Abstract
Deficits in cognitive control—that is, in the ability to withhold a default pre-potent response in favour of a more adaptive choice—are common in depression, anxiety, addiction and other mental disorders. Here we report proof-of-concept evidence that, in participants undergoing intracranial epilepsy monitoring, closed-loop direct stimulation of the internal capsule or striatum, especially the dorsal sites, enhances the participants’ cognitive control during a conflict task. We also show that closed-loop stimulation upon the detection of lapses in cognitive control produced larger behavioural changes than open-loop stimulation, and that task performance for single trials can be directly decoded from the activity of a small number of electrodes via neural features that are compatible with existing closed-loop brain implants. Closed-loop enhancement of cognitive control might remediate underlying cognitive deficits and aid the treatment of severe mental disorders.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The main data supporting the results in this study are available within the paper and its Supplementary Information. Pre-processed and anonymized neural and behavioural data are available through Zenodo at https://zenodo.org/record/5083120#.YOhvWehKiUk and https://zenodo.org/record/5085197#.YOhtouhKiUk.
Code availability
Analysis code is available at https://github.com/tne-lab/MSIT-Nature-Biomedical-Engineering. The closed-loop neurostimulation system has been released as open-source code and documented46, and the neural decoding and state-space modelling engines have similarly been released for open download (https://github.com/TRANSFORM-DBS/Encoder-Decoder-Paper and https://github.com/Eden-Kramer-Lab/COMPASS).
References
Roehrig, C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff. 35, 1130–1135 (2016).
Gordon, J. A. On being a circuit psychiatrist. Nat. Neurosci. 19, 1385–1386 (2016).
Insel, T. R. Disruptive insights in psychiatry: transforming a clinical discipline. J. Clin. Invest. 119, 700–705 (2009).
Mayberg, H. S. Targeted electrode-based modulation of neural circuits for depression. J. Clin. Invest. 119, 717–725 (2009).
Graat, I., Figee, M. & Denys, D. The application of deep brain stimulation in the treatment of psychiatric disorders. Int. Rev. Psychiatry 29, 178–190 (2017).
Sullivan, C. R. P., Olsen, S. & Widge, A. S. Deep brain stimulation for psychiatric disorders: from focal brain targets to cognitive networks. NeuroImage 225, 117515 (2021).
Scangos, K. W. & Ross, D. A. What we’ve got here is failure to communicate: improving interventional psychiatry with closed-loop stimulation. Biol. Psychiatry 84, e55–e57 (2018).
Widge, A. S., Malone, D. A. & Dougherty, D. D. Closing the loop on deep brain stimulation for treatment-resistant depression. Front. Neurosci. 12, 175 (2018).
Widge, A. S. & Miller, E. K. Targeting cognition and networks through neural oscillations: next-generation clinical brain stimulation. JAMA Psychiatry 76, 671–672 (2019).
Cuthbert, B. N. & Insel, T. R. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 11, 126 (2013).
Kirkby, L. A. et al. An amygdala-hippocampus subnetwork that encodes variation in human mood. Cell 175, 1688–1700.e14 (2018).
Veerakumar, A. et al. Field potential 1/f activity in the subcallosal cingulate region as a candidate signal for monitoring deep brain stimulation for treatment-resistant depression. J. Neurophysiol. 122, 1023–1035 (2019).
Widge, A. S. et al. Treating refractory mental illness with closed-loop brain stimulation: progress towards a patient-specific transdiagnostic approach. Exp. Neurol. 287, 461–472 (2017).
Badre, D. Cognitive control, hierarchy, and the rostro-caudal organization of the frontal lobes. Trends Cogn. Sci. 12, 193–200 (2008).
Grahek, I., Shenhav, A., Musslick, S., Krebs, R. M. & Koster, E. H. W. Motivation and cognitive control in depression. Neurosci. Biobehav. Rev. 102, 371–381 (2019).
Kouneiher, F., Charron, S. & Koechlin, E. Motivation and cognitive control in the human prefrontal cortex. Nat. Neurosci. 12, 939–945 (2009).
Solomon, M. et al. The neural substrates of cognitive control deficits in autism spectrum disorders. Neuropsychologia 47, 2515–2526 (2009).
Widge, A. S. et al. Deep brain stimulation of the internal capsule enhances human cognitive control and prefrontal cortex function. Nat. Commun. 10, 1–11 (2019).
Widge, A. S., Heilbronner, S. R. & Hayden, B. Y. Prefrontal cortex and cognitive control: new insights from human electrophysiology. F1000Research 8, F1000 (2019).
