Abstract
Australia has committed to the 17 Sustainable Development Goals (SDGs) goals under the UN’s 2030 Agenda. However, these goals may not be fully achieved in Australia under current policy settings. Australia reports success in achieving the goal for quality and access to safe drinking water and sanitation (SDG 6), though for Australians living in remote Indigenous communities, the experience is very different. Furthermore, the burden of disease is higher in remote communities (SDG 3). Many of these diseases are waterborne or hygiene-related, including prevalence in some remote Indigenous communities of endemic trachoma eye infection, preventable through access to functioning water services and available soap. This research provides a case for identifying, then understanding the interlinkages between SDGs 3, 6, and others locally, as well as nationally. This will enable governments to enact policies for long-term sustainable solutions for remotely-located and marginalised peoples in Australia in line with Agenda 2030 commitments.
Similar content being viewed by others
Introduction
The United Nation’s sustainable development agenda sets out a comprehensive vision for economic, social and environmental development, with health integral to sustainable social development, but deeply interconnected within the 17 Sustainable Development Goals (SDGs) that were endorsed in September 2015 for achievement by 20301. The SDGs are richly interlinked, and understanding these connections is important to maximise positive outcomes and minimise negative impacts2,3,4. A recent United Nations (UN) publication outlined the importance of coordination between different government agencies and levels to achieve the goals. It identified that ‘vertical integration efforts aim to create synergies and enhanced consistency across levels of government’ (p.x) but that there are ‘few examples of full and effective vertical integration across national, subnational and local levels for SDG implementation’ (p.xi)5.
Examples of the need for integration of goals are SDG 3 (‘Good health and well-being’) and SDG 6 (‘Clean water and sanitation’), underlining the extrapolation of ‘health’ described by the SDG targets to include both personal and environmental health. The extended SDG 3 description states: ‘a major risk factor for infectious diseases and mortality is the lack of safe water, sanitation and hygiene (WASH) services’6. This statement reinforces the connection to SDG 6. The health impact of unsafe water and the associated risk of contamination from unmanaged sewage is estimated to cause around sixty percent of deaths from diarrhoea globally7.
Focusing on Australia, the World Bank’s Development Indicators report that 100 percent of the population are using safely-managed drinking water and sanitation services8. However, WASH challenges such as poor drinking water quality, limited access to safely managed water, limited hygiene infrastructure and marginal living conditions have been identified as key factors contributing to risk of infection and disease transmission in remotely-located, discrete Indigenous communities9. Given that the UN agenda’s ambition is that ‘no one will be left behind’, it is crucial to determining what needs to be done for Australia to meet its commitments under Agenda 20301,10. Understanding the current access to water-related basic services for Indigenous Australians who live in geographically-remote locations and who are already noted to be socio-economically disadvantaged, and the rate of improvement in this, is key to this country-wide consideration.
Given this context, this research uses a case study in remote Australia to further clarify the intersection between SDGs 3 and 6, purposively exploring its complexity in order to provide a basis for integrated progress of the two goals simultaneously. The objective of this research was to clarify the intersection between SDGs 3 and 6, in order to provide a basis for integrated progress of the two goals simultaneously. These findings are likely to be of use to inform the policy–science interface around SDG implementation of both SDGs 3 and 6, and the broader 2030 sustainable development agenda, including for Indigenous Australians.
Australia is one of the 193 UN member countries that unanimously endorsed the SDGs. Unlike the preceding Millennium Development Goals, the SDGs apply to all countries and citizens—irrespective of the country’s level of development11,12. For Australia, this domestic—as well as regional—focus necessitates considering the development, health and environmental status of Australian issues (see ref. 13).
The 17 SDGs are explicated in detail by a total of 169 targets, and 232 indicators outline how to measure the progress of the goal1. For example, SDG 6 outlines the UN’s ambition for safe management of drinking water and faecal waste, and the attainment of hygiene1. Beyond SDG 6, water is explicitly mentioned in relation to SDG 3 (health impacts from water-borne diseases and contaminated water), SDG 11 (water-related disasters), SDG 12 (water pollution), and SDG 15 (conservation of freshwater ecosystems)1,14. This complex of linkages to SDG 6 speaks to the interlinkage of all SDGs that provides an integrated set of priorities with interdependent goals and targets4.
For example, the goal for health and well-being (SDG 3) is influenced by efforts to reduce poverty (SDG 1), knowledge of health behaviours (SDG 4) and their gendered differences (SDG5), clean water, sanitation and hygiene (SDG 6), safe and healthy living environments (SDG 11), and agricultural products (SDG 15)15. Yet currently the systemic links between the SDGs and associated targets are not explicit16, despite an acknowledgement within the UN that the SDGs should be considered through an integrated approach, noting that ‘sustainable development interventions cannot be put in an economic, social and/or environmental box’17.
