ABSTRACT
In Zambia limited access to adequate water and sanitation is a key developmental challenge, particularly for rapidly expanding peri-urban areas. During 2016–2017, a cross-sectional household survey was conducted among 12,500 households representing ~60,000 individuals to assess the burden of household diarrheal and respiratory disease and to measure water, sanitation, and hygiene (WASH) characteristics in Lusaka, Zambia. We found that socio-economic factors, including having an additional household member, having children <5 years old in the household, living in a rental home, and higher annual household expenditure were associated with diarrhea and respiratory illness. We also found an increased risk for diarrhea associated with a number of WASH-related factors–such as not covering all water storage containers, not using soap for handwashing, having an unimproved sanitation facility, and utilizing a heavily shared toilet (≥18 people). Detectable free chlorine residual in household stored water and more hours of water availability per day were associated with reduced odds of waterborne illness. In all, 75% of household stored water was contaminated with E. coli and households consuming less water (<20 L/day per person) for all purposes had lower odds of diarrhea than households consuming more water—these findings highlight the need for enhanced WASH services within densely populated peri-urban areas and the importance of achieving universal access to safely managed water and sanitation services.
Similar content being viewed by others
Introduction
Currently, 55% of the world’s population lives in urban areas, a figure which will approach 70% in 20501. Global population size is projected to reach nearly 10 billion persons by 2050, with the majority of population growth occurring in urban and peri-urban areas (PUAs) in low-income countries in Asia and Africa1. Many of these cities lack the basic water and sanitation infrastructure to support rapidly expanding populations2. In 2015, 2.1 billion people lacked safely managed drinking water and 4.5 billion lacked safely managed sanitation services3. Limited access to water and sanitation services results in diarrheal illness, which causes 500,000 deaths among children <5 years old annually4. It also contributes to respiratory illness5,6,7, which caused 880,000 deaths among children <5 years old in 20168. These negative consequences of rapid urbanization are often felt disproportionately by the urban poor, who typically reside in low-income, peri-urban areas, also known as “informal settlements,” that are located on the outskirts of cities and are frequently beyond the reach of basic infrastructure9. As of 2014, 881 million people were living in informal settlements worldwide10.
In Zambia, where ~40% of the population lives in urban areas, limited access to adequate water and sanitation is one of the key developmental challenges11. The problem is most intense in the capital city of Lusaka, where water and sanitation infrastructure—built in the 1960s and 1970s for a population of 300,000—is insufficient to meet the needs of the current population of approximately two million12. The situation is especially acute in PUAs in Lusaka, which are home to approximately 70% of Lusaka’s population13. In 2010, only 24% of peri-urban households had piped water to the home or plot, and nearly 60% collected their water from community sources such as kiosks13. Access to sanitation infrastructure in these areas is similarly low, with nearly 88% of households using pit latrines13.
Many key global health indicators are poor in Zambia. For example, the mortality rate for children <5 years old was 60 per 1000 live births in 2017, which is above the average of 43 per 1000 live births in the World Banks’s low and middle income countries aggregate grouping11. Sixty-one percent of deaths in Zambia in 2016 were caused by communicable diseases and maternal, prenatal, and nutrition conditions compared with 50% in the World Bank’s low-income countries aggregate grouping11. These indicators are directly or indirectly related to the status of water supply and sanitation infrastructure and underscore the universal necessity of equitable access to adequate water and sanitation services.
In 2013, the Millennium Challenge Corporation (MCC), a US development agency, in partnership with the Government of Zambia (Millennium Challenge Account Zambia [MCAZ]), began designing a $350 million upgrade and extension of the water, sanitation, and drainage infrastructure in Lusaka to increase population access to potable water, sanitation, and flood protection14. Prior to the construction of new water and sanitation infrastructure, the U.S. Centers for Disease Control and Prevention (CDC) collected data from 2016 to 2017 on waterborne illness in households and water, sanitation, and hygiene (WASH) variables to better understand conditions in peri-urban communities of Lusaka. Our objectives were to characterize water and sanitation conditions in households, estimate the burden of diarrheal and respiratory disease in the household, and explore the factors associated with these illnesses in PUAs of Lusaka, Zambia, during 2016–17.
