Abstract
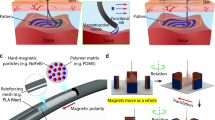
The rigidity and relatively primitive modes of operation of catheters equipped with sensing or actuation elements impede their conformal contact with soft-tissue surfaces, limit the scope of their uses, lengthen surgical times and increase the need for advanced surgical skills. Here, we report materials, device designs and fabrication approaches for integrating advanced electronic functionality with catheters for minimally invasive forms of cardiac surgery. By using multiphysics modelling, plastic heart models and Langendorff animal and human hearts, we show that soft electronic arrays in multilayer configurations on endocardial balloon catheters can establish conformal contact with curved tissue surfaces, support high-density spatiotemporal mapping of temperature, pressure and electrophysiological parameters and allow for programmable electrical stimulation, radiofrequency ablation and irreversible electroporation. Integrating multimodal and multiplexing capabilities into minimally invasive surgical instruments may improve surgical performance and patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The main data supporting the results in this study are available within the paper and its Supplementary Information. Source data for the figures are available from figshare with the identifier https://doi.org/10.6084/m9.figshare.12631835.
Code availability
The custom MATLAB software for data analysis can be downloaded from https://github.com/optocardiography.
Change history
10 September 2020
The Peer Review file originally published with this Article was an old version; the updated file is now available.
References
Biere, S. S. et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379, 1887–1892 (2012).
Bacha, E. & Kalfa, D. Minimally invasive paediatric cardiac surgery. Nat. Rev. Cardiol. 11, 24–34 (2014).
Martens, T. P. et al. Percutaneous cell delivery into the heart using hydrogels polymerizing in situ. Cell Transplant. 18, 297–304 (2009).
Oxley, T. J. et al. Minimally invasive endovascular stent-electrode array for high-fidelity, chronic recordings of cortical neural activity. Nat. Biotechnol. 34, 320–327 (2016).
Kim, D.-H. et al. Dissolvable films of silk fibroin for ultrathin conformal bio-integrated electronics. Nat. Mater. 9, 511–517 (2010).
Dukkipati, S. R. et al. Visual balloon-guided point-by-point ablation: reliable, reproducible, and persistent pulmonary vein isolation. Circ. Arrhythm. Electrophysiol. 3, 266–273 (2010).
Wazni, O., Wilkoff, B. & Saliba, W. Catheter ablation for atrial fibrillation. N. Engl. J. Med. 365, 2296–2304 (2011).
Kim, D.-H. et al. Materials for multifunctional balloon catheters with capabilities in cardiac electrophysiological mapping and ablation therapy. Nat. Mater. 10, 316–323 (2011).
Roche, E. T. et al. A light-reflecting balloon catheter for atraumatic tissue defect repair. Sci. Transl. Med. 7, 306ra149 (2015).
Lee, S. P. et al. Catheter-based systems with integrated stretchable sensors and conductors in cardiac electrophysiology. Proc. IEEE 103, 682–689 (2015).
Kim, Y., Parada, G. A., Liu, S. & Zhao, X. Ferromagnetic soft continuum robots. Sci. Robot. 4, eaax7329 (2019).
Ashammakhi, N. et al. Minimally invasive and regenerative therapeutics. Adv. Mater. 31, 1804041 (2019).
Fang, H. et al. Capacitively coupled arrays of multiplexed flexible silicon transistors for long-term cardiac electrophysiology. Nat. Biomed. Eng. 1, 0038 (2017).
Hua, Q. et al. Skin-inspired highly stretchable and conformable matrix networks for multifunctional sensing. Nat. Commun. 9, 244 (2018).
Chung, H. U. et al. Binodal, wireless epidermal electronic systems with in-sensor analytics for neonatal intensive care. Science 363, eaau0780 (2019).
Sharma, T., Aroom, K., Naik, S., Gill, B. & Zhang, J. X. Flexible thin-film PVDF-TrFE based pressure sensor for smart catheter applications. Ann. Biomed. Eng. 41, 744–751 (2013).
Klinker, L. et al. Balloon catheters with integrated stretchable electronics for electrical stimulation, ablation and blood flow monitoring. Extrem. Mech. Lett. 3, 45–54 (2015).
Lee, K. et al. Microneedle drug eluting balloon for enhanced drug delivery to vascular tissue. J. Control. Release 321, 174–183 (2020).
Liu, Z. et al. Transcatheter self-powered ultrasensitive endocardial pressure sensor. Adv. Funct. Mater. 29, 1807560 (2019).
Bergmann, O. et al. Dynamics of cell generation and turnover in the human heart. Cell 161, 1566–1575 (2015).
Xu, S. et al. Assembly of micro/nanomaterials into complex, three-dimensional architectures by compressive buckling. Science 347, 154–159 (2015).
Wu, J.-F. Scanning approaches of 2-D resistive sensor arrays: a review. IEEE Sens. J. 17, 914–925 (2016).
Gustafsson, S. E. Transient plane source techniques for thermal conductivity and thermal diffusivity measurements of solid materials. Rev. Sci. Instrum. 62, 797–804 (1991).
Webb, R. C. et al. Ultrathin conformal devices for precise and continuous thermal characterization of human skin. Nat. Mater. 12, 938–944 (2013).
Krishnan, S. R. et al. Epidermal electronics for noninvasive, wireless, quantitative assessment of ventricular shunt function in patients with hydrocephalus. Sci. Transl. Med. 10, eaat8437 (2018).
Yokoyama, K. et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythm. Electrophysiol. 1, 354–362 (2008).