Australia’s commitment to the SDGs arises from its support for the UNGA resolution of 25 September 2015 regarding the 2030 Agenda for Sustainable Development18. The 2030 Agenda is not an international treaty and does not create legal obligations; there is no binding obligation on any country or political leader to achieve SDG3 or SDG6 and no sanction for not doing so19. Nevertheless, the resolution includes significant processes to encourage political leaders to strive for the agreed results18. These include detailed goals and targets specifying objectives and use of the High Level Political Forum to provide peer review of implementation performance18, pp. 33–34).
While the targets have been agreed to be “aspirational and global”, with each government free to set national targets appropriate to its circumstances, the 232 agreed indicators for the SDGs are very clear to assist reporting and accountability.
SDG 6 was proposed to the UN as a specific goal in acknowledgement that access to clean, safely managed water, sanitation, and hygiene are key interventions for primary health prevention and could reduce the global disease burden by almost ten per cent20,21. This is likely to have a flow-on effect on educational attainment, public health costs, and economic productivity14, with WASH investments calculated as providing seven-to-one benefits to costs for health outcomes22. A recent analysis of interlinkages between a range of SDGs identified that improved water quality and access contributes directly to improved health, which is otherwise difficult to achieve4. That analysis noted that interaction between SDGs 3 and 6 is strongest in locations with prevalent waterborne and infectious diseases; it also noted poverty (SDG 1) as a structural factor that influences health4.
Australia’s commitment to Agenda 2030 is reflected in the Australian Government’s 2017 Foreign Policy White Paper23, which states that in working with partners to achieve the SDGs, Australia will use its overseas development assistance to catalyse sustained and inclusive economic growth to help reduce poverty23. Australia’s particular commitment to SDG6 and other water-relevant aspects of the 2030 Agenda was exemplified by the participation in the period 2016–2018 of the then Australian Prime Minister, the Honourable Malcolm Turnbull, in the UN High Level Panel on Water24, championing Panel initiatives on water data, water use efficiency and innovation in the water sector25.
The Panel’s final outcome document recommends, inter alia, that all countries ‘address gaps in service delivery models, technology and behaviour change which limit access to sustainable drinking water and sanitation for all—including the needs of women, girls, people with disabilities and communities in vulnerable situations, recognising access to water and sanitation services and a fundamental human right’. Since then, the United Nations has issued the World Water Development Report 2019 ‘Leaving No-one Behind’, which sets out clearly the key issues and challenges in achieving the universality objectives of Agenda 203026. These calls to the world require reflections on how well is Australia itself is addressing these gaps27.
Indigenous Australians living in remote communities provide a case study for the potential for SDG commitments to significantly improve current health and water status of some of the most disadvantaged members of Australian society. Health status is best described holistically through ‘social determinants’, a term coined by Marmot and Wilkinson28 to describe how the ‘the health of populations is related features of society and its social and economic organisation’ (p.xi). The complex social and environmental determinants of health and well-being inequalities between Indigenous and non-Indigenous Australians are widely documented, and are acknowledged as being particularly challenging in more remote and isolated communities29,30,31,32,33. One of the key indicators identified as a significant factor in Australian Aboriginal poor health is stress, created in part by ‘a burden of grief, guilt, anger, frustration and bitterness that many people carry’34, p. 3).
Indigenous Australians are significantly disadvantaged by the loss of connection to country and the limited infrastructure associated with the locations in remote areas that they reside. For example, Indigenous Australians are almost four times as likely to die with chronic kidney disease as a cause of death than non-Indigenous Australians35. The UN Special Rapporteur released a report in late 2017 on the rights of Indigenous Australians, noting inequalities in resources for remote service management of chronic diseases, and the importance of cultural connection for improving health indicators36. The need for continued action, focus and funding is reflected in the Government’s latest report on Closing the Gap (in Indigenous disadvantage). It stated that, in the past 10 years, ‘the lives of Aboriginal and Torres Strait Islander people have improved but more gains need to be made. It is clear that continued effort and action is required’37, p. 8).
Discrete, remote Australian Indigenous communities were selected as the case study focus, as these are often both geographically-isolated and economically-disadvantaged, two factors that can affect the quality of health and WASH services. Such communities are defined as permanently inhabited by a predominantly Indigenous population (Aboriginal and Torres Strait Islanders), where housing or infrastructure may be managed on a community basis38. Over the past decade, management of housing has changed to a diverse mix of institutional arrangements. A ‘remote’ or ‘very remote’ area is classified according to the Accessibility/Remoteness Index of Australia. Population data from 2011 calculated that the total population in Australian remote Indigenous communities (including those on island communities as well as the mainland) amounted to 116,58839.
