Abstract
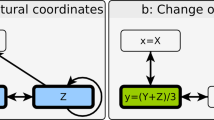
Current methods of drug dosing rely on physical parameters (such as sex, age and weight) that do not account for genetic and physiological differences among individual patients. These differences can greatly affect how drugs are processed in the body and can result in ineffective underdosing or toxic overdosing. Here, we describe a generalizable closed-loop system consisting of a biosensor, controller and infusion pump, and a model of drug pharmacokinetics that continuously monitors and adjusts the concentration of a given drug in the body. As proof of concept, we demonstrate that the system can maintain the concentration of doxorubicin—a widely used chemotherapy drug—in live rabbits and rats at any desired set point and in real time, while automatically compensating for large pharmacokinetic differences among individual animals and stabilizing dramatic perturbations arising from acute drug–drug interactions. The feedback-loop system opens up the possibility of tightly controlled, patient-specific dosing of chemotherapeutics and other drugs within narrow therapeutic windows.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Baker, S. D. et al. Role of body surface area in dosing of investigational anticancer agents in adults, 1991–2001. J. Natl Cancer I. 94, 1883–1888 (2002).
Gurney, H. How to calculate the dose of chemotherapy. Brit. J. Cancer 86, 1297–1302 (2002).
Khalil, F. & Läer, S. Physiologically based pharmacokinetic modeling: methodology, applications, and limitations with a focus on its role in pediatric drug development. J. Biomed. Biotechnol. 2011, 907461 (2011).
Mathijssen, R. H. J. et al. Flat-fixed dosing versus body surface area based dosing of anticancer drugs in adults: does it make a difference? Oncologist 12, 913–923 (2007).
Muller, P. Y. & Milton, M. N. The determination and interpretation of the therapeutic index in drug development. Nat. Rev. Drug Discov. 11, 751–761 (2012).
Gao, B., Klumpen, H.-J. & Gurney, H. Dose calculation of anticancer drugs. Expert Opin. Drug Met. 4, 1307–1319 (2008).
Undevia, S. D., Gomez-Abuin, G. & Ratain, M. J. Pharmacokinetic variability of anticancer agents. Nat. Rev. Cancer 5, 447–458 (2005).
Johnston, A. & Holt, D. W. Therapeutic drug monitoring of immunosuppressant drugs. Brit. J. Clin. Pharmaco. 47, 339–350 (1999).
van Gelder, T., van Schaik, R. H. & Hesselink, D. A. Pharmacogenetics and immunosuppressive drugs in solid organ transplantation. Nat. Rev. Nephrol. 10, 725–731 (2014).
Burns, M. Management of narrow therapeutic index drugs. J. Thromb. Thrombolys. 7, 137–143 (1999).
Cohen, M. R. Pharmacists’ role in ensuring safe and effective hospital use of insulin. Am. J. Health-Syst. Ph. 67, S17–S21 (2010).
Kanto, J. & Gepts, E. Pharmacokinetic implications for the clinical use of propofol. Clin. Pharmacokinet. 17, 308–326 (1989).
Relling, M. V. & Evans, W. E. Pharmacogenomics in the clinic. Nature 526, 343–350 (2015).
Momper, J. D. & Wagner, J. A. Therapeutic drug monitoring as a component of personalized medicine: applications in pediatric drug development. Clin. Pharmacol. Ther. 95, 138–140 (2014).
Zanger, U. M. Pharmacogenetics—challenges and opportunities ahead. Front. Pharmacol. 1, 112 (2010).
Wang, B., Canestaro, W. J. & Choudhry, N. K. Clinical evidence supporting pharmacogenomic biomarker testing provided in US Food and Drug Administration drug labels. JAMA Intern. Med. 174, 1938–1944 (2014).
Touw, D. J., Neef, C., Thomson, A. H. & Vinks, A. A. Cost-effectiveness of therapeutic drug monitoring: a systematic review. Ther. Drug Monit. 27, 10–17 (2005).
Swen, J. J. et al. Translating pharmacogenomics: challenges on the road to the clinic. PLoS Med. 4, 1317–1324 (2007).
DiFrancesco, R. et al. Quality assessment for therapeutic drug monitoring in AIDS Clinical Trials Group (ACTG 5146): a multicenter clinical trial. Ther. Drug Monit. 32, 458–466 (2010).
Klonoff, D. C. Smart sensors for maintaining physiologic homeostasis. J. Diabetes Sci. Technol. 5, 470–475 (2011).
Uemura, K. & Sugimachi, M. Automated cardiovascular drug infusion system to control hemodynamics. Adv. Biomed. Eng. 2, 32–37 (2013).
Struys, M. M. et al. Comparison of closed-loop controlled administration of propofol using Bispectral Index as the controlled variable versus ‘standard practice’ controlled administration. Anesthesiology 95, 6–17 (2001).
Doyle, F. J., Huyett, L. M., Lee, J. B., Zisser, H. C. & Dassau, E. Closed-loop artificial pancreas systems: engineering the algorithms. Diabetes Care 37, 1191–1197 (2014).