Ariyarathna, N., Kumar, S., Thomas, S. P., Stevenson, W. G. & Michaud, G. F. Role of contact force sensing in catheter ablation of cardiac arrhythmias: evolution or history repeating itself? JACC Clin. Electrophysiol. 4, 707–723 (2018).
Yousef, H., Boukallel, M. & Althoefer, K. Tactile sensing for dexterous in-hand manipulation in robotics—a review. Sens. Actuator A 167, 171–187 (2011).
Costa, P., Ribeiro, S. & Lanceros-Mendez, S. Mechanical vs. electrical hysteresis of carbon nanotube/styrene–butadiene–styrene composites and their influence in the electromechanical response. Compos. Sci. Technol. 109, 1–5 (2015).
Jang, K.-I. et al. Self-assembled three dimensional network designs for soft electronics. Nat. Commun. 8, 15894 (2017).
Dewire, J. & Calkins, H. State-of-the-art and emerging technologies for atrial fibrillation ablation. Nat. Rev. Cardiol. 7, 129–138 (2010).
Maor, E. et al. Pulsed electric fields for cardiac ablation and beyond: A state-of-the-art review. Heart Rhythm 16, 1112–1120 (2019).
Hjouj, M. & Rubinsky, B. Magnetic resonance imaging characteristics of nonthermal irreversible electroporation in vegetable tissue. J. Membr. Biol. 236, 137–146 (2010).
Ramer, O. Integrated optic electrooptic modulator electrode analysis. IEEE J. Quantum Electron. 18, 386–392 (1982).
Nath, S., DiMarco, J. P. & Haines, D. E. Basic aspects of radiofrequency catheter ablation. J. Cardiovasc. Electrophysiol. 5, 863–876 (1994).
McClintock, R. Strain gauge calibration device for extreme temperatures. Rev. Sci. Instrum. 30, 715–718 (1959).
Hur, S.-G., Kim, D.-J., Kang, B.-D. & Yoon, S.-G. Effect of the deposition temperature on temperature coefficient of resistance in CuNi thin film resistors. J. Vac. Sci. Technol. B 22, 2698–2701 (2004).
Pikul, J. et al. Stretchable surfaces with programmable 3D texture morphing for synthetic camouflaging skins. Science 358, 210–214 (2017).
Gloschat, C. et al. RHYTHM: an open source imaging toolkit for cardiac panoramic optical mapping. Sci. Rep. 8, 2921 (2018).
Aras, K. K., Faye, N. R., Cathey, B. & Efimov, I. R. Critical volume of human myocardium necessary to maintain ventricular fibrillation. Circ. Arrhythm. Electrophysiol. 11, e006692 (2018).
Rodenhauser, A. et al. PFEIFER: Preprocessing framework for electrograms intermittently fiducialized from experimental recordings. J. Open Source Softw. 3, 472 (2018).
Acknowledgements
I.R.E. and J.A.R. acknowledge support from the Leducq Foundation project RHYTHM and R01-HL141470. This project was supported by the National Institute of General Medical Sciences of the National Institutes of Health under grant nos. P41 GM103545 and R24 GM136986, and the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI). K.A. acknowledges support from the National Institutes of Health K99-HL148523-01A1. X.C. acknowledges support from National Key R&D Program of China (grant 2018YFA0108100) and China Scholarship Council. This work made use of the NUFAB facility of Northwestern University’s NUANCE Center, which has received support from the Soft and Hybrid Nanotechnology Experimental (SHyNE) Resource (NSF ECCS-1542205); the MRSEC program (NSF DMR-1720139) at the Materials Research Center; the International Institute for Nanotechnology (IIN); the Keck Foundation; and the State of Illinois, through the IIN.
Author information
Authors and Affiliations
Contributions
M.H., L.C., K.A., R.G., Y.H., I.R.E. and J.A.R. conceived the ideas, designed the experiments and wrote the manuscript; L.C., K.L. and G.Y. performed mechanical, electrical and thermal modelling. M.H., C. Liang, B.S., J.-H.K., Q.Y., Y.M., E.S., J.M.B., Y.L., C. Liu and J.B.M. fabricated the devices; M.H., X.C., H.Z., B.S., W.B., Y.M. and W.L. performed in vitro data collection and analysis; M.H., K.A., H.Z. and N.R.F. performed ex vivo data collection and analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary notes, figures, tables and video captions.
Supplementary Video 1
Temperature mapping using the multiplexing circuit with proper grounding.
Supplementary Video 2
Pressure mapping on a porcine heart.
Supplementary Video 3
Electrogram mapping on a rabbit heart.
Supplementary Video 4
Temperature mapping during radiofrequency ablation.
Supplementary Video 5
Electrogram mapping on a human heart.
Rights and permissions
About this article
Cite this article
Han, M., Chen, L., Aras, K. et al. Catheter-integrated soft multilayer electronic arrays for multiplexed sensing and actuation during cardiac surgery. Nat Biomed Eng 4, 997–1009 (2020). https://doi.org/10.1038/s41551-020-00604-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-020-00604-w
This article is cited by
-
A self-powered intracardiac pacemaker in swine model
Nature Communications (2024)
-
Emerging sensing and modeling technologies for wearable and cuffless blood pressure monitoring
npj Digital Medicine (2023)
-
Highly sensitive and broadband meta-mechanoreceptor via mechanical frequency-division multiplexing
Nature Communications (2023)
-
Multi-parameter e-skin based on biomimetic mechanoreceptors and stress field sensing
npj Flexible Electronics (2023)
-
Soft bioelectronics for the management of cardiovascular diseases
Nature Reviews Bioengineering (2023)