Although investment in, and access to WASH services have improved in recent years in remote Indigenous communities in Australia, many residents continue to experience challenges with drinking water quality, inadequate and disrupted sanitation services, and associated health issues29. The latest Overcoming Indigenous Disadvantage review and report card identified that health outcomes for Indigenous communities—particularly those in remote and very remote locations—were compromised by a range of environmental health factors within homes and communities10. Concerns raised regarding the quality of infrastructure and services include whether health hardware in remote communities met equivalent standards in non-Indigenous communities10.
Results and discussion
The results and discussion are combined into a single section as the social determinants of health are critical in understanding the context of the results and the way in which many of the SDGs are affected. In taking this approach, the focus is on the social environment rather than more specific aspects of health services and behaviour that arise from the determinants40. When considering Indigenous health in Australia, social determinants describe the causal pathways of ill-health which can include poverty and inequality, and thus also includes access to essential services, including health services and water and sanitation services40.
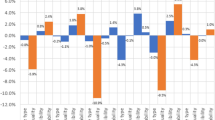
Statistics reflecting the current status of the total Australian and the Indigenous Australian populations are provided against the selected SDG 3 and 6 targets in Table 1. Where data exists, the status for individual and environmental health for Indigenous Australians living in remote communities is lower than the total Australian population, indicating that, at a disaggregated level, Australia has not yet delivered against the indicators for the SDG target. As the table displays, specific data was unable to be located for all indicators at a national level, with many gaps even in the SDG progress datasheets of the 2017 UN ESCAP Yearbook11. It is noted that some relevant data does exist at a sub-national level, but is reported in an aggregate format for national statistics. While the data is reported in the sections below, in addition to the table, the descriptive case study data was provided in lieu of detailed data at a sub-national level. The section numbers relate to the targets and indicators beneath the two goals in focus: SDG3 (health) and SDG 6 (water).
SDG 3: health
Only targets under SDG 3 with a direct linkage to water-borne diseases and safe water and sanitation are examined, using the indicator numbers for the targets.
Under-5 mortality rate
The health gap between Indigenous and non-Indigenous Australians is illustrated by the life expectancy at birth, which has been reported as up to 11.5 years less than the national average30. For those children aged under 5 years old, the Australian rate of deaths per thousand live births was 3.8 in 201611,41. However, data that specifically considers Indigenous Australians were 6.2 deaths per thousand live births for the same year42. This discrepancy, often referred to as the ‘gap’ of Indigenous disadvantage, does reflect an historical improvement for Indigenous child deaths, from 13.5 deaths per 1000 live births in 199843. This change has been attributed in part to improved access to antenatal care, reduced rates of smoking during pregnancy that have reduced low birthweight babies and child immunisation43. These data are drawn from the annual ‘Closing the Gap’ report, published by the Australian Government against set criteria within an agreed framework to address Indigenous disadvantage37. The annual publication and commitment to specifically address an Australian population with significant overall health burden provides a precedent or exemplar for possible national SDG reporting.
Number of people requiring interventions against neglected tropical diseases
The World Health Organisation lists 20 ‘neglected tropical diseases’, which are prevalent in tropical and subtropical climates and often among populations living in poverty, with limited sanitation and hygiene management- which is often the method for disease transmission44. Of these diseases, at least three are prevalent in remote Indigenous communities in Australia:
-
Scabies is a hygiene-related disease caused by a human itch mite infestation of the skin, usually spread by skin-to-skin contact45. Early, repeated infections can be linked to vulnerability to chronic diseases in later life. Recurrent infections by Group A streptococcus (GAS) of traumatised skin after scabies can also lead to acute rheumatic fever (ARF) and to post-streptococcal glomerulonephritis (PSGN)46,47,48,49. This association is significant as PSGN and rheumatic fever can lead to chronic kidney disease (CKD)50 and rheumatic heart disease51 respectively. Remote Indigenous communities of northern Australia have the highest rates of scabies globally, with hyper-endemic rates in many remote communities52. A key contributor to scabies and other skin infections in remote Indigenous populations has been noted to be residential over-crowding, and related infections with Staphylococcus aureus and Streptococcus pneumoniae have been specifically linked to direct contact transmission exacerbated by levels of crowding in remote and very remote communities48,53,54,55,56,57,58,59.
-
Soil-transmitted helminthiases (STH) infection risk factors involve those living in poverty and the associated lack of access to clean water and toilets, which contribute to unhygienic practices. In Australia, STH are only of concern where they are endemic in some Indigenous communities, particularly Strongyloides stercoralis in Queensland, Northern Territory, Western Australia, and New South Wales60. The worm can contribute to mortality and morbidity, particularly in immune-suppressed patients, but the cycle of infection is effectively disrupted by the introduction of sewerage systems60.