Results
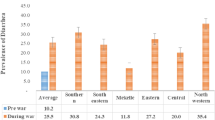
We approached 16,059 households and successfully completed interviews at 12,511 representing 60,575 individuals (8079 <5 years old) in Lusaka. Table 1 summarizes the characteristics of 12,511 households recruited and interviewed for the cross-sectional study. Of 12,511 households, 26% (n = 3278) reported having at least one household member with waterborne illness (either diarrhea or respiratory illness) in the past 7 days; 13% (n = 1600) for diarrhea and 16% (n = 1993) for respiratory illness only (Table 1). Specifically, of 60,575 individuals, 3% (n = 1827) and 4% (n = 2370) experienced diarrheal and respiratory illness respectively in the past 7 days. For children <5 years old (n = 8079), 8% (n = 648) had diarrhea, and 10% (n = 800) had respiratory illness in the past 7 days (individual level data not shown).
More than three-quarters of heads of households (78%) were male; 59% (n = 7403) of participants had only attained a primary or lower level of education. The median household size was five persons (Interquartile range or IQR: 3–6), and approximately half of all households (51%, n = 6346) included children <5 years old. Less than a third of households (30%, n = 3342) owned their house.
For WASH characteristics, 17% (n = 2066) of households were accessing unimproved sources for drinking water. Water was available from the source for a median of 9 h per day and surveyed households reported consuming a median of 20 liters of water per day per capita for all uses (drinking, cooking, cleaning, bathing, etc.). Nearly all households (n = 12,362; 98.8%) stored their drinking water; 83% (n = 9877) of households covered all of their household water storage containers. Only 13% (n = 1573) of households reported treating their stored water (e.g., chlorinating, boiling, or filtering) on the day of interview. Nineteen percent (n = 2270) used flush toilets; however, only 1% (n = 137) of households used flush toilets connected to a sewered network. A fifth of households (21%) reported their toilet being shared heavily (≥18 people). Sixty-one percent (n = 7599) of household respondents reported using soap when washing their hands and were able to produce soap for observation. Of the subset of households that were randomly selected for water quality testing of household stored water (n = 3147), 75% (n = 2355) had drinking water that tested positive for E. coli and 92% (n = 2884) had FCR < 0.2 mg/L. The distributions of demographic and WASH characteristics were similar between the overall sample of households (n = 12,511) and the subset of households that received water quality testing of household stored water (n = 3147; Table 1).
In multivariable logistic regression models, having an additional household member, having one or more children <5 years old in the household, living in a rental home, and household expenditure >3rd quartile were all associated with waterborne, diarrhea, and respiratory illness (Table 2); i.e., the odds of having waterborne illness were 5% higher when household size increased by 1 (OR: 1.05, 95% CI: 1.03–1.08), 50% higher when the household included one or more children <5 years old (OR: 1.50, 95% CI: 1.36–1.66), 46% higher when living in a rental home (OR: 1.46, 95% CI: 1.29–1.65) and 20% higher when household expenditure was above the 3rd quartile (OR: 1.20, 95% CI: 1.08–1.34). Households that reported not using soap when handwashing were at higher odds of waterborne illness (OR: 1.20, 95% CI: 1.10–1.32) and diarrhea (OR: 1.18, 95% CI: 1.05–1.34). Having an unimproved sanitation facility was a risk for diarrheal illness (OR: 1.37, 95% CI: 1.06–1.77) and utilizing a heavily shared toilet (≥18 people) was a risk factor for both waterborne illness (OR: 1.18, 95% CI: 1.06–1.31) and diarrhea (OR: 1.33, 95% CI: 1.17–1.53). Higher education level (tertiary or secondary vs. primary or lower) was inversely associated with waterborne illness and respiratory illness; achieving a secondary vs. primary or lower education level was inversely associated with diarrhea. Households with annual expenditures in the top quartile had a 17–23% higher odds of having waterborne, diarrheal, and respiratory illness. Households observed to have water storage containers uncovered or partially covered were exclusively associated with diarrhea (OR: 1.25, 95% CI 1.06–1.46). Interestingly, households consuming less water for all purposes (<20 L/day per person in the household) had lower odds of diarrhea (OR: 0.87, 95% CI: 0.77–0.98; Table 2).
