Abstract
Inhaled corticosteroid (ICS) therapy is widely prescribed without a history of exacerbations and consensus guidelines suggest withdrawal of ICS in these patients would reduce the risk of side effects and promote cost-effective prescribing. The study describes the prescribing behaviour in the United Kingdom (UK) in relation to ICS withdrawal and identifies clinical outcomes following withdrawal using primary and secondary care electronic health records between January 2012 and December 2017. Patients with a history ≥12 months’ exposure who withdrew ICS for ≥6 months were identified into two cohorts; those prescribed a long-acting bronchodilator maintenance therapy and those that were not prescribed any maintenance therapy. The duration of withdrawal, predictors of restarting ICS, and clinical outcomes were compared between both patient cohorts. Among 76,808 patients that had ≥1 prescription of ICS in the study period, 11,093 patients (14%) withdrew ICS therapy at least once during the study period. The median time without ICS was 9 months (IQR 7–14), with the majority (71%) receiving subsequent ICS prescriptions after withdrawal. Patients receiving maintenance therapy with a COPD review at withdrawal were 28% less likely to restart ICS (HR: 0.72, 95% CI 0.61, 0.85). Overall, 69% and 89% of patients that withdrew ICS had no recorded exacerbation event or COPD hospitalisation, respectively, during the withdrawal. This study provides evidence that most patients withdrawing from ICS do not experience COPD exacerbations and withdrawal success can be achieved by carefully planning routine COPD reviews whilst optimising the use of available maintenance therapies.
Similar content being viewed by others
Introduction
International clinical guidelines on the management of Chronic Obstructive Pulmonary Disease (COPD), Global Initiative for Chronic Obstructive Lung Disease (GOLD) 20201,2,3 recommend long-acting inhaled bronchodilators, including β2-agonists (LABA) and anti-muscarinic agents (LAMA) as maintenance therapies. These agents can be prescribed as a monotherapy dose, fixed dose of dual LAMA/LABA therapy, or in combination with inhaled corticosteroids (ICS) for the symptomatic management of COPD and the prevention of COPD-related exacerbations.
The GOLD treatment strategy recommends that ICS (prescribed as a combination inhaler with a LABA or as part of triple-therapy regimen with LAMA and LABA) are reserved for COPD patients with frequent or severe exacerbations, and research shows that certain features might identify patients more or less likely to respond well to treatment with ICS, including asthma-like phenotype or biomarkers such as eosinophilia4,5,6,7,8. However, considerable dissociation has been reported between guideline recommendations and clinicians’ practices9,10,11 despite significant efforts to promote and disseminate the GOLD strategy12. ICS are often inappropriately prescribed for patients with mild or moderate COPD without a history of exacerbations resulting in up to 70% of patients in current practice receiving ICS-containing regimens13,14. There is a lack of evidence of the benefit of ICS in patients with preserved lung function and no history of exacerbations15,16. Safety concerns, particularly regarding increased incidence of pneumonia, osteoporosis, bruising, adrenal suppression, and diabetes have been reported in ICS users17.
It has been proposed that ICS should be withdrawn in patients who may have been prescribed this therapy inappropriately, to reduce side effects and promote cost-effective prescribing18,19,20. The recently published European Respiratory Society (ERS) guidelines on ICS withdrawal suggest patients withdrawing ICS should receive ongoing maintenance therapy with a bronchodilator21. While guidelines and clinical opinion have been shared around how to withdraw ICS22,23,24,25, there is limited evidence on the extent to which withdrawal recommendations have been adopted in primary care26. The aim of this study is to describe the trends in ICS withdrawal and the outcomes for patients receiving long-acting bronchodilator maintenance therapy (LAMA or LABA monotherapy or combination dual therapy), compared to patients not receiving any maintenance bronchodilators. Secondly, this study will aim to identify patient characteristics associated with successful withdrawal of ICS.
Methods
Study design and Inclusion criteria
This retrospective cohort study included patients belonging to UK general practices contributing data to the Clinical Practice Research Datalink (CPRD), the world’s largest longitudinal primary care database that is utilised for pharmacoepidemiologic research27,28. The data encompasses approximately 60 million patients; GPs voluntarily contribute the data which is automatically transferred from the routine patient care and it is representative of the UK population27.