-
Trachoma eye infection remains in some of Australia’s Indigenous communities, the only developed country where it has not been eradicated61. Infection is correlated with a range of WASH-related factors including irregular washing, limited access to clean water and crowded housing62. It is caused by a bacterium that inflames the eye, and recurrent infections cause scarring of the eye and structural changes to the eyelid that can result in blindness62. Earlier research described how trachoma infections were sometimes viewed by remote community residents as normal, due to long-term familiarity with the symptoms. In other cases it was seen as a lower priority to more acute diseases such as skin infections, which presented a challenge to preventive and curative measures. The presence of both trachoma and skin infections are indicative of the ongoing need to provide sustainable washing facilities (‘environmental improvements’, within the WHO strategy)63,64.
Mortality rate attributed to unsafe water, unsafe sanitation and lack of hygiene (exposure to unsafe Water, Sanitation and Hygiene for All (WASH) services)
Residents of remote Australian communities, especially Indigenous Australians, continue to experience chronic and hygiene-related diseases at rates higher than the wider Australian population30,65. Water contamination has been proposed as one of the causes for this higher disease burden. Studies have found that drinking water supplies can be contaminated by microbes or naturally-occurring chemical and wastewater treatment can be poorly maintained with irregular monitoring66. For example, the WA Auditor-General’s 2015 report found many WA Indigenous communities had nitrate levels in their groundwater-sourced drinking water that were above the safe level for bottle-fed babies67. Another study found that over half of remote communities rated their housing as unsafe or unhealthy, due to environmental risks from dust, water, and sanitation68. An analysis of paediatric presentations over 10 years at the main hospital of the Northern territory, Royal Darwin Hospital (2004–2013), found gastroenteritis and other viral infectious to be the most common causes, with a disproportionate rate of presentation and admission among Indigenous children69. Pre-existing multiple morbidity in Aboriginal populations causes a disproportionately increasing incidence of Melioidosis, a soil-based bacterial infection associated with tropical flood waters, and a potential mortality rate of forty percent70.
SDG 6: water and sanitation
Proportion of population using safely managed drinking water services
National data for drinking water quality indicates that 99% of Australians in urban areas use ‘improved’ water, although the water quality data for overall rural and remote-living Australians are not available71. The literature provides documentation that the provision and maintenance of consistently sufficient and safe water to small communities in remote locations is an ongoing challenge for public utilities, local governments, and other agencies responsible for this provision63,72.
The detailed data available describe water quality for specific Indigenous communities, not the population. Although community-level data is not comparable to population-level data, the data do highlight significant contamination in direct contrast to the high level of safe drinking water in urban areas. For example, data regarding the 274 remote Indigenous communities in Western Australia indicated that the quality of drinking water supplied to some communities did not meet Australian standards approximately 30% of the time73. Further, E. coli and/or Naegleria microbes were detected in at least one community each month over a two-year monitoring period, indicating faecal contamination of the drinking water33,73. The microbial water-borne disease, Cryptosporidiosis, was found to be disproportionately high in remote Indigenous communities, compared to the non-Indigenous urban population in Western Australia74. Other enteric pathogens identified in contaminated water in remote Indigenous communities include Salmonella, Shigella, Campylobacter, E. coli and Rotavirus29. Furthermore, in the parts Northern Territory, Queensland and Western Australia where groundwater is the principal source of drinking and household water supply, some communities have been identified as exceeding Australian standards for nitrates and uranium73 (ABS38).
Proportion of population using safely managed sanitation services, including a hand-washing facility with soap and water
A significant impact on sanitation and hygiene in remote communities is domestic over-crowding. In 2014–15, 38% of the Indigenous adult population in remote areas and very remote areas were living in crowded conditions, almost three times the rate than in non-remote areas (13%)75. Compounding the effects of crowding, 28% were living in a dwelling in which one or more of the facilities for washing people, clothes and bedding, for safely removing waste, and/or for enabling the safe storage and cooking of food was not available or did not work75.
Regarding the ability to wash hands, faces and bodies with soap and water to prevent such infections as trachoma, very few households in Central Australian remote communities were found to possess soap on a regular basis30. These hygiene difficulties can be directly linked to crowding, which impacts on ‘health hardware’, the housing infrastructure that enables the washing of people and clothes, and enables safe preparation of food63,76. There can also be a high cost of washing supplies, when used by a large number of the house’s residents; this can be a challenge in addition to the cultural expectations of sharing assets among family members63.
Proportion of wastewater safely treated
National data indicates that that 74% of Australians use ‘safely managed’ sanitation facilities, defined as safe disposal of faecal material on or off site71. In 2006, the majority of remote Aboriginal communities relied on septic tanks as their main sewerage system, while a smaller number used pit toilets and a handful of communities did not have any organised sewerage system38. This has now changed following the implementation of state- and territory-funded programmes. The Council of Australian Governments’ (COAG) Strategy on Water and Wastewater Services in remote (including Indigenous) Communities has provided national funding for centralised water treatment infrastructure77. Despite the improvement of these wastewater services, there has been evidence of poor maintenance of wastewater treatment facilities. For example, a 2015 audit from Western Australia noted a high rate of communities that did not meet national standards—with reported drinking water contamination from sewage-derived E. coli or Naegleria sp. microbes at least once in 68 communities in the two-year period of reporting67.