Using the same models for the subset of households that received water quality testing of household stored water (n = 3147), we found a similar pattern of association between the three illness outcomes and demographic variables of household size, having a child under 5 in the household, and home ownership (Table 3). Household expenditure and higher education level was no longer associated with any illness outcomes. Among WASH factors, the model results were also similar: handwashing without soap remained a risk factor for waterborne illness (OR: 1.23, 95% CI: 1.05–1.44), utilizing unimproved sanitation was a risk factors for diarrhea (OR: 1.62, 95% CI: 1.00–2.63) and heavy toilet sharing (≥18 people) was a risk factor for diarrhea (OR: 1.42, 95% CI: 1.07–1.88). Also similar to the full data analysis, consuming less water for all purposes (<20 L/day vs >20 L/day) was negatively associated with diarrhea (OR: 0.70, 95% CI: 0.55–0.89). Having fewer hours of water availability per day (<7 vs >11) was a risk factor for waterborne illness (OR: 1.58, 95% CI: 1.00–2.49) and having a detectable FCR > 0.2 mg/L was associated with lower odds of waterborne illness (OR: 0.65, 95% CI: 0.45–0.94). The odds of all three illness outcome variables was estimated higher for households that had detectable E. coli in stored household water; however, it did not achieve statistical significance in the models (Table 3).
Discussion
The findings from this cross-sectional study in peri-urban Lusaka, Zambia suggest that waterborne illness, diarrheal illness, and respiratory illness were positively associated with socioeconomic-related factors such as larger household size (especially having young children in the household), renting homes, and higher household expenditures. Additionally, for waterborne illness and diarrheal illness, WASH-related indicators including not using soap when handwashing, not covering all household water storage containers, using an unimproved sanitation facility, heavy toilet sharing, and higher water consumption for all purposes were identified as risk factors. WASH-related factors were not significant contributors to respiratory illness in this population as they have been in other studies5,6,7.
Focusing on sanitation, while the majority of households surveyed had access to “improved” sanitation, most utilized pit latrines with slabs (70%); 18% had access to flush toilets and only 1% were connected to a sewered network (Table 1). Of those households without flush toilets, the majority were using shared facilities with ~20% of these households sharing their facility with an estimated 18 or more people. This “heavy sharing” of sanitation facilities was a significant risk factor for having one or more members of the household reporting diarrhea or waterborne illness in the week before interview, which is consistent with other studies linking shared sanitation to diarrheal disease risk15,16,17. Utilizing an unimproved sanitation facility was also found to be a risk factor for diarrheal illness in this population (Tables 2 and 3), which is consistent with other studies18,19,20. Pit latrines in peri-urban Lusaka are generally unlined and waste is rarely transported offsite, resulting in full pits being abandoned and new ones dug in close proximity to obsolete pits. Lusaka has a high water table and utilization of shallow wells for household water is common21. The high density of unlined pit latrines leads to contamination of groundwater sources in peri-urban areas of Lusaka and highlights the need to increase access to safely managed sanitation services. Furthermore, sewer connections have been widely shown to decrease diarrhea; one meta-analysis found a 31% reduction in diarrheal morbidity among households with access to a toilet with sewer connection22. Studies of sewerage installations in large cities in Brazil and Iran have also demonstrated a decrease in diarrheal prevalence23,24. The results from this cross-sectional evaluation point to the potential health gains that could result by decreasing a peri-urban population’s reliance on shared, latrine-based sanitation and increasing access to sewerage connections and network, in alignment with the United Nations’ Sustainable Development Goal SDG 6.2 for universal access to safely managed sanitation25.
