µm - 50µm G-J. Immunofluorescence for p-p47phox shows that p-p47phox expression is induced after SNC in DRG (H and J) compared to sham (G and I). Scale bar: 100µm. All experiments were performed at least three times from samples corresponding to independent animals.
Supplementary Figure 4 NOX2 complex is induced in the nerve after sciatic injury but not after spinal cord injury.
A-B. Representative immunofluorescence for gp91phox in a sham (A) and injured-SNC (B) nerve 2h after surgery shows intense immunolabelling after injury (B) in a Tuj-1 positive sciatic nerve, while a very low signal is detectable in sham (A). Scale bar: 100µm. C. Representative immunofluorescence for p-p47phox and NF-200 after a T10 spinal cord crush at the dorsal root entry zone (DREZ). Shown is strong expression of neuronal p-p47phox in proximity to the DREZ but not more distally along the dorsal root. Scale bar: 150µm. D-E. Representative immunofluorescence for p-p47phox and NF-200 after a T10 spinal cord crush shows undetectable p-p47phox immunosignal in the central nerve roots between 2 and 5 mm distally from the DREZ (D) and in the DRG (E). Scale bar: 150µm. All experiments were performed at least three times from samples corresponding to independent animals.
Supplementary Figure 5 Ncf1/p47phox expression is induced after spinal cord injury around the lesion site.
A-F. Representative immunofluorescence (spinal cord parasagittal section) for p-p47phox and NF-200 around the lesion site (asterisk) after a T10 spinal cord crush. Shown is strong expression of neuronal p-p47phox in proximity to the injury as opposed to an undetectable immunosignal in control spinal cords after laminectomy (G-H). Scale bar: 100µm. All experiments were performed at least three times from samples corresponding to independent animals.
Supplementary Figure 6 CX3CR1 is required for the expression of Ncf1/p47phox after nerve injury and is required for post-injury DRG outgrowth.
A, B. Representative immunofluorescence for p-p47phox in the sciatic nerve in proximity to the injury site (A) or the DRG (B) after SNC in WT and CX3CR1 null mice shows intense immunolabelling in WT, while a low signal is detectable CX3CR1 null mice. Scale bar: 150µm. C. Bar graphs show a significant reduction in anti-p-p47phox immunosignal in CX3CR1 null compared to WT mice after SNC. Mean fold change ± s.e.m. normalized vs WT (p-p47phox fluorescence intensity, arbitrary units). N=6 animals per condition. (** p<0.01) indicate significant difference with respect to WT (ANOVA followed by Bonferroni test, p=0.0096). D. Shown is DRG neurite outgrowth (TUJ1 immunostaining, 12h) that is significantly enhanced after a conditioning lesion (SNC) in WT but not in CX3CR1 null mice Scale bar: 50µm. E. Bar graphs display average DRG neurite length in WT versus CX3CR1 null mice including after a conditioning lesion (SNC). N= 3 animals per condition. Mean neurite length per cell ± s.e.m. (***p<0.001) indicate significant difference with respect to WT-sham (ANOVA followed by Bonferroni test, p<0.0001). Source data for C and E are provided in Supplementary Table 5.
Supplementary Figure 7 BMDM derived exosomes containing active NOX2 internalize into the neuron via a dynamin dependent mechanism.
A. Bar graph shows the percentage of GFP positive DRG neurons after plating in microfluidic chambers together with Ncf1-GFP electroporated BMDM and after dynasore versus vehicle (DMSO). B-C Z stack fluorescent images showing GFP expression of Ncf13xS/D-GFP after electroporation in LPS-activated BMDM, in macrophages (B), DRG neurites (C). Ncf1-GFP co-localizes with the endosomal marker Rab7 (B) and with Trk (C) (arrows). Scale bar: 25µm (B) and 100µm (C). Data is expressed as mean percentage of GFP+ DRG cells ± s.e.m. vs total DRG neurons on the grooves. N= 3 independent experiments. (**p<0.0088) indicate significant difference versus GFP-DMSO (two-sided Student’s T test). D-E. Dynasore delivered in BMDM conditioned media over DRG neurites after electroporation of GFP or Ncf1-GFP inhibits endocytosis of vesicles in DRG neurites. GFP and Ncf1-GFP co-localize with the endosomal marker Trk. Scale bar: 100µm. F. Bar graph shows the amount of GFP positive vesicles in DRG neurites after Veh or Dynasore (Dyna) pre-incubation. Data is expressed as average number of GFP+ puncta per 200µm of neurite (2-3 neurites per cell; 6-7 cells per well) ± s.e.m. N= 6 wells per condition. (**p<0.01, ***p<0.005) indicate significant difference versus GFP-Veh (ANOVA followed by Bonferroni test, p<0.0001). G. Dynasore delivered in culture media blocks endocytosis into DRG neurites of Alexa 594 labelled transferrin. Scale bar: 100µm. H. (a) BMDM stained with membrane dye PKH67 (green) and nuclear dye Hoechst (blue). (b) BMDM incubated with non-PKH67 stained exosomes. (c-d) BMDM incubated with exosomes stained with PKH67 (d shows the inset from c). (e-f) BMDM incubated with exosomes derived from BMDM that were pre-incubated with PKH67 (f shows the inset from e). Scale bars: 100µm (a, b, c and e) 10µm (d and f). Experiment performed three times with similar results. Source data for A and F are provided in Supplementary Table 5.