Ferguson, B. S. et al. Real-time, aptamer-based tracking of circulating therapeutic agents in living animals. Sci. Transl. Med. 5, 213ra165 (2013).
Chatelut, E. et al. Dose banding as an alternative to body surface area-based dosing of chemotherapeutic agents. Brit. J. Cancer 107, 1100–1106 (2012).
Eksborg, S., Strandler, H.-S., Edsmyr, F., Näslund, I. & Tahvanainen, P. Pharmacokinetic study of IV infusions of adriamycin. Eur. J. Clin. Pharmacol. 28, 205–212 (1985).
Dobbs, N. A. et al. Gender affects doxorubicin pharmacokinetics in patients with normal liver biochemistry. Cancer Chemoth. Pharm. 36, 473–476 (1995).
Elis, A. et al. Doxorubicin in lymphoma: association between pharmacokinetic variability and clinical response. Ther. Drug Monit. 32, 50–52 (2010).
Barpe, D. R., Rosa, D. D. & Froehlich, P. E. Pharmacokinetic evaluation of doxorubicin plasma levels in normal and overweight patients with breast cancer and simulation of dose adjustment by different indexes of body mass. Eur. J. Pharm. Sci. 41, 458–463 (2010).
Ang, K. H., Chong, G. & Li, Y. PID control system analysis, design, and technology. IEEE T. Contr. Syst. T. 13, 559–576 (2005).
Greene, R. F., Collins, J. M., Jenkins, J. F., Speyer, J. L. & Myers, C. E. Plasma pharmacokinetics of adriamycin and adriamycinol: implications for the design of in vitro experiments and treatment protocols. Cancer Res. 43, 3417–3421 (1983).
Camaggi, C. M. et al. Epirubicin and doxorubicin comparative metabolism and pharmacokinetics. A cross-over study. Cancer Chemoth. Pharm. 21, 221–228 (1988).
Mross, K. et al. Pharmacokinetics and metabolism of epidoxorubicin and doxorubicin in humans. J. Clin. Oncol. 6, 517–526 (1988).
Mross, K., Mayer, U., Hamm, K., Burk, K. & Hossfeld, D. K. Pharmacokinetics and metabolism of iodo-doxorubicin and doxorubicin in humans. Eur. J. Clin. Pharmacol. 39, 507–513 (1990).
Schoukroun-Barnes, L. R. et al. Reagentless, structure-switching, electrochemical aptamer-based sensors. Annu. Rev. Anal. Chem. 9, 163–181 (2016).
Thorslund, S., Sanchez, J., Larsson, R., Nikolajeff, F. & Bergquist, J. Functionality and stability of heparin immobilized onto poly(dimethylsiloxane). Colloid. Surface B 45, 76–81 (2005).
Maniez-Devos, D. M., Baurain, R., Trouet, A. & Lesne, M. Doxorubicin pharmacokinetics in the rabbit. J. Pharmacol. 16, 159–169 (1985).
Scripture, C. D. & Figg, W. D. Drug interactions in cancer therapy. Nat. Rev. Cancer 6, 546–558 (2006).
Watanabe, K. Current chemotherapeutic approaches for hepatoblastoma. Int. J. Clin. Oncol. 18, 955–961 (2013).
Najjar, T. A. O. & Saad, S. Y. Effect of treatment schedule on the toxicity and pharmacokinetics of cisplatin-doxorubicin combination in rabbits. J. Egypt. Nat. Cancer I. 12, 259–265 (2000).
Rahman, A., Carmichael, D., Harris, M. & Roh, J. K. Comparative pharmacokinetics of free doxorubicin and doxorubicin entrapped in cardiolipin liposomes. Cancer Res. 46, 2295–2299 (1986).
Ueda, Y. et al. Comparison of efficacy, toxicity and pharmacokinetics of free adriamycin and adriamycin linked to oxidized dextran in rats. Chem. Pharm. Bull. 37, 1639–1641 (1989).
Bendetowicz, A. V, Béguin, S., Caplain, H. & Hemker, H. C. Pharmacokinetics and pharmacodynamics of a low molecular weight heparin (enoxaparin) after subcutaneous injection, comparison with unfractionated heparin—a three way cross over study in human volunteers. Thromb. Haemostasis 71, 305–313 (1994).
Barbour, A., Scaglione, F. & Derendorf, H. Class-dependent relevance of tissue distribution in the interpretation of anti-infective pharmacokinetic/pharmacodynamic indices. Int. J. Antimicrob. Ag. 35, 431–438 (2010).
Absalom, A. R., Mani, V., De Smet, T. & Struys, M. M. R. F. Pharmacokinetic models for propofol—defining and illuminating the devil in the detail. Brit. J. Anaesth. 103, 26–37 (2009).
Williams, C. K. & Maddox, R. R. Implementation of an i.v. medication safety system. Am. J. Health-Syst. Ph. 62, 530–536 (2005).