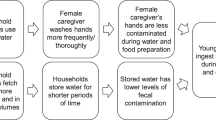
For water supply metrics, while accessing unimproved drinking water sources (unprotected well, private borehole, surface water, bottled water) was not found to be a significant risk factor for diarrheal illness in this population, higher water consumption per person (defined as ≥20 L/day) for all purposes was a significant risk factor. This result stands in contrast to previous studies that have found increased water consumption to be protective against diarrheal disease26,27. Almost all households in our study reported having to store water and the high percentage of household stored water samples testing positive for the presence of E. coli, an indicator of fecal contamination, may partially explain the counter-intuitive finding that lower consumption of water was protective against diarrheal disease. Other studies utilizing quantitative microbial risk assessment (QMRA) have found that in low-income, urban environments with poor sanitation, excreta can contaminate multiple environmental exposure pathways aside from drinking water (e.g. foods, surfaces, bathing water, etc.) and this contributes to total fecal exposure28,29. It is possible that the high proportion of household stored water found to be contaminated with E. coli contributed to the finding of less water consumption for all purposes (drinking, cooking, and bathing) being protective against diarrheal disease. Additionally, those households not covering all of their stored water containers also had higher odds of diarrheal illness. These results illustrate the potential impact of household- or plot-level piped water access on health by reducing the need for potable water storage. The importance of water supply has been shown in meta-analyses that found water supply interventions—such as installing standpipes or household connections—reduce diarrheal illness by 25–37%30,31,32. A meta-regression found a relative risk for diarrheal disease of 0.86 (95% CI: 0.72, 1.03) from interventions that provided piped water connections (with non-continuous flow) to households that previously relied on improved community sources (e.g., stand pipes), and a relative risk of 0.21 (95% CI: 0.08, 0.56) in water interventions that provided continuous, high quality piped water connections to households that previously relied on improved community sources31. While the illness reduction from a continuous connection is based on limited evidence from a single study, the meta-regression identifies the health benefits that can be achieved from household connections that provide continuous water supply, and our results from the cross-sectional evaluation demonstrate the potential risks associated with water storage. Among the subset of households with water quality testing of stored household water, our study found that detectable free chlorine residual was associated with reduced odds of waterborne illness as was increased water availability, findings with direct relevance to the new SDG ladders for safely managed drinking water.
The socio-economic findings from this study are generally consistent with previous studies33,34,35 with the exception of the observed association between higher expenditure and all illness outcomes, which is not readily explained. Of note, household expenditure and education-related variables, and several of the WASH-related factors that were associated with diarrhea in the full models dropped out as significant factors in the sub-set analysis for households that received water quality testing. This suggests that after accounting for objective household water quality measures, these factors’ independent contribution to explain the household illnesses were no longer significant. With the inclusion of objective water quality variables, having a child <5 years old, utilizing unimproved sanitation and heavy toilet sharing were the strongest risk factors for diarrhea, while consuming less water for all purposes remained protective. Having detectable free chlorine residual and more hours of water availability per day were associated with lower odds of waterborne illness. The directionality of factors (risk or protective) did not change for any of the outcomes when including water quality parameters.
This study has several limitations. First, it relied on self-reported measures of waterborne illness. Self-reported health outcome data, here for diarrhea and respiratory illness, are inherently biased and contain validity issues. Recall bias may lead to under-reporting not just around the key health outcome indicators but also around other covariates like water consumption and household expenditure. However, we tried to minimize recall bias by keeping recall of illness to a 7-day window and by rigorous training of field staff on case definitions and consistency in survey administration. Second, certain survey questions, particularly around water treatment and handwashing, are subject to over-reporting by social desirability bias. Finally, this study was non-experimental in design.