It is also relevant to note that water and sanitation access are mentioned under basic health services described in SDG1 (indicator 1.4.1, ‘Proportion of population living in households with access to basic services’). Data indicates that the total Australian population is rated 8.8/10 (‘mature’) for health services access78. However, descriptive research identified that Indigenous and non-Indigenous Australians in remote areas often are disadvantaged in access to health services79.
Proportion of bodies of water with good ambient water quality
Specific inland water assessments indicate ‘very poor’ to ‘good’ results80. Recent years have improved or stabilised water quality, although the condition of water ecosystems was predominantly rated as poor and future improvements are challenged by reduced resources for monitoring and reporting80. There is no single national repository of data on surface-water quality, nor are there any regular national or state-scale assessments. Without such data, it is difficult to evaluate or critically analyse this indicator.
In conclusion, in remote Australian Indigenous communities the microbial contamination of drinking water remains a risk, and bore water may contain naturally high levels of chemical contaminants. Sanitation has improved with the increasing installation of centralised wastewater treatment replacing onsite septic tanks, yet concerns remain regarding contamination and poor maintenance. The status of hygiene and related health issues, such as trachoma eye infection, is the area of greatest need—especially as chronic infections in early childhood are often linked to vulnerability to other diseases in later life. Significant crowding limits the ability of individuals to maintain personal and environmental hygiene conditions that can negatively affect health.
These findings directly link personal and environmental health (SDG 3) to the status of drinking water, sewage and hygiene maintenance (SDG 6). When reading such results, it is informative to understand them through the approach of social determinants of health. Beyond these three SDGs, the remaining SDGs also provide important context that contributes to health. For example, SDG 1 (poverty) mentions how disadvantage can arise from limited access to basic services, SDG 8 (decent work) requires consideration of unemployment rates in remote communities that lack resources and industries, SDG 10 (equality) considers equality both within and between societies, and SDG 11 (cities) considers different aspects of sustainable and resilient communities.
Beyond understanding and acting on interlinkages, further research is required to ensure accurate data that reflects the complete and detailed status of each country’s progress against the SDGs. As shown by the JMP data presented in this research, the granularity of data from most sources is lacking. Given that high-income countries should be aiming for 100% compliance with SDG indicators, ensuring detailed data from an appropriately local-level sources is required. With Indigenous peoples estimated around 4% of the Australian population, and fewer again in remote communities, their health challenges are easily glossed over in the aggregate data. But if “no-one is to be left behind”, such specific data—which differs significantly from the other health-monitoring and water-monitoring regimes, must be provided in a format that is not lost in the reporting of the SDG indicators.
Despite the challenges, these interrelationships indicate that addressing the relevant SDGs in combination can more effectively progress the goals and targets. In this case study, identifying then understanding the interlinkages between SDG 3, 6, and others can enable development of long-term sustainable solutions for remotely-located and marginalised peoples in Australia and internationally.
Methods
The research team included two Aboriginal Australians, to ensure appropriate portrayal and communication of the results. The research employed a case study design to respond to this objective.
The case study approach involved three methods. Firstly, a literature and information review was conducted to understand the range of issues on which health interacts with water and sanitation. Secondly, and building on this initial review, the relevant SDG targets and their associated indicators for health (SDG 3) and WASH (SDG 6) were selected, drawn from the 13 targets within SDG 3 and 8 targets within SDG6. Targets were identified as relevant if there was current literature that described the relationships between health and water and sanitation. Finally, an analytical process of deliberation connected the data from the review to the SDG targets. This was undertaken by the authors through dialogue and debate drawn from the supporting literature.
Data availability
All data is available from public sources.
References
UN. Transforming our World: The 2030 Agenda for Sustainable Development. (United Nations, New York, 2015).
UN ESCAP. Integrated Approaches for Sustainable Development Goals Planning: The Case of Goal 6 on Water and Sanitation. (United Nations Economic and Social Commission of the Asia Pacific, Bangkok, 2017).
Hall, N. et al. Achieving the UN Sustainable Development Goals for Water and Beyond. (Global Change Institute, The University of Queensland, Brisbane, 2016).
ICSU. A Guide to SDG Interactions: From Science to Implementation. (International Council for Science (ICSU), Paris, 2017).
UN DESA. Working Together: Integration, Institutions and the Sustainable Development Goals- World Public Sector Report 2018. (Department of Economic and Social Affairs, United Nations, New York, 2018).
UN DESA. Sustainable Development Goal 3. (Division for Sustainable Development, Department of Economic and Social Affairs, United Nations, New York, 2017).
