Abstract
COVID-19 vaccines are effective and important to control the ongoing pandemic, but vaccine reactogenicity may contribute to poor uptake. Analgesics or antipyretic medications are often used to alleviate vaccine side effects, but their effect on immunogenicity remains uncertain. Few studies have assessed the effect of analgesics/antipyretics on vaccine immunogenicity and reactogenicity. Some studies revealed changes in certain immune response parameters post-vaccination when analgesics/antipyretics were used either prophylactically or therapeutically. Still, there is no evidence that these changes impact vaccine efficacy. Specific data on the impact of analgesic/antipyretic medications on immunogenicity of COVID-19 vaccines are limited. However, available data from clinical trials of licensed vaccines, along with recommendations from public health bodies around the world, should provide reassurance to both healthcare professionals and vaccine recipients that short-term use of analgesics/antipyretics at non-prescription doses is unlikely to affect vaccine-induced immunity.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has impacted global health and economies. Millions have died from this illness and many more have experienced reduced quality of life from COVID-19 ailment and the disease measures enforced to control virus transmission. Thus, the arrival of efficacious vaccines has been much welcomed.
To date, over 300 vaccine candidates have emerged, with more than 100 currently in clinical development and 17 deployed for emergency use in various countries around the world1,2. Among them, eight vaccines have currently been granted emergency use authorization by the World Health Organization (WHO), including messenger ribonucleic acid (mRNA), adenovirus vector-based, and inactivated virus vaccines2. Many other vaccines are at various stages of clinical development and consideration for emergency use authorization.
Within 6 months of the first COVID-19 vaccine approval3, over 2 billion doses of vaccines have been administered worldwide4. Despite this unprecedented pace in vaccine rollout, many more individuals need to be vaccinated and boosted before the necessary beneficial epidemiological impact of vaccination can be achieved and sustained globally. As vaccine supply increases, greater willingness to be vaccinated will also be required to increase uptake. One reason for vaccine hesitancy is the concern for vaccine-associated side effects5, including pain at the injection site, headache, myalgia, fever, and fatigue, although they are usually transient. Thus, therapeutic use of medication to reduce the rate and/or severity of vaccine-induced side effects, without impacting vaccine immunogenicity and efficacy, may be helpful in countering such hesitancy and improving vaccine and booster uptake rates.
Analgesics and antipyretics, such as acetaminophen (paracetamol) and non-steroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen), have been routinely used for decades to manage acute side effects, or reactogenicity, following vaccination. However, some have speculated that the use of antipyretics/analgesics to manage reactogenicity may impact vaccine efficacy. As booster vaccinations will eventually be needed to sustain vaccine effectiveness, there is an urgent need to determine whether the use of over-the-counter analgesics/antipyretics has any negative impact on vaccine immunogenicity and efficacy. Furthermore, it is important to determine whether vaccine immunogenicity and reactogenicity following the use of these medications vary by age group.
This article summarizes the evidence on the use of analgesic/antipyretic medications to relieve side effects following vaccination. It describes both the clinical and molecular bases of how such medications can minimize side effects without compromising vaccine immunogenicity and efficacy. Finally, it discusses the implications of such interventions for the global vaccination efforts against COVID-19.
Background on immunogenicity and reactogenicity of vaccines
Immune responses and the effectiveness of vaccines differ throughout life. At birth, the child’s immune system is considered ‘immature’, and maternal antibodies transferred trans-placentally and by breast feeding can interfere with vaccination. Consequently, many childhood vaccines are administered after several months of age, when the immune system has matured and maternal antibodies have waned. However, even in the absence of maternal antibodies, increasing age has been associated with better vaccine efficacy. Indeed, dengue vaccination in younger children between the ages of 2 and 6 years old showed lower vaccine efficacy than older children, even though both groups were immunologically naïve to dengue at baseline6,7. The effectiveness of measles vaccination between 12 and 18 months of age is another good example of this phenomenon8. With aging, the thymus involutes and naïve T cell production declines which, together with other age-related changes, leads to immunosenescence9. Comorbidities can also impact immune responses and affect vaccine efficacy in the elderly10. Thus, immunological findings from different vaccine studies may not be broadly applicable across all age groups.
Vaccines contain viral antigens or viral genes for translation into antigens, preferably in antigen-presenting cells upon inoculation, to induce specific immune responses and memory to protect against the corresponding pathogen and associated disease11. Vaccination first induces the innate immune response, which includes phagocytosis, release of chemokines and cytokines, complement activation, and cellular recruitment11. These innate immune responses play fundamental roles in programming subsequent adaptive immune responses12 and are thus required for the development of acquired immunity13. Among the cells in the innate immune system are antigen-presenting cells, such as dendritic cells12,14, which are essential in linking between the innate and adaptive immune systems. These cells interact with T and B cells to trigger the long-lasting adaptive responses12,15.