Several large, well-designed intervention studies have found no effect of WASH-related interventions on diarrhea and child growth36,37 with one demonstrating moderate impact38. Randomized, experimental interventions that provide water and sewer connections are few given the inherent cost of infrastructure and equity considerations. This study, while not an impact evaluation, found an increased risk for diarrhea associated with a number of WASH-related factors including heavy toilet sharing, utilizing unimproved sanitation facilities, sub-optimal water storage practices, handwashing without soap, and increased consumption of water for all purposes, the majority of which was contaminated with E. coli. The results presented from this study demonstrate the basic need and potential health gains that can result from water and sanitation infrastructure investments in urban and peri-urban areas. As underscored by the findings from this cross-sectional study, sustained investment in the WASH infrastructure sector is imperative to achieve the targets of SDG 6—universal access to safely managed water and sanitation by 2030—and is critically needed in many of the world’s fastest growing urban and peri-urban areas.
Methods
Study design
Between 17 October 2016 and 26 October 2017, we conducted a cross-sectional household survey to assess health, water, and sanitation conditions among households in PUAs across Lusaka. Data collection occurred for a full year to account for the seasonal differences in key health outcomes such as diarrheal incidence39,40,41,42,43,44,45,46. A two-stage cluster sampling strategy was employed, with the primary sampling units being the “Standard Enumeration Areas” (SEAs) provided by the Zambian Central Statistics Office. SEAs are the smallest enumeration units in Lusaka, each representing ~175 households on average. Two hundred and seventy-five peri-urban SEAs were selected using a probability proportionate to size (PPS) sampling strategy. The same number of households per SEA was then randomly selected to let all households have the same overall probability of selection irrespective of SEA size and served as the secondary sampling units.
Within each selected SEA, 11 interview households were randomly selected to receive water quality testing of stored household water (i.e., water stored in a jerry can, bucket, or other container in the household). Following completion of the survey, an ~120 ml water sample was aseptically collected into a sterile plastic sample bag containing sodium thiosulfate. Another sample was collected for free chlorine residual (FCR) testing on site. Sample bags were transported on ice to a local laboratory for same-day analysis. Membrane filtration was used to enumerate Escherichia coli (E. coli), a bacterial indicator of fecal contamination.
Study population
Study participants were residents ≥18 years old identified as the head of household or spouse of the head of household within the selected study PUAs. Written informed consent was obtained from all study participants. Participants answered questions regarding household demographics and WASH access and practices. They also answered questions pertaining to all individuals in their household, specifically illness (prevalence of diarrhea and influenza-like illness) and time spent collecting water. Households were deemed ineligible and replaced if one of the following scenarios occurred: a household was selected for an interview and a head of household or their spouse was not home after three visits; a head of household or their spouse did not consent to be interviewed; a head of household or their spouse were under the age of 18; a household had not been living in that structure for ≥2 months; a head of household or their spouse could only be found on Sunday or outside of field data collection hours. The questionnaire was written in English and translated into Nyanja and Bemba, the two most commonly spoken tribal languages in Lusaka.
Outcomes
The three health outcomes included in this study were waterborne illness at the household level categorized as any household member having experienced diarrhea or respiratory illness in the 7 days before interview (yes vs. no), diarrheal illness categorized as any household member having experienced diarrhea in the 7 days before interview (yes vs. no), and respiratory illness categorized as any household member having experienced respiratory or “flu-like” illness in the 7 days before interview (yes vs. no). In the questionnaire, diarrhea was defined as “three or more loose or watery stools in a 24-h period” and respiratory illness was defined as having a fever and a cough, a fever and a sore throat, or all three symptoms.
Statistical analyses
To examine the factors associated with the outcome variables (waterborne illness, diarrhea illness, and respiratory illness), we ran three multivariable logistic regressions, one model per each outcome. We investigated a number of demographic, socio-economic, and WASH factors based on a priori hypotheses of biologically or socioeconomically plausible risk or protective associations. Possible correlations from our three-level clustered data (i.e., households within a SEA, and SEAs within a PUA) were treated using Generalized Estimating Equations with compound symmetry correlation structure; the quasi information criterion was used to select the variable with the best model fit out of several correlated ones47.