WHO. Preventing Diarrhoea through Better Water, Sanitation and Hygiene: Exposures and Impacts in Low- and Middle-Income Countries. (World Health Organisation, Geneva, 2014).
World Bank. World Development Indicators. (World Bank Group, Washington DC, 2014).
McDonald, E., Bailie, R., Grace, J. & Brewster, D. A case study of physical and social barriers to hygiene and child growth in remote Australian aboriginal communities. BMC Public Health. https://doi.org/10.1186/1471-2458-9-346 (2009).
Productivity Commission. Overcoming Indigenous Disadvantage: Key Indicators 2016 (Productivity Commission, Australian Government, Melbourne, 2016).
UNESCAP. Statistical Yearbook for Asia and the Pacific 2017: SDG Datasheet (Australia). (United Nations Economic and Social Commission of the Asia Pacific, Bangkok, 2018).
Watson, R., Thwaites, J., Griggs, D., Kestin, T. & McGrath, K. Sustainable Development Goals and Targets for Australia: An Interim Proposal. (Sustainable Development Solutions Network and Monash Sustainability Institute, Melbourne, 2014).
Hall, N. L. et al. Implementing the United Nations’ Sustainable Development Goals for water and beyond in Australia: A proposed systems approach. Australas. J. Water Resour. 22, 29–38 (2018).
Jenkins, M. Access to Water and Sanitation. POST note 521 (2016).
IFPRI. Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030. (International Food Policy Research Institute, Washington, DC, 2016).
Le Blanc, D. Towards Integration at Last? The Sustainable Development Goals as a Network of Targets: Working Paper No. 141. (United Nations Department of Economic and Social Affairs, Geneva, 2015).
UN ESCAP. Pacific Consultation on Progress on the Millennium Development Goals and the Post-2015 Development Agenda. (United Nations Economic and Social Commission for Asia and the Pacific, Bangkok, 2014).
UN. Transforming Our World: the 2030 Agenda for Sustainable Development (United Nations A/RES/70/1). (United Nations General Assembly, New York, 2015).
UN. The Sustainable Development Agenda. (Department of Public Information, United Nations, New York, 2016).
Cameron, C., Hunter, P., Jagals, P. & Pond, K. Valuing Water, Valuing Livelihoods: Guidance on Social Cost-benefit Analysis of Drinking-water Interventions, with special reference to Small Community Water Supplies. (International Water Association and World Health Organisation, 2011).
Prüss-Üstün, A., Bos, R., Gore, F. & Bartram, J. Safer Water, Better Health: Costs, Benefits and Sustainability of Interventions to Protect and Promote Health. (World Health Organization, Geneva, 2008).
OECD. OECD Environmental Outlook to 2050. (OECD Environment Directorate and the PBL Netherlands Environmental Assessment Agency, Paris, 2011).
Australian Government. 2017 Foreign Policy White Paper. (Australian Government, Canberra, 2017).
UN HLPW. Action Plan. (High Level Panel on Water, United Nations, New York, 2016).
UN. High Level Panel on Water webpage. (United Nations, New York, 2017).
UN Water. The United Nations World Water Development Report 2019: Leaving No One Behind. (United Nations Water, Geneva, 2019).
UN HLPW. Making Every Drop Count: An Agenda for Water Action. (United Nations’ High-Level Panel on Water, New York, 2018).
Marmot, M. & Wilkinson, R. (eds) Social Determinants of Health (Oxford University Press, New York, 1999).
Clifford, H., Pearson, G., Franklin, P., Walker, R. & Zosky, G. Environmental health challenges in remote Aboriginal Australian communities: clean air, clean water and safe housing. Aust. Indigenous Health Bull. 15, 1–13 (2015).
Foster, T. & Dance, B. Water-washed diseases and access to infrastructure in remote indigenous communities in the northern territory. Aust. Water Assoc. J. 39, 72–77 (2012).
McDonald, E., Bailie, R., Brewster, D. & Morris, P. Are hygiene and public health interventions likely to improve outcomes for Australian Aboriginal children living in remote communities? A systematic review of the literature. BMC Public Health 8, 1 (2008).
McDonald, E., Slavin, N., Bailie, R. & Schobben, X. No germs on me: A social marketing campaign to promote hand-washing with soap in remote Australian aboriginal communities. Glob. Health Promot. 18, 62–65 (2011).
Qld Health. The Health of Queenslanders 2016: Report of the Chief Health Officer. (Queensland Health, Brisbane, 2016).
Jeffries-Stokes, C., Stokes, A. & McDonald, L. Pulkurlkpa: the joy of research in aboriginal communities. J. Paediatr. Child Health. https://doi.org/10.1111/jpc.13008 (2015).
AIHW. Chronic Kidney Disease in Aboriginal and Torres Strait Islander people (Report PHE 151). (Australian Institute of Health and Welfare, Canberra, 2011).
