Abstract
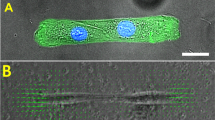
In asthma, the contraction of the airway smooth muscle and the subsequent decrease in airflow involve a poorly understood set of mechanical and biochemical events. Organ-level and molecular-scale models of the airway are frequently based on purely mechanical or biochemical considerations and do not account for physiological mechanochemical couplings. Here, we present a microphysiological model of the airway that allows for the quantitative analysis of the interactions between mechanical and biochemical signals triggered by compressive stress on epithelial cells. We show that a mechanical stimulus mimicking a bronchospastic challenge triggers the marked contraction and delayed relaxation of airway smooth muscle, and that this is mediated by the discordant expression of cyclooxygenase genes in epithelial cells and regulated by the mechanosensor and transcriptional co-activator Yes-associated protein. A mathematical model of the intercellular feedback interactions recapitulates aspects of obstructive disease of the airways, which include pathognomonic features of severe difficult-to-treat asthma. The microphysiological model could be used to investigate the mechanisms of asthma pathogenesis and to develop therapeutic strategies that disrupt the positive feedback loop that leads to persistent airway constriction.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The authors declare that all data supporting the findings of this study are available within the paper and its Supplementary Information. The source data for the figures in this study are available in figshare (https://doi.org/10.6084/m9.figshare.7639898)83.
References
Bates, J. Toward a nonlinear network theory of complex disease. In International Conference on Complex Systems 1–7 (NECSI, 2006).
Venegas, J. G. et al. Self-organized patchiness in asthma as a prelude to catastrophic shifts. Nature 434, 777–782 (2005).
Winkler, T. & Venegas, J. G. Self-organized patterns of airway narrowing. J. Appl. Physiol. 110, 1482–1486 (2011).
Suki, B. & Frey, U. Temporal dynamics of recurrent airway symptoms and cellular random walk. J. Appl. Physiol. 95, 2122–2127 (2003).
Mauroy, B., Filoche, M., Weibel, E. & Sapoval, B. An optimal bronchial tree may be dangerous. Nature 427, 633–636 (2004).
Alam, R. & Gorska, M. M. Mitogen‐activated protein kinase signalling and ERK1/2 bistability in asthma. Clin. Exp. Allergy 41, 149–159 (2011).
Lambert, R. K., Wilson, T. A., Hyatt, R. E. & Rodarte, J. R. A computational model for expiratory flow. J. Appl. Physiol. 52, 44–56 (1982).
Anafi, R. C. & Wilson, T. A. Airway stability and heterogeneity in the constricted lung. J. Appl. Physiol. 91, 1185–1192 (2001).
Donovan, G. M., Sneyd, J. & Tawhai, M. H. The importance of synergy between deep inspirations and fluidization in reversing airway closure. PLoS ONE 7, e48552 (2012).
Huber, H. L. & Koessler, K. K. The pathology of bronchial asthma. Arch. Intern. Med. 30, 689–760 (1922).
James, A. L., Paré, P. D. & Hogg, J. C. The mechanics of airway narrowing in asthma. Am. Rev. Respir. Dis. 139, 242–246 (1989).
Wiggs, B. R., Hrousis, C. A., Drazen, J. M. & Kamm, R. D. On the mechanism of mucosal folding in normal and asthmatic airways. J. Appl. Physiol. 83, 1814–1821 (1997).
Okada, S. F. et al. Inflammation promotes airway epithelial ATP release via calcium-dependent vesicular pathways. Am. J. Respir. Cell Mol. Biol. 49, 814–820 (2013).
Savla, U., Sporn, P. H. & Waters, C. M. Cyclic stretch of airway epithelium inhibits prostanoid synthesis. Am. J. Physiol. Lung Cell. Mol. Physiol. 273, L1013–L1019 (1997).
Arold, S. P., Malavia, N. & George, S. C. Mechanical compression attenuates normal human bronchial epithelial wound healing. Respir. Res. 10, 9 (2009).
Copland, I. B., Reynaud, D., Pace-Asciak, C. & Post, M. Mechanotransduction of stretch-induced prostanoid release by fetal lung epithelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 291, L487–L495 (2006).
Burnstock, G. Purine-mediated signalling in pain and visceral perception. Trends Pharmacol. Sci. 22, 182–188 (2001).
Ferguson, D., Kennedy, I. & Burton, T. ATP is released from rabbit urinary bladder epithelial cells by hydrostatic pressure changes–possible sensory mechanism? J. Physiol. 505, 503–511 (1997).
Cuthbert, M. Effect on airways resistance of prostaglandin E1 given by aerosol to healthy and asthmatic volunteers. Br. Med. J. 4, 723–726 (1969).