As the innate immune response is key to induce adaptive immunity, it has been widely assumed that vaccine-associated side effects are correlated with immunogenicity. However, findings from recent studies with the live attenuated yellow fever vaccine suggest that this assumption is not applicable for all vaccines. Studies on yellow fever vaccine have shown that individuals who developed side effects had higher levels of endoplasmic reticulum (ER) stress response genes expressed in the blood at baseline, likely in lymphocytes, as well as lower level of tricarboxylic acid cycle activity, likely in the monocytes16. As vaccination induces protein expression, the ER stress would be worsened and further complicated by increased energy demand, resulting in maladaptive ER stress response and pro-inflammatory response. This early pro-inflammatory response is directly correlated with the development of side effects, such as headache, myalgia, and fever11,16. In contrast, the innate immune response that correlates with adaptive immunogenicity develops from 3 to 7 days post-vaccination, with type-I interferon responses featuring more prominently than pro-inflammation17,18. Indeed, Chan et al.16 found no difference in neutralizing antibody levels against the yellow fever virus between participants who developed side effects and those who did not. Thus, there could be qualitative and temporal differences in the innate immune response that are involved in the development of side effects versus those that shape adaptive immunity. However, the yellow fever vaccine is a live attenuated virus; the separation between the innate immune responses that drive side effect manifestation and adaptive immune responses may be less distinct in other forms of vaccines. Hence, whether side effects can be minimized by analgesics and antipyretics without compromising adaptive immune responses will still need to be gleaned from clinical observations.
Effect of analgesic and antipyretic medicines on immune responses to vaccination
Although analgesics and antipyretics are not indicated for prophylactic use, they can be administered at the time of vaccination to prevent side effects or therapeutically following side-effect onset. A limited number of studies have evaluated the effect of analgesics/antipyretics on immunogenicity11,19,20,21,22. However, these studies have been limited to either specific age groups of the population or specific vaccines. As COVID-19 vaccination is being applied universally and eventually to all age groups, we undertook a more expansive review of the literature on acetaminophen and NSAIDs and their effects on vaccination.
Acetaminophen (Paracetamol)
Despite its widespread use for many years, the mechanism(s) of action of acetaminophen remain(s) unclear. The drug may exert its therapeutic effects through inhibition of cyclo-oxygenase (COX)-1 and −2 and the subsequent decrease of prostaglandin synthesis23, although other mechanisms have been suggested. Both COX-2 activation and prostaglandin production are important in innate immune response signaling23. Activated T and B cells express COX-2 and produce prostaglandins24. A small number of randomized controlled trials with several different vaccines have investigated the effects of prophylactic or therapeutic acetaminophen on vaccine responses in pediatric25,26,27,28 and adult populations29, with conflicting results (Table 1).
In a non-inferiority study investigating the use of prophylactic acetaminophen on vaccine immunogenicity, Falup-Pecurariu et al.25 observed a statistically non-significant trend for reduced antibody titers when prophylactic acetaminophen was given to infants immediately or several hours after the first dose of pneumococcal non-typable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) co-administered with diphtheria-tetanus-acellular pertussis-hepatitis B recombinant-inactivated poliomyelitis-adsorbed conjugated Haemophilus influenzae type b vaccine (DTaP-HBV-IPV/Hib) and diphtheria-tetanus-acellular pertussis-inactivated poliomyelitis-adsorbed conjugated Haemophilus influenzae type b vaccine (DTaP-IPV/Hib), compared with infants who did not receive prophylactic acetaminophen. This trend was not, however, seen after a booster dose25. Similarly, in children receiving PHiD-CV co-administered with DTaP-HBV-IPV/Hib and oral human rotavirus vaccines, prophylactic acetaminophen given immediately after vaccination (three doses at 6–8 h intervals) was associated with lower antibody titers but not lower seroconversion rates compared with those not receiving acetaminophen. The impact was less marked following booster vaccination26. However, this effect did not impact subsequent induction of immunological memory27.
Data from infants given the diphtheria-tetanus-whole cell pertussis-hepatitis B recombinant-inactivated poliomyelitis-adsorbed conjugated Haemophilus influenzae type b (DTwP-HBV-Hib) combination vaccine found that immune responses were similar regardless of whether acetaminophen was used prophylactically, therapeutically, or not at all28.