Supplementary Figure 8 Ncf1/p47phox and ROS are present in Rab7+ endosomes after injury in the sciatic nerve and in the DRG.
A. Confocal micrographs of immunofluorescence for p-p47phox, Rab7 and DAPI in the sciatic nerve 12h after SNC show that p-p47phox localizes in Rab7+ endosomes (arrowheads and inset). Scale bar: 60 µm. B. Confocal micrographs of immunofluorescence for p-p47phox, Rab7 and DAPI in the DRG 12h after SNC show that p-p47phox localizes in Rab7+ endosomes in the cell body of DRG neurons. Scale bar: 60µm. C. Confocal micrographs of immunofluorescence Rab7 combined with in vivo oxidative levels detection by Oxyburst-BSA and DAPI in the sciatic nerve 6h after SNC show that ROS production localizes in Rab7+ endosomes (arrowheads and inset). Scale bar: 12µm. D. Line plots show p-p47phox immunosignal after SNC as a function of distance from the injury site. Data is expressed as mean fluorescence intensity ± s.e.m. of p-p47phox. N= 3 animals per condition. (*p<0.05, **p<0.01, ***p<0.001) indicate significant difference with respect to WT after injury (ANOVA followed by Bonferroni test, p<0.0001). Source data is provided in Supplementary Table 5. E. Immunoblotting of endosomal fraction purified by Rab7 or control IgG immunoisolation of sciatic nerve extracts does not show expression of non-endosomal membrane organelles such as lysosomes (LAMP2), plasma membrane (CD71) or nucleus (H3). Experiment performed three times with similar results.
Supplementary Figure 9
Unprocessed images of all gels and blots
Supplementary information
Supplementary Information
Supplementary Figures 1–9 and Supplementary Table legends.
Supplementary Table 1
RNAseq dataset.
Supplementary Table 2
GO analysis.
Supplementary Table 3
KEGG pathways analysis.
Supplementary Table 4
ROS-dependent genes and relative GO and KEGG analysis.
Supplementary Table 5
Statistics source data.
Supplementary Table 6
Information on antibodies used in this study.
Rights and permissions
About this article
Cite this article
Hervera, A., De Virgiliis, F., Palmisano, I. et al. Reactive oxygen species regulate axonal regeneration through the release of exosomal NADPH oxidase 2 complexes into injured axons. Nat Cell Biol 20, 307–319 (2018). https://doi.org/10.1038/s41556-018-0039-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41556-018-0039-x
This article is cited by
-
Rab32 facilitates Schwann cell pyroptosis in rats following peripheral nerve injury by elevating ROS levels
Journal of Translational Medicine (2024)
-
Hepatoprotective effects of oligochitosan on hybrid groupers (Epinephelus lanceolatu ♂ × Epinephelus fuscoguttatus ♀) against Vibrio harvey infection via suppressing apoptosis-related pathways
Aquaculture International (2024)
-
Unleashing Axonal Regeneration Capacities: Neuronal and Non-neuronal Changes After Injuries to Dorsal Root Ganglion Neuron Central and Peripheral Axonal Branches
Molecular Neurobiology (2024)
-
Inflammatory Factor IL1α Induces Aberrant Astrocyte Proliferation in Spinal Cord Injury Through the Grin2c/Ca2+/CaMK2b Pathway
Neuroscience Bulletin (2024)
-
A swift expanding trend of extracellular vesicles in spinal cord injury research: a bibliometric analysis
Journal of Nanobiotechnology (2023)