Sweatman W. & Collier H. Effects of prostaglandins on human bronchial muscle. Nature 217, 69 (1968).
Mathé, A. A. & Hedqvist, P. Effect of prostaglandins F2α and E2 on airway conductance in healthy subjects and asthmatic patients. Am. Rev. Respir. Dis. 111, 313–320 (1975).
Hanna, C., Bach, M., Pare, P. & Schellenberg, R. Slow-reacting substances (leukotrienes) contract human airway and pulmonary vascular smooth muscle in vitro. Nature 290, 343–344 (1981).
Xiong, W. & Ferrell, J. E. A positive-feedback-based bistable ‘memory module’ that governs a cell fate decision. Nature 426, 460–465 (2003).
Tian, X.-J., Zhang, X.-P., Liu, F. & Wang, W. Interlinking positive and negative feedback loops creates a tunable motif in gene regulatory networks. Phys. Rev. E 80, 011926 (2009).
Lavoie, T. L. et al. Dilatation of the constricted human airway by tidal expansion of lung parenchyma. Am. J. Respir. Crit. Care Med. 186, 225–232 (2012).
LaPrad, A. S., Szabo, T. L., Suki, B. & Lutchen, K. R. Tidal stretches do not modulate responsiveness of intact airways in vitro. J. Appl. Physiol. 109, 295–304 (2010).
LaPrad, A. S., West, A. R., Noble, P. B., Lutchen, K. R. & Mitchell, H. W. Maintenance of airway caliber in isolated airways by deep inspiration and tidal strains. J. Appl. Physiol. 105, 479–485 (2008).
Noble, P. B. et al. Responsiveness of the human airway in vitro during deep inspiration and tidal oscillation. J. Appl. Physiol. 110, 1510–1518 (2011).
Park, J.-A. et al. Unjamming and cell shape in the asthmatic airway epithelium. Nat. Mater. 14, 1040–1048 (2015).
Noble, P., Sharma, A., McFawn, P. & Mitchell, H. Elastic properties of the bronchial mucosa: epithelial unfolding and stretch in response to airway inflation. J. Appl. Physiol. 99, 2061–2066 (2005).
Huh, D. et al. Reconstituting organ-level lung functions on a chip. Science 328, 1662–1668 (2010).
West, A. R. et al. Development and characterization of a 3D multicell microtissue culture model of airway smooth muscle. Am. J. Physiol. Lung Cell. Mol. Physiol. 304, L4–L16 (2012).
Benam, K. H. et al. Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nat. Methods 13, 151–157 (2016).
Noble, P. B., McFawn, P. K. & Mitchell, H. W. Responsiveness of the isolated airway during simulated deep inspirations: effect of airway smooth muscle stiffness and strain. J. Appl. Physiol. 103, 787–795 (2007).
Vanhoutte, P. M. Epithelium-derived relaxing factor(s) and bronchial reactivity. J. Allergy Clin. Immunol. 83, 855–861 (1989).
Park, J.-A. & Tschumperlin, D. J. Chronic intermittent mechanical stress increases MUC5AC protein expression. Am. J. Respir. Cell Mol. Biol. 41, 459–466 (2009).
Tschumperlin, D. J. et al. Mechanotransduction through growth-factor shedding into the extracellular space. Nature 429, 83–86 (2004).
Wang, N., Butler, J. P. & Ingber, D. E. Mechanotransduction across the cell surface and through the cytoskeleton. Science 260, 1124–1127 (1993).
Wang, N. et al. Cell prestress. I. Stiffness and prestress are closely associated in adherent contractile cells. Am. J. Physiol. Cell Physiol. 282, C606–C616 (2002).
An, S. S., Laudadio, R. E., Lai, J., Rogers, R. A. & Fredberg, J. J. Stiffness changes in cultured airway smooth muscle cells. Am. J. Physiol. Cell Physiol. 283, C792–C801 (2002).
An, S. S., Fabry, B., Trepat, X., Wang, N. & Fredberg, J. J. Do biophysical properties of the airway smooth muscle in culture predict airway hyperresponsiveness? Am. J. Respir. Cell Mol. Biol. 35, 55–64 (2006).
Ressler, B., Lee, R. T., Randell, S. H., Drazen, J. M. & Kamm, R. D. Molecular responses of rat tracheal epithelial cells to transmembrane pressure. Am. J. Physiol. Lung Cell. Mol. Physiol. 278, L1264–L1272 (2000).
Swartz, M., Tschumperlin, D. J., Kamm, R. & Drazen, J. Mechanical stress is communicated between different cell types to elicit matrix remodeling. Proc. Natl Acad. Sci. USA 98, 6180–6185 (2001).