The impact of acetaminophen prophylaxis on vaccine immunogenicity may be antigen-specific30. Among infants who received repeat doses of the 13-valent pneumococcal conjugate (PCV13) and combined DTaP-HBV-IPV/Hib vaccines, antibody titers for five of 13 pneumococcal serotypes were significantly lower at 5 months of age among participants given prophylactic acetaminophen than among those who did not receive acetaminophen30. No difference in antibody titer was observed after booster doses at 13 months of age.
There may also be age-specific effects on acetaminophen prophylaxis and immunogenicity. A randomized, double-blind, placebo-controlled study in 474 Canadian healthcare workers found that acetaminophen given immediately after influenza vaccine administration (four doses at 4-h intervals) did not affect antibody responses29.
In summary, research on the effect of acetaminophen on vaccine immunogenicity is limited and does not establish clear evidence against the use of acetaminophen as a treatment for vaccine-induced side effects. Although the clinical significance of prophylactic acetaminophen use on antibody level is not known, some data suggest that the use of therapeutic acetaminophen may be preferred over prophylactic use to avoid any potential impact on immunogenicity.
NSAIDS
NSAIDs, most commonly ibuprofen at non-prescription doses, are also often used to manage post-vaccination side effects. The therapeutic effects of NSAIDs are the result of the inhibition of well-defined inflammatory pathways involving prostaglandin synthesis and COX-1 and COX-2 activities. Investigations into the impact of NSAIDs on vaccine immunogenicity have been mostly conducted in children and have led to varying conclusions (Table 1).
Neither immediate nor delayed prophylactic ibuprofen use had an impact on the immune responses to primary or booster vaccination in infants receiving the PHiD-CV vaccine21. Similarly, children receiving the inactivated influenza vaccine did not generate lower immune responses if they had received prophylactic ibuprofen, compared with those not receiving ibuprofen20,31.
In another study by Wysocki et al.30, infants who were given ibuprofen prophylaxis with repeat doses of PCV13 and combined DTaP-HBV-IPV/Hib vaccines had significantly reduced antibody responses to Bordetella pertussis filamentous hemagglutinin and the tetanus toxin, but not to pneumococcal antigens30.
Early investigations among a small number of older patients indicated that NSAID use is unlikely to impact vaccine responses32. More recently, an analysis of patients aged ≥65 years receiving a trivalent inactivated influenza vaccine reported altered antibody production, B cell phenotypic changes, alteration in immune cell proportions, and transcriptome-wide modifications in those receiving long-term NSAID33. However, there was no statistically significant difference in antibody titers between NSAIDs users and non-NSAIDs users. A meta-analysis of four clinical studies on long-term aspirin use in older adults (n = 1,597) also found no difference in antibody titers following influenza vaccination34.
In summary, while some studies have demonstrated a potential impact of ibuprofen prophylaxis on post-vaccination antibody production in children, studies in older adults found no significant impact. The observed changes in antibody titers appear to have little or no clinical impact, since the tested vaccines were effective.
Reactogenicity of current COVID-19 vaccines
The urgent need for COVID-19 vaccines posed an unprecedented dilemma—the need to expedite preclinical and clinical development of vaccines (some of which were based on relatively novel technologies) without jeopardizing safety and efficacy evaluation. Table 2 summarizes available reactogenicity data for the COVID-19 vaccines currently approved for emergency use.
mRNA-based vaccines
BNT162b2 (Pfizer-BioNTech) is a lipid nanoparticle-formulated, nucleoside-modified RNA vaccine encoding the full-length spike protein35,36. Among 8,183 vaccine recipients included in a reactogenicity subset of a Phase 2/3 study, injection-site pain was the most commonly reported local side effect, affecting 78–83% of recipients after the first dose and 66–71% after the second dose (Table 2)37. The most commonly reported systemic symptoms were fatigue (34–59%) and headache (39–52%), which generally occurred 1–2 days after vaccination. Both injection-site pain and systemic events were more commonly reported by younger than older recipients, and systemic events were observed more commonly after the second dose than after the first. Vaccine efficacy did not appear to be significantly affected by age in this Phase 2/3 trial37. Hwang et al. assessed the association between local and systemic reactogenicity and humoral immunogenicity following administration of BNT162b2 vaccine to healthy volunteers (n = 93)38. Association was evaluated using multivariate linear regression with adjustment for age, sex, and use of antipyretics. The study found that grades of local and systemic adverse events were not significantly associated with anti-S1 immunoglobulin G levels, suggesting no direct correlation between these adverse events and humoral immunogenicity.