Cavanagh, J. F. & Frank, M. J. Frontal theta as a mechanism for cognitive control. Trends Cogn. Sci. 18, 414–421 (2014).
Sharpe, M. J. et al. An integrated model of action selection: distinct modes of cortical control of striatal decision making. Annu. Rev. Psychol. 70, 53–76 (2019).
Bari, A. & Robbins, T. W. Inhibition and impulsivity: behavioral and neural basis of response control. Prog. Neurobiol. 108, 44–79 (2013).
Burguière, E., Monteiro, P., Mallet, L., Feng, G. & Graybiel, A. M. Striatal circuits, habits, and implications for obsessive–compulsive disorder. Curr. Opin. Neurobiol. 30, 59–65 (2015).
Cohen, M. X. Midfrontal theta tracks action monitoring over multiple interactive time scales. NeuroImage 141, 262–272 (2016).
Ryman, S. G. et al. Impaired midline theta power and connectivity during proactive cognitive control in schizophrenia. Biol. Psychiatry 84, 675–683 (2018).
Provenza, N. R. et al. Decoding task engagement from distributed network electrophysiology in humans. J. Neural Eng. 16, 056015 (2019).
Smith, E. H. et al. Widespread temporal coding of cognitive control in the human prefrontal cortex. Nat. Neurosci. 22, 1883–1891 (2019).
Voytek, B. et al. Oscillatory dynamics coordinating human frontal networks in support of goal maintenance. Nat. Neurosci. 18, 1318–1324 (2015).
Haber, S. N. et al. Circuits, networks, and neuropsychiatric disease: transitioning from anatomy to imaging. Biol. Psychiatry 87, 318–327 (2020).
Haber, S. N. Corticostriatal circuitry. Dialogues Clin. Neurosci. 18, 7–21 (2016).
Makris, N. et al. Variability and anatomical specificity of the orbitofrontothalamic fibers of passage in the ventral capsule/ventral striatum (VC/VS): precision care for patient-specific tractography-guided targeting of deep brain stimulation (DBS) in obsessive compulsive disorder (OCD). Brain Imaging Behav. 10, 1054–1067 (2016).
Li, N. et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat. Commun. 11, 3364 (2020).
Dubreuil-Vall, L., Chau, P., Ruffini, G., Widge, A. S. & Camprodon, J. A. tDCS to the left DLPFC modulates cognitive and physiological correlates of executive function in a state-dependent manner. Brain Stimul. 12, 1456–1463 (2019).
Tyagi, H. et al. A randomized trial directly comparing ventral capsule and anteromedial subthalamic nucleus stimulation in obsessive-compulsive disorder: clinical and imaging evidence for dissociable effects. Biol. Psychiatry 85, 726–734 (2019).
Sheth, S. A. et al. Human dorsal anterior cingulate cortex neurons mediate ongoing behavioural adaptation. Nature 488, 218–221 (2012).
Wodlinger, B. et al. Ten-dimensional anthropomorphic arm control in a human brain−machine interface: difficulties, solutions, and limitations. J. Neural Eng. 12, 016011 (2015).
Hochberg, L. R. et al. Reach and grasp by people with tetraplegia using a neurally controlled robotic arm. Nature 485, 372–375 (2012).
Shenhav, A., Cohen, J. D. & Botvinick, M. M. Dorsal anterior cingulate cortex and the value of control. Nat. Neurosci. 19, 1286–1291 (2016).
Gillan, C. M., Kosinski, M., Whelan, R., Phelps, E. A. & Daw, N. D. Characterizing a psychiatric symptom dimension related to deficits in goal-directed control. eLife 5, e11305 (2016).
Bourget, D. et al. An implantable, rechargeable neuromodulation research tool using a distributed interface and algorithm architecture. In 7th International IEEE/EMBS Conference on Neural Engineering (NER) (IEEE, 2015).
Bach, D. R., Hoffmann, M., Finke, C., Hurlemann, R. & Ploner, C. J. Disentangling hippocampal and amygdala contribution to human anxiety-like behavior. J. Neurosci. 39, 8517–8526 (2019).
Mégevand, P. et al. The hippocampus and amygdala are integrators of neocortical influence: a corticocortical evoked potential study. Brain Connect. 7, 648–660 (2017).
Cavanagh, J. F. & Shackman, A. J. Frontal midline theta reflects anxiety and cognitive control: meta-analytic evidence. J. Physiol. Paris 109, 3–15 (2015).