Hortobágyi, G. N. Anthracyclines in the treatment of cancer. Drugs 54, (Suppl. 4) 1–7 (1997).
Singal, P. K. & Iliskovic, N. Doxorubicin-induced cardiomyopathy. N. Engl. J. Med. 339, 900–905 (1998).
Minotti, G., Menna, P., Salvatorelli, E., Cairo, G. & Gianni, L. Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol. Rev. 56, 185–229 (2004).
Fulbright, J. M., Huh, W., Anderson, P. & Chandra, J. Can anthracycline therapy for pediatric malignancies be less cardiotoxic? Curr. Oncol. Rep. 12, 411–419 (2010).
Hutson, J. R. et al. Pharmacokinetic and pharmacogenetic determinants and considerations in chemotherapy selection and dosing in infants. Expert Opin. Drug Met. 8, 709–722 (2012).
Grosman, B., Dassau, E., Zisser, H. C., Jovanovic, L. & Doyle, F. J. Zone model predictive control: a strategy to minimize hyper- and hypoglycemic events. J. Diabetes Sci. Technol. 4, 961–975 (2010).
Greenblatt, D. J., Sellers, E. M. & Koch-Weser, J. Importance of protein binding for the interpretation of serum or plasma drug concentrations. J. Clin. Pharmacol. 22, 259–263 (1982).
Pavlovic, E. et al. Microfluidic device architecture for electrochemical patterning and detection of multiple DNA sequences. Langmuir 24, 1102–1107 (2008).
Turksoy, K., Bayrak, E. S., Quinn, L., Littlejohn, E. & Cinar, A. Multivariable adaptive closed-loop control of an artificial pancreas without meal and activity announcement. Diabetes Technol. The. 15, 386–400 (2013).
Magni, L. et al. Run-to-run tuning of model predictive control for type 1 diabetes subjects: in silico trial. J. Diabetes Sci. Technol. 3, 1091–1098 (2009).
Ho, J. S. et al. Wireless power transfer to deep-tissue microimplants. Proc. Natl Acad. Sci. USA 111, 7974–7979 (2014).
Farra, R. et al. First-in-human testing of a wirelessly controlled drug delivery microchip. Sci. Transl. Med. 4, 122ra21 (2012).
Phares, N., White, R. J. & Plaxco, K. W. Improving the stability and sensing of electrochemical biosensors by employing trithiol-anchoring groups in a six-carbon self-assembled monolayer. Anal. Chem. 81, 1095–1100 (2009).
Herbert, J. M. et al. The antiaggregating and antithrombotic activity of clopidogrel is potentiated by aspirin in several experimental models in the rabbit. Thromb. Haemostasis 80, 512–518 (1998).
Zehnder, A. M., Hawkins, M. G., Trestrail, E. A., Holt, R. W. & Kent, M. S. Calculation of body surface area via computed tomography-guided modeling in domestic rabbits (Oryctolagus cuniculus). Am. J. Vet. Res. 73, 1859–1863 (2012).
Gilpin, D. A. Calculation of a new Meeh constant and experimental determination of burn size. Burns 22, 607–611 (1996).
Acknowledgements
We are grateful for the financial support of the Garland Initiative, Army Research Office (W911NF-10-2-0114, W911QY-15-C-0026) and the W. M. Keck Foundation Medical Research Program. We thank B. Eisenhower, D. Hoggarth, J. Somerson, D. Mamerow, A. Pressman, G. Marcus, S. Hall, M. Eisenstein, M. Nakamoto, K. Plaxco and F. Doyle for helpful discussions. We also thank A. Griffin, R. Wynn, and M. Garcia at the UCSB Animal Resource Center for their technical expertise and assistance with the animal studies.
Author information
Authors and Affiliations
Contributions
B.S.F. and H.T.S. conceived of the project. P.L.M. and B.S.F. designed the experiments, fabricated the sensors and created the control and simulation software. P.L.M. directed the animal studies, performed the controller simulations and analysed the data. D.M. and K.L.P. performed all animal procedures in the studies. T.E.K. assisted in design of, provided supervision for, and wrote the protocols for the animal studies. P.L.M. and H.T.S wrote and edited the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Information
Supplementary figures (PDF 1427 kb)
Rights and permissions
About this article
Cite this article
Mage, P., Ferguson, B., Maliniak, D. et al. Closed-loop control of circulating drug levels in live animals. Nat Biomed Eng 1, 0070 (2017). https://doi.org/10.1038/s41551-017-0070
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41551-017-0070
This article is cited by
-
A massively parallel screening platform for converting aptamers into molecular switches
Nature Communications (2023)
-
Opportunities and challenges in the diagnostic utility of dermal interstitial fluid
Nature Biomedical Engineering (2023)
-
A high-dimensional microfluidic approach for selection of aptamers with programmable binding affinities
Nature Chemistry (2023)
-
Pre-equilibrium biosensors as an approach towards rapid and continuous molecular measurements
Nature Communications (2022)
-
Computational systems biology in disease modeling and control, review and perspectives
npj Systems Biology and Applications (2022)