The possibility that inflammatory response to mRNA vaccination underpins adverse events also raises the possibility that those with inflammatory conditions could have more or accentuated side effects. However, a study by Furer and colleagues did not find any significant difference in the rate or severity of side effects from BNT162b2 vaccination between those with autoimmune inflammatory rheumatic diseases compared to healthy controls39. However, it should be noted that most of the subjects with autoimmune conditions in this study were also on immunosuppressive therapy at the time of vaccination. Immunogenicity was impaired in those treated with rituximab, glucocorticoids and other immunosuppressive therapies that act on lymphocytes rather than the more widely used antipyretics/analgesics.
mRNA-1273 (Moderna) is a lipid-nanoparticle encapsulated mRNA vaccine, which expresses the pre-fusion-stabilized spike glycoprotein40,41. Similar reactogenicity to BNT162b2 has been reported for mRNA-1273 in both a Phase 1 study42 and a Phase 3 trial with 30,420 vaccine recipients43. In the Phase 3 trial, injection-site pain occurred in 83.7% of vaccine recipients after the first dose and 88.2% after the second dose (Table 2). Injection-site reactions were mostly mild-to-moderate in severity (grade ≤2) and lasted for a mean of 2.6 and 3.2 days after the first and second doses, respectively. Solicited systemic side effects also occurred more frequently after the second dose (79.4%) than after the first (54.9%), with fatigue and headache most commonly reported after both the first and the second dose and events more severe after the second dose than after the first. Both solicited local and systemic side effects were more common among younger (18 to <65 years of age) than older participants (≥65 years of age). However, studies on the safety of vaccination and immunogenicity in the elderly have largely excluded those who are frail with poorly controlled co-morbidities44. Ironically, this population is at high risk of severe COVID-19. These are important gaps in knowledge that need to be addressed urgently.
In summary, the reactogenicity (both local and systemic) associated with mRNA-based vaccines observed in clinical trials is notably higher than that seen with most non-COVID vaccines, which may have a negative effect on second dose compliance.
Adenovirus vector-based vaccines (OXFORD/ASTRAZENECA [AZ], SERUM INSTITUTE OF INDIA, SKBIO, JANSSEN/Johnson & Johnson [J&J])
AZD1222 (Oxford/AZ) is a replication-defective chimpanzee adenovirus-vectored vaccine expressing the full-length SARS-CoV-2 spike glycoprotein gene45. AZD1222 is also registered separately for a vaccine produced by the Serum Institute of India46 and by SKBio in South Korea.
In the randomized controlled Phase 2 component of a Phase 2/3 trial of AZD1222 (n = 420), the most common solicited local side effects after the first dose of the standard-dose vaccine were injection-site pain (in 61% of patients aged 18–55, 43% aged 56–69, and 20% aged ≥70) and tenderness (in 76%, 67%, and 49% of patients in the respective age groups)47. The most common solicited systemic side effects across the respective age groups after the first dose of the standard-dose vaccine were fatigue, headache, feverishness, and myalgia47. Local and systemic side effects were reported more commonly by younger than by older recipients and more commonly after the first dose than after the second (Table 2). No severe local side effects were reported, and the severity of systemic side effects was lower after the second than after the first dose. No reactogenicity differences between males and females were reported. The study by Hwang et al. (2021) had also included healthy adults (n = 42) who were vaccinated with AZD122238. Results were similar to those for recipients of the BNT162b2 mRNA vaccine, with no indication of an association between either local or systemic reactogenicity and humoral immunogenicity.
Ad26.COV2.S (Janssen/J&J) is a recombinant, replication-incompetent human adenovirus type 26 (Ad26) vector encoding a full-length, membrane-bound SARS-CoV-2 spike protein in a prefusion-stabilized conformation48,49. Ad26.COV2.S is administered as a single dose, differentiating it from the other vaccines considered here. In a Phase 3 trial (n = 44,325), the reactogenicity of the vaccine was reported to be generally mild-to-moderate and transient50. The most common local side effect was injection-site pain (48.6%). The most common systemic side effects were headache (38.9%) and fatigue (38.2%) (Table 2). Incidence rates for both local and systemic side effects were higher among individuals aged 18–59 years than among those aged ≥60, and antipyretic use was more frequent in younger than in older vaccine recipients.