Gibson, W. S. et al. The impact of mirth-inducing ventral striatal deep brain stimulation on functional and effective connectivity. Cereb. Cortex 27, 2183–2194 (2017).
Okun, M. S. et al. Deep brain stimulation in the internal capsule and nucleus accumbens region: responses observed during active and sham programming. J. Neurol. Neurosurg. Psychiatry 78, 310–314 (2007).
Zelmann, R. et al. CLoSES: a platform for closed-loop intracranial stimulation in humans. NeuroImage 223, 117314 (2020).
Bush, G. & Shin, L. M. The multi-source interference task: an fMRI task that reliably activates the cingulo-frontal-parietal cognitive/attention network. Nat. Protoc. 1, 308–313 (2006).
Smith, E. H. et al. Frequency-dependent representation of reinforcement-related information in the human medial and lateral prefrontal cortex. J. Neurosci. 35, 15827–15836 (2015).
McTeague, L. M. et al. Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. Am. J. Psychiatry 174, 676–685 (2017).
Computational Psychiatry (The MIT Press, 2016).
National Institute of Mental Health Strategic Plan for Research 48 (NIMH, 2020).
Wu, H. et al. Closing the loop on impulsivity via nucleus accumbens delta-band activity in mice and man. Proc. Natl Acad. Sci. USA 115, 192–197 (2018).
Wu, H. et al. Brain-responsive neurostimulation for loss of control eating: early feasibility study. Neurosurgery (2020); https://doi.org/10.1093/neuros/nyaa300
Martin, D. M., McClintock, S. M., Forster, J. J., Lo, T. Y. & Loo, C. K. Cognitive enhancing effects of rTMS administered to the prefrontal cortex in patients with depression: a systematic review and meta-analysis of individual task effects. Depress. Anxiety 34, 1029–1039 (2017).
Grisanzio, K. A. et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry 75, 201–209 (2017).
Inzlicht, M., Shenhav, A. & Olivola, C. Y. The effort paradox: effort is both costly and valued. Trends Cogn. Sci. 22, 337–349 (2018).
Klein, E. et al. Brain-computer interface-based control of closed-loop brain stimulation: attitudes and ethical considerations. Brain Comput. Interfaces 3, 140–148 (2016).
Cabrera, L. Y. et al. Authentic self and last resort: international perceptions of psychiatric neurosurgery. Cult. Med. Psychiatry https://doi.org/10.1007/s11013-020-09679-1 (2020).
Goering, S., Klein, E., Dougherty, D. D. & Widge, A. S. Staying in the loop: relational agency and identity in next-generation DBS for psychiatry. AJOB Neurosci. 8, 59–70 (2017).
Conrad, E. C., Humphries, S. & Chatterjee, A. Attitudes toward cognitive enhancement: the role of metaphor and context. AJOB Neurosci. 10, 35–47 (2019).
Bick, S. K. et al. Caudate stimulation enhances learning. Brain J. Neurol. 142, 2930–2937 (2019).
Prerau, M. J. et al. Characterizing learning by simultaneous analysis of continuous and binary measures of performance. J. Neurophysiol. 102, 3060–3072 (2009).
Paulk, A. C. et al. Bidirectional modulation of human emotional conflict resolution using intracranial stimulation. Preprint at bioRxiv https://doi.org/10.1101/825893 (2019).
Sani, O. G. et al. Mood variations decoded from multi-site intracranial human brain activity. Nat. Biotechnol. 36, 954–961 (2018).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A.-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160 (2009).
González-Villar, A. J. & Carrillo-de-la-Peña, M. T. Brain electrical activity signatures during performance of the Multisource Interference Task. Psychophysiology 54, 874–881 (2017).
Kleiner, M., Brainard, D. & Pelli, D. What’s new in Psychtoolbox-3. Perception 36, 1–16 (2007).
Dykstra, A. R. et al. Individualized localization and cortical surface-based registration of intracranial electrodes. NeuroImage 59, 3563–3570 (2012).
LaPlante, R. et al. The interactive electrode localization utility: software for automatic sorting and labeling of intracranial subdural electrodes. Int. J. Comput. Assist. Radiol. Surg. 12, 1829–1837 (2017).
Widge, A. S. et al. Predictors of hypomania during ventral capsule/ventral striatum deep brain stimulation. J. Neuropsychiatry Clin. Neurosci. 28, 38–44 (2015).