The considered demographic factors in the models were gender of head of household, education level attained by head of household (primary or under, secondary, and tertiary), household size, and a household having any child <5 years old (yes vs. no). Home ownership (rent vs. own) and household expenditure (dichotomized at the third quartile) were included as a proxy for socioeconomic status; household expenditure as a proxy for income included measurements for food, rent, utilities, healthcare, and educational expenditure categories. For WASH practices, we considered the household water source, daily water consumption per person for all purposes (≤20 L/day, vs. >20), daily water availability (<7 h/day, 7-11, and >11), covers observed on water storage containers (some/none vs. all), stored water treatment (yes vs. no), self-reported handwashing with soap (yes vs. no), and heavy toilet sharing (≥18 people vs. <18 people). We used WHO/UNICEF Joint Monitoring Programme (JMP) definitions for dichotomizing the type of sanitation facilities and drinking water sources as either “Improved” or “Unimproved”. “Improved” drinking water sources, as per the JMP, were communal tap/water kiosk, protected well, piped water, and kiosk from another compound; “unimproved” drinking water sources included unprotected well, private borehole, surface water, and bottled water. “Improved” sanitation facilities, as per the JMP, were pit latrine with slab, ventilated improved pit latrine (VIP), and flush toilet, with “unimproved” being pit latrine without slab, bucket/chamber pot, no facilities/bushes/plastic bags.
In a second round of analyses, we subset the data to only those households that received water quality testing of household stored water. We then ran three multivariable logistic regression models identical to the models listed above but with the addition of two water quality parameters, FCR and E. coli. Per WHO guidelines, the FCR variable was dichotomized as ≥0.2 (sufficient FCR) vs. <0.2 mg/L and the E. coli variable was dichotomized as present (i.e., ≥1 colony forming unit [CFU] per 100 ml) vs. absent (i.e., <1 CFU per 100 ml).
Ethical review
The study received approval from the Biomedical Research Ethics Committee at the University of Zambia and was reviewed in accordance with CDC human research protection procedures and determined to be a non-research, program evaluation activity.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
United Nations. 2018 Revision of World Urbanization Prospects/Multimedia Library - United Nations Department of Economic and Social Affairs (2018). https://www.un.org/development/desa/publications/2018-revision-of-world-urbanization-prospects.html. Accessed on 16 Jul 2018
César Calderón, L. S. Infrastructure and economic development in sub-saharan Africa. J. Afr. Econ. 19, i13–i87 (2010).
WHO. Progress on Sanitation and drinking water 2013 update. World Health 1, 1–40 (2013).
WHO. JMP launch versi on July 12 2017. Progress on Drinking Water, Sanitation and Hygiene - 2017 Update and SDG Baselines. WHO Libr. Cat. Data (2017). https://doi.org/10.1007/s12686-011-9397-4.
Pham, N. D. et al. Risk factors for human infection with avian influenza A H5N1, Vietnam, 2004. Emerg. Infect. Dis. 12, 1841–1847 (2006).
Hennessy, T. W. et al. The relationship between in-home water service and the risk of respiratory tract, skin, and gastrointestinal tract infections among rural Alaska Natives. Am. J. Public Health 98, 2072–2078 (2008).
Luby, S. P. & Halder, A. K. Associations among handwashing indicators, wealth, and symptoms of childhood respiratory illness in urban Bangladesh. Trop. Med. Int. Heal 13, 835–844 (2008).
WHO. Global Health Observatory Repository. WHO (2018). http://apps.who.int/gho/data/node.main. Accessed on 16th Jul 2018
Checkley, W. et al. Effect of water and sanitation on childhood health in a poor Peruvian peri-urban community. Lancet 363, 112–118 (2004).
UN Habitat. World Cities Report 2016 - Urbanization and Development: Emerging Futures. International Journal (2016). https://doi.org/10.1016/S0264-2751(03)00010-6.
World Bank. World Bank Open Data (2018). https://data.worldbank.org/indicator. Accessed on 16 Jul 2018.
Zambia. 2010 Census of Population and Housing Preliminary Population Figures (2011).
2010 Census of Population and Housing Dataset (2010).
Millennium Challenge Corporation. Zambia Compact (2019). https://www.mcc.gov/where-we-work/program/zambia-compact.