Inactivated Virus Vaccines (SINOPHARM, SINOVAC BIOTECH)
BBIBP-CorV (Sinopharm) is a beta-propiolactone-inactivated SARS-CoV-2 vaccine developed in China and is produced in African green monkey kidney cells (Vero cells) that have been inoculated with SARS-CoV-2 (HB02 strain)51. In a Phase 2 study with 448 adults, the most common local side effect after first and second vaccinations was injection-site pain (16%)52. The most common systemic side effects were fatigue (3%) and fever (2%). Reactogenicity of the vaccine was generally mild-to-moderate. However, data in the elderly population are limited, as the study only enrolled patients aged 18–59 years.
CoronaVac (Sinovac Biotech) is a formalin-inactivated SARS-CoV-2 vaccine available for emergency use and was also developed in China. It is produced in Vero cells that have been inoculated with SARS-CoV-2 (CN02 strain). Data from Phase 1/2 studies in adults aged 18–59 years53 and ≥60 years54 indicated mild reactogenicity after vaccination. In younger vaccine recipients (Phase 2 data)53, injection-site pain was the most commonly reported side effect, occurring in 21–26% of recipients after both doses when administered 2 weeks apart and in 10–11% when the dosing interval was increased to 4 weeks. Fatigue and headache were the most common systemic side effects (Table 2). The incidence of all side effects was lowest after the second dose. Most were mild and resolved within 48 h. An indirect comparison with data from older recipients54 indicated a lower incidence of local and systemic side effects in the older population (Table 2).
Third (BOOSTER) dose of COVID-19 vaccines
Several countries have now begun to administer a third or booster dose several months after completion of the primary two-dose vaccination. Early data from studies that have explored the benefit of booster vaccination suggest that the safety profile of the booster dose is comparable across the different vaccines, regardless of what vaccine was used for the primary vaccination series55. This study, however, did not include the inactivated vaccines.
Effect of analgesic and antipyretic medicines on immune responses to COVID-19 vaccination
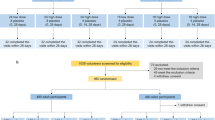
Only one study has specifically addressed the effect of the analgesic and antipyretic medication on the immunogenicity and reactogenicity of COVID-19 vaccines56. However, in most of the other COVID-19 vaccine trials, participants were allowed to use analgesics and antipyretics to treat post-vaccination symptoms. Where available, data from these studies offer some insight into the potential impact of these medicines on immune responses to COVID-19 vaccines (Table 3).
Phase 2/3 data on BNT162b2 (Pfizer-BioNTech) showed that younger vaccine recipients were more likely to use antipyretic or pain medication than older recipients and both age groups were more likely to use these medications following vaccination with BNT162b2 than placebo (Table 3)37. Vaccine efficacy against confirmed COVID-19 was 95.0% for onset at ≥7 days after the second vaccination with similar efficacy (generally 90–100%) observed across subgroups defined by age, sex, race, ethnicity, baseline body mass index, and the presence of coexisting conditions37. In the Phase 1 part of the trial, analgesic/antipyretic use was reported more frequently with increasing dose and number of doses57.
In two of five trial sites participating in a Phase 1/2 study of AZD1222 (Oxford/AZ), a protocol amendment permitted prophylactic acetaminophen prior to vaccination56. Vaccine reactogenicity (both local and systemic side effects) was generally reduced in recipients of prophylactic acetaminophen compared with those who did not receive acetaminophen (Table 3). Adjusted analysis of the effect of prophylactic acetaminophen in the first 2 days after vaccination on side effects of any severity demonstrated significant reductions in pain (odds ratio [OR] 0.41), feeling feverish (OR 0.47), chills (OR 0.28), muscle ache (OR 0.51), headache (OR 0.47), and malaise (OR 0.53; all p < 0.05). Immunogenicity was not affected.
Data from the Phase 3 study of Ad26.COV2.S (Janssen/J&J) also showed that younger vaccine recipients were more likely to use antipyretic or pain medication than older recipients (Table 3)50,58. Vaccine efficacy against severe–critical COVID-19 was 76.7% for onset at ≥14 days and 85.4% for onset at ≥28 days post-vaccination and was considered similar in participants aged ≥60 years and the overall study population, irrespective of sex, race, or ethnicity.
To date, there are no published data on the use of analgesic/antipyretic medication with mRNA-1273 (Moderna), BBIBP-CorV (Sinopharm), or Coronavac (Sinovac Biotech) vaccines.