Basu, I. et al. A neural mass model to predict electrical stimulation evoked responses in human and non-human primate brain. J. Neural Eng. 15, 066012 (2018).
Basu, I. et al. Consistent linear and non-linear responses to invasive electrical brain stimulation across individuals and primate species with implanted electrodes. Brain Stimul. 12, 877–892 (2019).
Yousefi, A. et al. Decoding hidden cognitive states from behavior and physiology using a Bayesian approach. Neural Comput. 31, 1751–1788 (2019).
Yousefi, A. et al. COMPASS: an open-source, general-purpose software toolkit for computational psychiatry. Front. Neurosci. 12, 957 (2019).
Vaskov, A. K. et al. Cortical decoding of individual finger group motions using ReFIT Kalman filter. Front. Neurosci. 12, 751 (2018).
Ratcliff, R. & McKoon, G. The diffusion decision model: theory and data for two-choice decision tasks. Neural Comput. 20, 873–922 (2008).
Palmer, E. M., Horowitz, T. S., Torralba, A. & Wolfe, J. M. What are the shapes of response time distributions in visual search? J. Exp. Psychol. Hum. Percept. Perform. 37, 58–71 (2011).
Oostenveld, R., Fries, P., Maris, E. & Schoffelen, J.-M. FieldTrip: open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput. Intell. Neurosci. https://doi.org/10.1155/2011/156869 (2011).
Bastos, A. M. & Schoffelen, J.-M. A tutorial review of functional connectivity analysis methods and their interpretational pitfalls. Front. Syst. Neurosci. 9, 175 (2015).
Janca, R. et al. Detection of interictal epileptiform discharges using signal envelope distribution modelling: application to epileptic and non-epileptic intracranial recordings. Brain Topogr. 28, 172–183 (2015).
Cohen, M. X. & Donner, T. H. Midfrontal conflict-related theta-band power reflects neural oscillations that predict behavior. J. Neurophysiol. 110, 2752–2763 (2013).
Skarpaas, T. L., Jarosiewicz, B. & Morrell, M. J. Brain-responsive neurostimulation for epilepsy (RNS® System). Epilepsy Res. 153, 68–70 (2019).
Stanslaski, S. et al. Design and validation of a fully implantable, chronic, closed-loop neuromodulation device with concurrent sensing and stimulation. IEEE Trans. Neural Syst. Rehabil. Eng. 20, 410–421 (2012).
Acknowledgements
We thank A. Afzal, G. Belok, K. Farnes, J. Felicione, R. Franklin, A. Gilmour, A. Gosai, M. Moran, M. Robertson, C. Salthouse, D. Vallejo-Lopez and S. Zorowitz for technical assistance with data collection and the research participants, without whose generous help none of this would have been possible. This work was supported by grants from the Defense Advanced Research Projects Agency (DARPA) under Cooperative Agreement Number W911NF-14-2-0045 issued by the Army Research Organization (ARO) contracting office in support of DARPA’s SUBNETS Program, the National Institutes of Health (UH3NS100548, R01MH111917, R01MH086400, R01DA026297, R01EY017658, K24NS088568), Ellison Foundation, Tiny Blue Dot Foundation, MGH Executive Council on Research, OneMind Institute, and the MnDRIVE and Medical Discovery Team-Addictions initiatives at the University of Minnesota. The views, opinions and findings expressed are those of the authors. They should not be interpreted as representing the official views or policies of the Department of Defense, Department of Health and Human Services, any other branch of the US Government, or any other funding entity.
Author information
Authors and Affiliations
Contributions
A.S.W., D.D.D., E.N.E. and S.S.C. designed the study. I.B., A.Y., B.C., R.Z. and U.T.E. designed key software and tools required for data collection. K.K.E. and T.D. selected the psychometric scales administered to participants and provided unpublished data related to norming of those questionnaires. E.N.E. and G.R.C. performed all surgical procedures. A.S.W., I.B., B.C., R.Z., A.C.P., S.S.C. and D.S.W. collected data with participants during acute seizure monitoring. A.S.W., I.B., A.Y., A.C.P. and N.P. analysed data. I.B. and A.S.W. wrote the paper, with substantial inputs from A.Y., R.Z., A.C.P. and S.S.C. All authors had opportunities for critical input into and revision of the submitted manuscript, and approved its submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Biomedical Engineering thanks Edward Chang, Philip Star, Peter Tass and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 iEEG Recording montage.