Yoon, A.-R. et al. COX-2 dependent regulation of mechanotransduction in human breast cancer cells. Cancer Biol. Ther. 16, 430–437 (2015).
Obermajer, N., Muthuswamy, R., Lesnock, J., Edwards, R. P. & Kalinski, P. Positive feedback between PGE2 and COX2 redirects the differentiation of human dendritic cells toward stable myeloid-derived suppressor cells. Blood 118, 5498–5505 (2011).
Dupont, S. et al. Role of YAP/TAZ in mechanotransduction. Nature 474, 179–183 (2011).
Halder, G., Dupont, S. & Piccolo, S. Transduction of mechanical and cytoskeletal cues by YAP and TAZ. Nat. Rev. Mol. Cell Biol. 13, 591–600 (2012).
An, S. S. et al. An inflammation-independent contraction mechanophenotype of airway smooth muscle in asthma. J. Allergy Clin. Immunol. 138, 294 (2016).
Tilley, S. L. et al. Receptors and pathways mediating the effects of prostaglandin E2 on airway tone. Am. J. Physiol. Lung Cell. Mol. Physiol. 284, L599–L606 (2003).
O’Sullivan, M. J. et al. Epithelial cells induce a cyclo-oxygenase-1–dependent endogenous reduction in airway smooth muscle contractile phenotype. Am. J. Respir. Cell Mol. Biol. 57, 683–691 (2017).
Pfeuty, B. & Kaneko, K. The combination of positive and negative feedback loops confers exquisite flexibility to biochemical switches. Phys. Biol. 6, 046013 (2009).
Wenzel, S. E. et al. Proceedings of the ATS workshop on refractory asthma. Am. J. Respir. Crit. Care Med. 162, 2341–2351 (2000).
Bateman, E. et al. Global strategy for asthma management and prevention: GINA executive summary. Eur. Respir. J. 31, 143–178 (2008).
Zhou, J., Alvarez-Elizondo, M. B., Botvinick, E. & George, S. C. Local small airway epithelial injury induces global smooth muscle contraction and airway constriction. J. Appl. Physiol. 112, 627–637 (2012).
Zhou, J., Alvarez-Elizondo, M. B., Botvinick, E. & George, S. C. Adenosine A1 and prostaglandin e receptor 3 receptors mediate global airway contraction after local epithelial injury. Am. J. Respir. Cell Mol. Biol. 48, 299–305 (2013).
Orehek, J., Douglas, J. S. & Bouhuys, A. Contractile responses of the guinea-pig trachea in vitro: modification by prostaglandin synthesis-inhibiting drugs. J. Pharmacol. Exp. Ther. 194, 554–564 (1975).
Gao, Y. & Vanhoutte, P. M. Responsiveness of the guinea pig trachea to stretch: role of the epithelium and cyclooxygenase products. J. Appl. Physiol. 75, 2112–2116 (1993).
Kullmann, F. A., Shah, M. A., Birder, L. A. & de Groat, W. C. Functional TRP and ASIC-like channels in cultured urothelial cells from the rat. Am. J. Physiol. Renal Physiol. 296, F892–F901 (2009).
Fronius, M. & Clauss, W. G. Mechano-sensitivity of ENaC: may the (shear) force be with you. Pflügers Arch. 455, 775–785 (2008).
Zhang, W. K. et al. Mechanosensitive gating of CFTR. Nat. Cell Biol. 12, 507–512 (2010).
Coste, B. et al. Piezo1 and Piezo2 are essential components of distinct mechanically activated cation channels. Science 330, 55–60 (2010).
Storch, U., Mederos y Schnitzler, M. & Gudermann, T. G protein-mediated stretch reception. Am. J. Physiol. Heart Circ. Physiol. 302, H1241–H1249 (2012).
Seminario-Vidal, L. et al. Rho signaling regulates pannexin 1-mediated ATP release from airway epithelia. J. Biol. Chem. 286, 26277–26286 (2011).
Genetos, D. C., Geist, D. J., Liu, D., Donahue, H. J. & Duncan, R. L. Fluid shear‐induced ATP secretion mediates prostaglandin release in MC3T3‐E1 osteoblasts. J. Bone Miner. Res. 20, 41–49 (2005).
Chand, N. & Eyre, P. Atypical (relaxant) response to histamine in cat bronchus. Agents Actions. 7, 183–190 (1977).
Chand, N. & Eyre, P. Histamine relaxes constricted trachea and bronchi of horse. Vet. Res. Commun. 1, 85–90 (1977).
Chand, N. & DeRoth, L. Actions of histamine and other substances on the airway smooth muscle of swine (in vitro). Vet. Res. Commun. 2, 151–155 (1978).