Clinical implications/summary
Analgesic and antipyretic medications have been used for decades to manage side effects caused by different types of vaccines in pediatric and adult populations, including the elderly. It is important to distinguish between changes in immune responses and clinical impact, such as vaccine efficacy. While some changes in immune responses (primarily with polysaccharide vaccines) may result from the use of these medications, there is no evidence that their use to manage side effects has any clinically meaningful impact on vaccine efficacy. In fact, it is unlikely that, based on the evidence available in the literature, the short-term use of analgesics/antipyretics at over-the-counter doses suppresses the clinical impact of vaccine-induced immune responses. However, it should also be noted that all of the studies examining the effect of analgesics/antipyretics on immunogenicity have focused exclusively on humoral responses. To our knowledge, none has systematically examined the impact of analgesics/antipyretics on cellular immune responses. Eliciting cellular immunity from COVID-19 vaccination is of particular importance since T cells play a major role in protection against severe and even symptomatic infection59,60.
An aspect that remains unknown is how effective analgesics/antipyretics would be in preventing rare but serious adverse events such as myocarditis/pericarditis and thrombosis61,62,63,64. As inflammation, at least in part, contributes to these serious adverse events65,66, anti-inflammatory treatments should also reduce the risk of such rare events. A global collaborative effort will be needed if we are to test prophylactic approaches to prevent such rare but serious events.
Available data from studies of vaccines currently approved for emergency use have provided some insight; efficacy rates of the mRNA vaccines remain very high, despite up to one-fifth of vaccine recipients reporting use of analgesic or antipyretic medication. Public health authorities also continue to recommend the use of these medicines to treat post-COVID-19 vaccination symptoms (Table 4). Any restriction of the use of analgesic and antipyretic medicines in this setting could contribute to COVID-19 vaccine hesitancy, which would have substantial global public health implications.
References
London School of Hygiene & Tropical Medicine. COVID-19 vaccine tracker. https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/ (2021).
World Health Organization (WHO) list of COVID-19 vaccine EULs. https://extranet.who.int/pqweb/vaccines/covid-19-vaccines (2021).
Medicines and Healthcare products Regulatory Agency. Press release. UK medicines regulator gives approval for first UK COVID-19 vaccine. https://www.gov.uk/government/news/uk-medicines-regulator-gives-approval-for-first-uk-covid-19-vaccine (2021).
Our World in Data. Statistics and Research. Coronavirus (COVID-19) vaccinations. https://ourworldindata.org/covid-vaccinations (2021).
Lin, C., Tu, P. & Beitsch, L. M. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines (Basel). 9, 16 (2020).
Sridhar, S. et al. Effect of dengue serostatus on dengue vaccine safety and efficacy. N. Engl. J. Med. 379, 327–340 (2018).
Biswal, S. et al. Efficacy of a tetravalent dengue vaccine in healthy children and adolescents. N. Engl. J. Med. 381, 2009–2019 (2019).
Gans, H. A. et al. Deficiency of the humoral immune response to measles vaccine in infants immunized at age 6 months. JAMA 280, 527–532 (1998).
Aw, D. et al. Immunosenescence: emerging challenges for an ageing population. Immunology 120, 435–446 (2007).
Kwetkat, A. & Heppner, H. J. Comorbidities in the elderly and their possible influence on vaccine response. Interdiscip. Top. Gerontol. Geriatr. 43, 73–85 (2020).
Hervé, C., Laupèze, B., Del Giudice, G., Didierlaurent, A. M. & Tavares Da Silva, F. The how’s and what’s of vaccine reactogenicity. NPJ Vaccines. 4, 39 (2019).
Pulendran, B. & Ahmed, R. Immunological mechanisms of vaccination. Nat. Immunol. 12, 509–517 (2011).
Nakayama, T. Causal relationship between immunological responses and adverse reactions following vaccination. Vaccine 37, 366–371 (2019).
Beutler, B. Microbe sensing, positive feedback loops, and the pathogenesis of inflammatory diseases. Immunol. Rev. 227, 248–263 (2009).
Gonzalez Dias, P. et al. Methods for predicting vaccine immunogenicity and reactogenicity. Hum. Vaccin Immunother. 16, 269–276 (2020).
Chan, K. R. et al. Metabolic perturbations and cellular stress underpin susceptibility to symptomatic live-attenuated yellow fever infection. Nat. Med. 25, 1218–1224 (2019).
Chan, C. Y. et al. Early molecular correlates of adverse events following yellow fever vaccination. JCI Insight 2, e96031 (2017).
Querec, T. D. et al. Systems biology approach predicts immunogenicity of the yellow fever vaccine in humans. Nat. Immunol. 10, 116–125 (2009).