Fuller, J. A., Clasen, T., Heijnen, M. & Eisenberg, J. N. S. Shared sanitation and the prevalence of diarrhea in young children: evidence from 51 countries, 2001 - 2011. Am. J. Trop. Med. Hyg. 91, 173–180 (2014).
Kelly K. et al. Sanitation and hygiene-specific risk factors for moderate-to-severe diarrhea in young children in the Global Enteric Multicenter Study, 2007–2011: case-control study. PLoS Med (2016). https://doi.org/10.1371/journal.pmed.1002010.
Adane, M., Mengistie, B., Kloos, H., Medhin, G. & Mulat, W. Sanitation facilities, hygienic conditions, and prevalence of acute diarrhea among under- five children in slums of Addis Ababa, Ethiopia: baseline survey of a longitudinal study. 1–18 (2017). https://doi.org/10.1371/journal.pone.0182783.
He, Z. & Bishwajit, G. Burden of common childhood diseases in relation to improved water, sanitation, and hygiene (WASH) among Nigerian children. Int. J. Environ. Res. Public Health (2018). https://doi.org/10.3390/ijerph15061241.
Bhavnani, D., Goldstick, J. E., Cevallos, W., Trueba, G. & Eisenberg, J. N. S. Impact of rainfall on diarrheal disease risk associated with unimproved water and sanitation. Am. J. Trop. Med. Hyg. 90, 705–711 (2014).
Hill, K. et al. The effect of water and sanitation on child health: evidence from the demographic and health surveys 1986–2007. Int. J. Epidemiol (2015). https://doi.org/10.1093/ije/dyr102.
Gauff Ingenieure. Lusaka Water Supply, Sanitation and Drainage (LWSSD) Project, Detailed Engineering Design, Tender Documents, Detailed ESIAs and ESMPs for Water Supply and Sanitation Projects, 90% Design Review Report - Water Supply (Vol. 1: Main Report) (2013).
Snilstveit, B., White, H., Fewtrell, L. & Waddington, H. Water, Sanitation And Hygiene Interventions To Combat Childhood Diarrhoea In Developing Countries Hugh Waddington, International Initiative for Impact Evaluation (3ie). About 3ie The International. Evaluation 119 (2009).
Barreto, M. L. et al. Effect of city-wide sanitation programme on reduction in rate of childhood diarrhoea in northeast Brazil: assessment by two cohort studies. Lancet 370, 1622–1628 (2007).
Kolahi, A. A., Rastegarpour, A. & Sohrabi, M. R. The impact of an urban sewerage system on childhood diarrhoea in Tehran, Iran: a concurrent control field trial. Trans. R. Soc. Trop. Med. Hyg. 103, 500–505 (2009).
United Nations. Sustainable Development Goal 6 Synthesis Report on Water and Sanitation (2018).
Shrestha, S. et al. Access to improved water and its relationship with diarrhoea in Kathmandu Valley, Nepal: a cross-sectional study. BMJ Open 3, 1–8 (2013).
Subiros, M., Brottet, E., Solet, J. L., Leguen, A. & Filleul, L. Health monitoring during water scarcity in Mayotte, France, 2017. BMC Public Health 19, 1–10 (2019).
Robb, K. et al. Assessment of fecal exposure pathways in low-income urban neighborhoods in Accra, Ghana: rationale, design, methods, and key findings of the sanipath study. Am. J. Trop. Med. Hyg. 97, 1020–1032 (2017).
Id, N. A. et al. Quantitative assessment of fecal contamination in multiple environmental sample types in urban communities in Dhaka, Bangladesh using SaniPath microbial approach. pp. 1–21 (2019).
Kaufmann, R. et al. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect. Dis. 5, 42–52 (2005).
Wolf, J. et al. Systematic review: assessing the impact of drinking water and sanitation on diarrhoeal disease in low- and middle-income settings: systematic review and meta-regression. Trop. Med. Int. Health 19, 928–942 (2014).