UN GA. Report of the Special Rapporteur on the rights of indigenous peoples on her visit to Australia, Thirty-sixth session, 11-29 September, Agenda item 3. (United Nations General Assembly Human Rights Council, New York, 2017).
DPMC. Closing The Gap: Prime Minister’s Report 2018. (Department of the Prime Minister and Cabinet, Commonwealth of Australia, Canberra, 2018).
Housing and Infrastructure in Aboriginal and Torres Strait Islander Communities, Australia, 2006 [Internet]. (Australian Bureau of Statistics, 2007) Available from: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4710.0Main+Features22006?OpenDocument.
Census of Population and Housing: Characteristics of Aboriginal and Torres Strait Islander Australians, 2011 [Internet]. (Australian Bureau of Statistics, 2012). Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2076.0main+features1102011.
Saggers, S. & Gray, D. in Social Determinants of Indigenous Health (eds Carson, B. et al.) (Allen & Unwin, 2007).
The Lancet. Health-Related SDGs: Australia. (The Lancet, London, 2016).
DPMC. Aboriginal and Torres Strait Islander Health Performance Framework 2014 Report. (Department of Prime Minister and Cabinet- Indigenous Affairs Office, Canberra, 2014).
DPMC. Closing the Gap Prime Minister’s Report 2017. (Department of Prime Minister and Cabinet, Canberra, 2017).
WHO. Neglected Tropical Diseases. (World Health Organisation, Geneva, 2017).
CDC. Hygiene-related Diseases: Scabies. (Center for Disease Control and Prevention, Atlanta, 2009).
Remote Primary Health Care Manuals. Central Australian Rural Practitioners Association (CARPA) Standard Treatment Manual. 7th edn, (Centre for Remote Health, 2017).
Davey, R. X. & Tong, S. Y. C. The epidemiology of Staphylococcus aureus skin and soft tissue infection in the southern Barkly region of Australia’s Northern Territory in 2017. Pathology 51, 308–312 (2019).
Engelman, D. et al. Invasive Staphylococcus aureus infections in children in tropical northern Australia. J. Pediatr. Infect. Dis. Soc. 3, 304–311 (2014).
Marshall, C. S. et al. Acute post-streptococcal glomerulonephritis in the Northern Territory of Australia: a review of 16 years data and comparison with the literature. Am. J. Trop. Med. Hyg. 85, 703–710 (2011).
Garcia-Garcia, G., Agodoa, L. & Norris, K. C. Chronic Kidney Disease in Disadvantaged Populations. (Elsevier Science & Technology, 2017).
Kerdemelidis, M., Lennon, D., Arroll, B., Peat, B. & Jarman, J. The primary prevention of rheumatic fever. J. Paediatr. Child Health 46, 534–548 (2010).
Lokuge, B. et al. Crusted scabies in remote Australia, a new way forward: lessons and outcomes from the East Arnhem Scabies Control Program. Med J. Aust. 2014 200, 644–648 (2014).
Jacoby, S. P. et al. Crowding and other strong predictors of upper respiratory tract carriage of Otitis media-related bacteria in Australian aboriginal and non-aboriginal children. Pediatr. Infect. Dis. J. 30, 480–485 (2011).
Bailie, R., Stevens, M., McDonald, E., Brewster, D. & Guthridge, S. Exploring cross-sectional associations between common childhood illness, housing and social conditions in remote Australian aboriginal communities. BMC Public Health 10, 147–147 (2010).
Clucas, D. B. et al. Disease burden and health-care clinic attendances for young children in remote aboriginal communities of northern Australia. Bull. World Health Organ. 86, 275–281 (2008).
McDonald, E. & Bailie, R. Hygiene improvement: Essential to improving child health in remote Aboriginal communities. p. 491–496 (Blackwell Publishing Asia, Melbourne, Australia, 2010).
McDonald, E., Bailie, R., Grace, J. & Brewster, D. A case study of physical and social barriers to hygiene and child growth in remote Australian aboriginal communities. BMC Public Health 9, 346 (2009).
Price Waterhouse Coopers. Living in the sunburnt country: findings of the review of the community housing and infrastructure programme. (PWC, 2007).
Quinn, E. K., Massey, P. D. & Speare, R. Communicable diseases in rural and remote Australia: the need for improved understanding and action. Rural Remote Health 15, 3371 (2015).
Gordon, C., Kurscheid, J., Jones, M., Gray, D. & McManus, D. Soil-transmitted helminths in tropical Australia and Asia. Tropical Med. Infect. Dis. 2, 1–32 (2017).
Taylor, H., Lange, F. & Stanford, E. Why is trachoma blinding Aboriginal children when mainstream Australia eliminated it 100 years ago? The Conversation.com, Sep 14 (2016).
Warren, J. M. & Birrell, A. L. Trachoma in remote Indigenous Australia: a review and public health perspective. Aust. N.Z. J. Public Health 40, S48–S52 (2016).