Das, R. R., Panigrahi, I. & Naik, S. S. The effect of prophylactic antipyretic administration on post-vaccination adverse reactions and antibody response in children: a systematic review. PLoS One 9, e106629 (2014).
Chau-Glendinning, H., Baber, B. & Neher, J. O. J Do prophylactic antipyretics reduce vaccination-associated symptoms in children? Fam. Pract. 69, E21–E22 (2020).
Koufoglou, E., Kourlaba, G. & Michos, A. Effect of prophylactic administration of antipyretics on the immune response to pneumococcal conjugate vaccines in children: a systematic review. Pneumonia (Nathan). 13(1), 7 (2021). Apr 25.
Scheifele, D. & Ward, B. Fever prophylaxis can reduce vaccine responses: A caution. Paediatr. Child Health 23, 245–246 (2018).
Agard, M., Asakrah, S. & Morici, L. A. PGE2 suppression of innate immunity during mucosal bacterial infection. Front Cell Infect. Microbiol. 3, 45 (2013).
Ryan, E. et al. Activated human B lymphocytes express cyclooxygenase-2 and cyclooxygenase inhibitors attenuate antibody production. J. Immunol. 174, 2619–2626 (2005).
Falup-Pecurariu, O. et al. Effects of prophylactic ibuprofen and paracetamol administration on the immunogenicity and reactogenicity of the 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugated vaccine (PHiD-CV) co-administered with DTPa-combined vaccines in children: an open-label, randomized, controlled, non-inferiority trial. Hum. Vaccin Immunother. 13, 649–660 (2017).
Prymula, R. et al. Effect of prophylactic paracetamol administration at time of vaccination on febrile reactions and antibody responses in children: two open-label, randomised controlled trials. Lancet 374, 1339–1350 (2009).
Prymula, R., Habib, A., François, N., Borys, D. & Schuerman, L. Immunological memory and nasopharyngeal carriage in 4-year-old children previously primed and boosted with 10-valent pneumococcal non-typeable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) with or without concomitant prophylactic paracetamol. Vaccine 31, 2080–2088 (2013).
Sil, A. et al. Effect of prophylactic or therapeutic administration of paracetamol on immune response to DTwP-HepB-Hib combination vaccine in Indian infants. Vaccine 35, 2999–3006 (2017).
Aoki, F. Y. et al. Effects of acetaminophen on adverse effects of influenza vaccination in health care workers. CMAJ 149, 1425–1430 (1993).
Wysocki, J. et al. A randomized study of fever prophylaxis and the immunogenicity of routine pediatric vaccinations. Vaccine 35, 1926–1935 (2017).
Walter, E. B. et al. The effect of antipyretics on immune response and fever following receipt of inactivated influenza vaccine in young children. Vaccine 35, 6664–6671 (2017).
Lafferty, W. P., Selinger, D. S., Schiffman, G. & Goodwin, J. S. Response to pneumococcal vaccine in the elderly: no enhancement by indomethacin. J. Immunopharmacol. 3, 241–250 (1981).
Agarwal, D. et al. Immune response to influenza vaccination in the elderly is altered by chronic medication use. Immun. Ageing 15, 19 (2018).
Jackson, M. L., Bellamy, A., Wolff, M., Hill, H. & Jackson, L. A. Low-dose aspirin use does not diminish the immune response to monovalent H1N1 influenza vaccine in older adults. Epidemiol. Infect. 144, 768–771 (2016).
Lamb, Y. N. BNT162b2 mRNA COVID-19 vaccine: first approval. Drugs 81, 495–501 (2021).
Comirnaty. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/comirnaty-epar-product-information_en.pdf (2021).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Hwang, Y. H. et al. Can reactogenicity predict immunogenicity after COVID-19 vaccination? Korean J. Intern Med. 36, 1486–1491 (2021).
Furer, V. et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann. Rheum. Dis. 80, 1330–1338 (2021).
Corbett, K. S. et al. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature 586, 567–571 (2020).
COVID-19 vaccine Moderna. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/spikevax-previously-covid-19-vaccine-moderna-epar-product-information_en.pdf (2021).
Anderson, E. J. et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N. Engl. J. Med. 383, 2427–2438 (2020).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 384, 403–416 (2021).
Soiza, R. L., Scicluna, C. & Thomson, E. C. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing 50, 279–283 (2021).
ChAdOx1-S. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/covid-19-vaccine-astrazeneca-product-information-approved-chmp-29-january-2021-pending-endorsement_en.pdf (2021).
COVISHIELD. Summary of product characteristics. https://nafdac.gov.ng/wp-content/uploads/Files/SMPC/SmPC-COVISHIELD_01-01-2021.pdf (2021).