Esrey, S. A., Potash, J. B., Roberts, L. & Shiff, C. Effects of improved water supply and sanitation on ascariasis, diarrhoea, dracunculiasis, hookworm infection, schistosomiasis, and trachoma.Bull. World Health Organ. 69, 609–621 (1991).
Getachew, A. et al. Diarrhea prevalence and sociodemographic factors among under-five children in rural areas of North Gondar Zone, Northwest Ethiopia. Int. J. Pediatr. 2018, 6031594 (2018).
Okour, A., Al-ghazawi, Z. & Gharaibeh, M. Diarrhea among children and the household conditions in a low-income rural community in the Jordan valley. Jordan Med. J. 46, 108–117 (2012).
Chowdhury, F., Khan, I. A., Patel, S. & Siddiq, A. U. Diarrheal illness and healthcare seeking behavior among a population at high risk for diarrhea in Dhaka, Bangladesh. PLoS ONE (2015). https://doi.org/10.1371/journal.pone.0130105.
Null, C. et al. Articles Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: a cluster-randomised controlled trial. Lancet Glob. Health 6, e316–e329 (2018).
Humphrey, J. H. et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: a cluster-randomised trial. Lancet Glob. Health 7, 132–147 (2019).
Luby, S. P. et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob. Health 6, e302–e315 (2018).
Huda, T. M. N. et al. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Soc. Sci. Med. 75, 604–611 (2012).
Boisson, S. et al. Effect of household-based drinking water chlorination on diarrhoea among children under five in Orissa, India: a double-blind randomised placebo-controlled trial. PLoS Med. 10, 1001497 (2013).
Luby, S. P., Halder, A. K., Huda, T., Unicomb, L. & Johnston, R. B. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: an observational study. PLoS Med. 8, 1001052 (2011).
Feikin, D. R. et al. The burden of common infectious disease syndromes at the clinic and household level from population-based surveillance in rural and Urban Kenya. PLoS ONE 6, 1–10 (2011).
Omore, R. et al. Health care-seeking behavior during childhood diarrheal illness: Results of health care utilization and attitudes surveys of caretakers in Western Kenya, 2007-2010. Am. J. Trop. Med. Hyg. 89, 29–40 (2013).
Nasrin, D. et al. Health care seeking for childhood diarrhea in developing countries: evidence from seven sites in Africa and Asia. Am. J. Trop. Med. Hyg. 89, 3–12 (2013).
Breiman, R. F. et al. Population-based incidence of typhoid fever in an urban informal settlement and a rural area in Kenya: implications for typhoid vaccine use in Africa. PLoS ONE 7, 29119 (2012).
Njuguna, H. N. et al. Use of population-based surveillance to define the high incidence of shigellosis in an urban slum in Nairobi, Kenya. PLoS ONE 8, 1–9 (2013).
Pan, W. Akaike’s information criterion in generalized estimating equations. Biometrics (2001). https://doi.org/10.1111/j.0006-341X.2001.00120.x.
Acknowledgements
We acknowledge the support of the Zambian Ministry of Health, The Millennium Challenge Account Zambia, and all study participants. This research was financially supported by The Millennium Challenge Corporation and conducted in collaboration with NORC at the University of Chicago and RuralNet Associates Ltd., Lusaka, Zambia. We also thank Tracy Ayers, Ben Nygren, and Mike Hoekstra for their input and guidance during study and instrument design. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
J.M.B., M.I.M, E.C.-K., F.K.M., A.T.T., G.D., and J.L.M. designed the evaluation and data collection tools. S.C.H., M.B.S., B.B.A., W.M., L.C.C., and J.M.B. collected and managed the data. S.C.H., S.K., and S.J. performed the data analysis. S.C.H., S.K., and J.M.B. drafted the manuscript. All authors reviewed and provided comments on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hubbard, S.C., Meltzer, M.I., Kim, S. et al. Household illness and associated water and sanitation factors in peri-urban Lusaka, Zambia, 2016–2017. npj Clean Water 3, 26 (2020). https://doi.org/10.1038/s41545-020-0076-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41545-020-0076-4