Hall, N. et al. Water, Sanitation and Hygiene in Remote Indigenous Australia: A Scan of Priorities. (The University of Queensland and Wateraid Australia, Brisbane, 2017).
Andrews, R., Kearns, T., Connors, C., Parker, C. & Carville, K. A. Regional initiative to reduce skin infections amongst aboriginal children living in remote communities of the Northern Territory, Australia. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0000554 (2009).
Hall, N., Shannon, C. & Jagals, P. It’s a fallacy that all Australians have access to clean water, sanitation and hygiene. The Conversation.com, Sep 7 (2016).
Hall, N. L. Australian indigenous remote communities & water, sanitation & hygiene: a scan of needs. Water e-journal 3, 1–9 (2018).
WA, AG. Delivering Essential Services to Remote Aboriginal Communities (Western Australian Auditor General, Perth, 2015).
Melody, S. M. et al. A cross-sectional survey of environmental health in remote aboriginal communities in Western Australia. Int. J. Environ. Health Res. 26, 525–535 (2016).
Buntsma, D. et al. Patterns of paediatric emergency presentations to a tertiary referral centre in the Northern Territory. Emerg. Med. Australas. 29, 678–685 (2017).
Price, E. et al. Unprecedented melioidosis cases in Northern Australia caused by an Asian Burkholderia pseudomallei strain identified by using large-scale comparative genomics. Appl. Environ. Microbiol. 82, 954–963 (2015).
JMP. Progress on Drinking Water, Sanitation and Hygiene 2017: Update and SDG Baselines. (World Health Organisation and United Nations Children’s Fund, Geneva, 2017).
Milligan, B. et al. QWater Conference. (Australian Water Association, Brisbane, 2019).
OAG. Delivering Essential Services to Remote Aboriginal Communities. (Office of the Auditor General Western Australia, Perth, 2015).
Hublin, J., Combs, B., Reid, S. & Ryan, U. Differences in the occurrence of cryptosporidiosis in aboriginal and non-aboriginal people in Western Australia (2002–2012). Infect. Genet. Evolut. 53, 1001–1006 (2017).
National Aboriginal and Torres Strait Islander Social Survey, 2014–15 [Internet]. (Australian Bureau of Statistics, 2016) Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4714.0~2014-15~Main%20Features~Population%20context~2.
Pholeros, P., Rainow, S. & Torzillo, P. Housing for Health: Towards a Health Living Environment for Aboriginal Australia. (Healthabitat, Sydney, 1993).
DILGP. Capacity Building Program (2011–2014) Report: COAG Strategy on Water and Wastewater Services in Remote (including Indigenous) Communities - Queensland. (Queensland Department of Infrastructure, Local Government and Planning, Brisbane, 2015).
EIU. Access to Healthcare Database. (The Economist Intelligence Unit, New York, 2017).
AIHW. Australian Burden of Disease Study: Impact and Causes of Illness and Seath in Aboriginal and Torres Strait Islander People 2011. (Australian Institute of Health and Welfare, Canberra, 2016).
Cth Australia. State and Trends of Water Quality in Australia: State of the Environment. (Commonwealth of Australia: Canberra, 2016).
Acknowledgements
Thanks to our colleagues within the Australian water industry who engaged with earlier discussions of this topic to shape this resulting publication.
Author information
Authors and Affiliations
Contributions
N.L.H. and P.S.H. developed the article idea. N.L.H. lead the data collation and analysis with oversight from P.S.H. S.C. and W.A. provided expert input on discussion, consideration and portrayal of Indigenous Australians, drawing from both their personal identities as Aboriginal women and as professionals working in Indigenous rights. A.S. wrote the contextual information and N.L.H. oversaw the integration of discussion. All authors reviewed article drafts and approved the final manuscript, and N.L.H. submitted and corresponded on the article. All authors reviewed the peer reviewer comments, and N.L.H. led the revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hall, N.L., Creamer, S., Anders, W. et al. Water and health interlinkages of the sustainable development goals in remote Indigenous Australia. npj Clean Water 3, 10 (2020). https://doi.org/10.1038/s41545-020-0060-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41545-020-0060-z
This article is cited by
-
Benefits, costs and enabling conditions to achieve ‘water for all’ in rural and remote Australia
Nature Water (2024)
-
Potential benefits of public–private partnerships to improve the efficiency of urban wastewater treatment
npj Clean Water (2023)
-
Measuring the gaps in drinking water quality and policy across regional and remote Australia
npj Clean Water (2022)
-
BR-174 highway, geotourism and socio-environmental conflicts in the northern remote regions of the Amazon
GeoJournal (2022)
-
Exploring trade-offs between SDGs for Indus River Dolphin conservation and human water security in the regulated Beas River, India
Sustainability Science (2022)