Ramasamy, M. H. et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 396, 1979–1993 (2021).
Bos, R. et al. Ad26 vector-based COVID-19 vaccine encoding a prefusion-stabilized SARS-CoV-2 spike immunogen induces potent humoral and cellular immune responses. NPJ Vaccines. 5, 91 (2020).
Ad26.COV2-S. Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/covid-19-vaccine-janssen-epar-product-information_en.pdf (2021).
Sadoff, J. et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N. Engl. J. Med. 384, 2187–2201 (2021).
Wang, H. et al. Development of an inactivated vaccine candidate, BBIBP-CorV, with potent protection against SARS-CoV-2. Cell 182, 713–721 (2020).
Xia, S. et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect. Dis. 21, 39–51 (2021).
Zhang, Y. et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18-59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 21, 181–192 (2021).
Wu, Z. et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 21, 803–812 (2021).
Munro, A. P. S. et al. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. Lancet 398, 2258–2276 (2021).
Folegatti, P. M. et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet 396, 467–478 (2020).
Walsh, E. E. et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N. Engl. J. Med. 383, 2439–2450 (2020).
Food and Drug Administration Briefing Document. Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. https://www.fda.gov/media/146217/download (2021).
Tan, A. T. et al. Early induction of functional SARS-CoV-2-specific T cells associate with rapid viral clearance and mild disease in COVID-19 patients. Cell Rep. 34, 108728 (2021).
Swadling, L. et al. Pre-existing polymerase-specific T cells expand in abortive seronegative SARS-CoV-2. Nature 601, 110–117 (2022).
Bozkurt, B., Kamat, I. & Hotez, P. J. Myocarditis with COVID-19 mRNA vaccines. Circulation 144, 471–484 (2021).
Diaz, G. A. et al. Myocarditis and pericarditis after vaccination for COVID-19. JAMA 326, 1210–1212 (2021).
Perez, Y. et al. Myocarditis following COVID-19 mRNA vaccine: a case series and incidence rate determination. Clin Infect Dis. ciab926. https://doi.org/10.1093/cid/ciab926 (2021).
Elalamy, I. et al. SARS-CoV-2 vaccine and thrombosis: an expert consensus on vaccine-induced immune thrombotic thrombocytopenia. Thromb. Haemost. 121, 982–991 (2021).
Liu, P. P., Blet, A., Smyth, D. & Li, H. The science underlying COVID-19: implications for the cardiovascular system. Circulation 142, 68–78 (2020).
Ostrowski, S. R. et al. Inflammation and platelet activation after COVID-19 vaccines – possible mechanisms beyond vaccine-induced immune thrombocytopenia and thrombosis. Front Immunol. Nov. 23, 779453 (2021).
Acknowledgements
This study was funded by GlaxoSmithKline. We thank Maxime Herve, Kamran Siddiqui, and Stephane Bissonnette from GlaxoSmithKline for their contributions to the review process. We also thank Ahsia Iqbal, PharmD, Rutgers University/GSK Consumer Health Postdoctoral Fellow, for research support during the development of this manuscript. Medical writing and editorial assistance were provided by Tony Reardon of Aura, a division of Spirit Medical Communications Group Ltd, funded by GlaxoSmithKline.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception of the work; to the acquisition, analysis, or interpretation of data; and have drafted the work or substantively revised it. All authors have approved the submitted version (and any substantially modified version that involves the author’s contribution to the study); and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
Eng Eong Ooi and Camille Locht have no potential competing interests to declare. Arti Dhar, Richard Petruschke, and Philippe Buchy are employees of GlaxoSmithKline. Jenny Guek Hong Low receives salary support from the National Medical Research Council of Singapore.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ooi, E.E., Dhar, A., Petruschke, R. et al. Use of analgesics/antipyretics in the management of symptoms associated with COVID-19 vaccination. npj Vaccines 7, 31 (2022). https://doi.org/10.1038/s41541-022-00453-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-022-00453-5
This article is cited by
-
Ibuprofen, other NSAIDs and COVID-19: a narrative review
Inflammopharmacology (2023)
-
Sublethal effects of acetaminophen exposure on benthic aquatic animal (Hydra magnipapillata)
Molecular & Cellular Toxicology (2023)
-
Pain Management in the Post-COVID Era—An Update: A Narrative Review
Pain and Therapy (2023)
-
Spotlight on therapeutic efficiency of mesenchymal stem cells in viral infections with a focus on COVID-19
Stem Cell Research & Therapy (2022)