Example recording montage from a single participant, with cortical parcellation overlaid. Electrode shanks represented by the grey dotted lines access a broad network covering multiple prefrontal structures, superficial and mesial temporal lobe, and striatum/internal capsule.
Extended Data Fig. 2 Accuracy results.
Accuracy during different stimulation experiments, for A) open-loop and B) closed-loop capsular stimulation. Boxes show the mean and confidence intervals for accuracy with stimulation at each site. Colours indicate stimulation sites as in the main text. The p-value above each bar represents a binomial exact test of accuracy compared to the non-stimulated baseline condition, with Benjamini-Hochberg false discovery rate correction. All accuracies are above 95%, with accuracy during stimulated blocks being very slightly higher in most cases. No results exceed chance significance. We did not have open- and closed-loop data from the same participants. To compare the CL and OL conditions, we therefore compared their accuracies across participants with a Fisher exact test for each of the three stimulation sites (L Dorsal, R Ventral, R Dorsal) that were used in both conditions. L Dorsal: p = 0.645. R Ventral: p = 0.440. R Dorsal: p = 0.655. These provide no evidence for a difference between OL and CL conditions. These results do not support a change in accuracy with any stimulation type. That is, the observed decrease in reaction times is a true performance improvement, not a shift along a speed-accuracy tradeoff. We were unable to analyse accuracy in the GLME framework because the differences between stimulation sites are so small as to make the models non-identifiable in all cases.
Extended Data Fig. 3 Cortical response to internal capsule stimulation.
Topographic structure of the internal capsule yields differential cortical effects from stimulation at different capsular sites. Before task-linked stimulation, we performed safety/perceptibility testing, where we repeatedly stimulated each potential site with brief 130 Hz pulse trains (see Methods). Each of those trains created an evoked response potential (ERP) in various cortical regions. For each participant, we collected all sEEG channels that were localized to grey matter of DLPFC or ACC. We then quantified the post-train ERP as the sum of the area under its polyphasic curve (AUC). We limited this analysis to channels ipsilateral to the site of stimulation. Each marker represents the mean log(AUC) in one participant. Boxes show the mean and confidence intervals for the ERP AUC from stimulation at each site. The stimulation sites that were more effective behaviorally produced the largest ERPs in these cognitive-control-associated regions, with right dorsal stimulation having the largest effects. (p-values represent t-test on the regression coefficients of a log-normal GLM, that is the same analysis used in main text Fig. 2). In the left hemisphere, dorsal stimulation produced larger responses than ventral stimulation, but this did not reach statistical significance given the small number of trials (5 test trains per participant). These results are consistent with the known topography of the internal capsule, where fibers that connect DLPFC and ACC to thalamus run in the dorsal-most part of the anterior limb, that is in close proximity to our chosen dorsal electrodes.
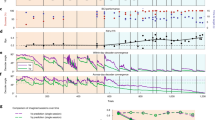
Extended Data Fig. 4 Open-loop and closed-loop effects in manifest data.
Effect of open-loop and closed-loop capsular stimulation on A) reaction time (RT) and B) Conflict related RT. Conflict related RT is calculated as the residual reaction time after subtracting the mean reaction time of the congruent trials in the same block, that is it has an expected value of 0 ms on non-conflict trials. We consider it as the closest raw/manifest data analogue of xconflict. We note, however, that both of these manifest RT variables include the Gaussian noise that is removed by the state-space filtering that produces xbase and xconflict. As such, the data in this figure are by definition noisier, and the analysis has lower statistical power. This leads to smaller effects in the open-loop results compared to main text Fig. 3. Closed-loop stimulation of the right dorsal internal capsule (our most effective open-loop intervention) was more effective than its open loop counterpart at reducing raw RT (the counterpart of xbase). Consistent with the specificity illustrated in main text Fig. 4 C, there was no advantage for closed-loop stimulation on the conflict-specific RT (the counterpart of xconflict). All formatting and graphical elements follow the conventions of main text Fig. 4.
Supplementary information
Rights and permissions
About this article
Cite this article
Basu, I., Yousefi, A., Crocker, B. et al. Closed-loop enhancement and neural decoding of cognitive control in humans. Nat. Biomed. Eng 7, 576–588 (2023). https://doi.org/10.1038/s41551-021-00804-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-021-00804-y
This article is cited by
-
Unraveling the mechanisms of deep-brain stimulation of the internal capsule in a mouse model
Nature Communications (2023)
-
Augmenting cognitive work: a review of cognitive enhancement methods and applications for operational domains
Cognition, Technology & Work (2022)