Stickland, M. K., Rowe, B. H., Spooner, C. H., Vandermeer, B. & Dryden, D. M. Effect of warm-up exercise on exercise-induced bronchoconstriction. Med. Sci. Sports Exerc. 44, 383–391 (2012).
Szczeklik, A. & Stevenson, D. D. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J. Allergy Clin. Immunol. 111, 913–921 (2003).
Picado, C. Aspirin‐intolerant asthma: role of cyclo‐oxygenase enzymes. Allergy 57, 58–60 (2002).
Hanania, N. A., Dickey, B. F. & Bond, R. A. Clinical implications of the intrinsic efficacy of beta-adrenoceptor drugs in asthma: full, partial and inverse agonism. Curr. Opin. Pulm. Med. 16, 1–5 (2010).
Ruan, Y. C., Zhou, W. & Chan, H. C. Regulation of smooth muscle contraction by the epithelium: role of prostaglandins. Physiology 26, 156–170 (2011).
Bultitude, M., HILLs, N. & Shuttleworth, K. Clinical and experimental studies on the action of prostaglandins and their synthesis inhibitors on detrusor muscle in vitro and in vivo. Br. J. Urol. 48, 631–637 (1976).
Lundström, V., Gréen, K. & Svanborg, K. Endogenous prostaglandins in dysmenorrhea and the effect of prostaglandin synthetase inhibitors (PGSI) on uterine contractility. Acta Obstet. Gynecol. Scand. 58, 51–56 (1979).
Trepat, X. et al. Universal physical responses to stretch in the living cell. Nature 447, 592 (2007).
Panettieri, R., Murray, R., DePalo, L., Yadvish, P. & Kotlikoff, M. A human airway smooth muscle cell line that retains physiological responsiveness. Am. J. Physiol. Cell Physiol. 256, C329–C335 (1989).
Kilic, O. et al. Brain-on-a-chip model enables analysis of human neuronal differentiation and chemotaxis. Lab Chip 16, 4152–4162 (2016).
Fabry, B. et al. Scaling the microrheology of living cells. Phys. Rev. Lett. 87, 148102 (2001).
Benjamini Y. & Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B 57, 289–300 (1995).
Van Koppen, C. et al. Beta adrenoceptor binding and induced relaxation in airway smooth muscle from patients with chronic airflow obstruction. Thorax 44, 28–35 (1989).
Aizawa, H., Miyazaki, N., Shigematsu, N. & Tomooka, M. A possible role of airway epithelium in modulating hyperresponsiveness. Br. J. Pharmacol. 93, 139–145 (1988).
Healy, Z. R. et al. Divergent responses of chondrocytes and endothelial cells to shear stress: cross-talk among COX-2, the phase 2 response, and apoptosis. Proc. Natl Acad. Sci. USA 102, 14010–14015 (2005).
Kilic O. et al. Dataset for A microphysiological model of the bronchial airways reveals the interplay of mechanical and biochemical signals in bronchospasm. Figshare https://doi.org/10.6084/m9.figshare.7639898 (2019).
Acknowledgements
This work was supported by National Institutes of Health grants U01 CA155758 (A.L), U54 CA209992 (A.L), R01 HL107361 (S.S.A) and P01 HL114471 (R.A.P., S.B.L. and S.S.A.). O.K. was a recipient of the American Heart Association Postdoctoral Fellowship (grant no. 13POST17140090). This work was also supported by a grant from the American Asthma Foundation (A.L. and S.S.A). S.S.A. was also supported by a Discovery Award and a Catalyst Award from the Johns Hopkins University.
Author information
Authors and Affiliations
Contributions
O.K., S.S.A. and A.L. conceptualized the work. O.K. carried out the device and platform design and fabrication. O.K., H.M.Y., A.Y., S.R.S., A.R.-V. and H.C. carried out the experiments. O.K. and A.L. performed the theoretical modelling. All authors contributed to data analysis, discussion and interpretation. O.K., S.S.A. and A.L. wrote and revised the manuscript with input from all authors.
Corresponding authors
Ethics declarations
Competing interests
O.K, S.S.A. and A.L. have a pending patent (US Patent Application 15/739,639) related to the work in this manuscript. The remaining authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary figures, tables and legend for Supplementary Video 1.
Supplementary Video 1
Tidal breathing in bronchial-chip
Rights and permissions
About this article
Cite this article
Kilic, O., Yoon, A., Shah, S.R. et al. A microphysiological model of the bronchial airways reveals the interplay of mechanical and biochemical signals in bronchospasm. Nat Biomed Eng 3, 532–544 (2019). https://doi.org/10.1038/s41551-019-0366-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-019-0366-7
This article is cited by
-
Thrombin induces IL-8/CXCL8 expression by DCLK1-dependent RhoA and YAP activation in human lung epithelial cells
Journal of Biomedical Science (2022)