Included patients in this study were those with a confirmed COPD record for adults ≥35 years of age at diagnosis, where the diagnosis of a COPD was defined using any record of a diagnostic Read Code for COPD in primary care records or COPD ICD-10 code in hospital records. The accuracy of COPD diagnosis in CPRD has been previously validated29. Patients were included if they were withdrawing a long-term ICS prescription between January 2012 to December 2017. To identify a group of patients with long-term ICS prescription, we required a minimum historical period of 12 months’ persistent exposure to ICS therapy (alone or in any combination) after allowing for the therapy period (calculated using amount prescribed or an imputed 28 days where data were missing). Additionally, patients were required to be currently registered in the observational period (January 2012 to December 2017) in general practices that contain research quality data linked with patient and practice-level secondary care hospital data in the Hospital Episode Statistics (HES) database. The final sample size for the study was based on the above basic eligibility criteria in addition to ICS-withdrawal requirements.
Definition of ICS withdrawal and data capture
Since gaps in prescription records of a few months are common within CPRD, a minimum ICS-free period was required to identify true withdrawal rather than a short period during which patients did not receive prescriptions. For the purposes of analysis, we therefore defined “withdrawal” as a period of at least 6 months with no record of ICS prescription. Patients’ withdrawal period was then considered from the index date—defined as the last date of ICS therapy based on the duration of medication prescribed, until the earlier date of subsequent ICS prescription (alone or in any combination), study end, acceptable research quality data (patient remains registered in GP practice without any data gaps), transferring out of the registered practice, or death. For patients with multiple periods of ICS withdrawal, we considered the first occurring period. Data capture consisted of a 2-year period prior to ICS withdrawal and minimum 6 months period after the withdrawal date to identify clinical outcomes.
Outcomes of interest
Outcomes of interest in this study included time without ICS; the number of exacerbations (defined as antibiotic and oral corticosteroid (OCS) prescriptions taken together for 5–14 days or lower respiratory tract infection Read Code, or an acute exacerbation Read Code where that did not coincide with a spirometry test)30 during the patient’s ICS-withdrawal period; the number of COPD hospitalisations (ICD-10 code J44.0, J44.1 or J22 in any position of hospital episode); the number of interactions with a general practitioner (GP); the number of short-acting bronchodilator prescriptions (i.e. rescue therapy); and number of pneumonia episodes (Read Code and ICD-10 codes J12-J16 and J18). Measurements of these outcomes were taken from distinct patient groups (patients receiving bronchodilation maintenance therapy compared to patients not receiving bronchodilation therapy).
Patient characteristics and covariates
Baseline characteristics included age at the start of withdrawal, sex, BMI, smoking status, vaccination history (influenza or pneumococcal vaccination), co-morbidities (heart disease or asthma), prior history of COPD exacerbations, recent eosinophil count and percent predicted forced expiratory volume in 1 s (FEV1). In addition, the coding of routine COPD reviews (6 or 12-month intervals) with spirometry procedure on the day was also recorded. All clinical and demographic covariates were collected at baseline using the primary care electronic health data in CPRD.
Two distinct patient groups were defined—those receiving one or more long-acting bronchodilator maintenance therapies during the ICS-withdrawal period, and those with no long-acting bronchodilator treatment during the period of ICS withdrawal. Long-acting bronchodilator treatment in the maintenance group consisted of LAMA or LABA monotherapy, LAMA/LABA combination fixed dose, or LAMA + LABA combination free dose which includes separate inhalers prescribed for intended regular daily usage, not for as-needed use31.
Statistical analysis
Baseline characteristics and follow-up patient outcomes were described for patients receiving or not receiving inhaled maintenance therapy during their ICS-withdrawal period. Cross-tabulated summary statistics were used to describe these patient characteristics and included mean ± standard deviation (SD) for continuous data and number (percentage) for categorical data. Missing data for covariates were quantified without imputation due to the relative percentage of missing data.
Kaplan–Meier plots to describe the probability of ICS-free time (months) and median ICS-free time (months) were calculated in patients that were prescribed a maintenance therapy compared with those without maintenance therapies. The frequency and percentage of patients lost to follow-up were also quantified by corresponding reasons for the loss to follow-up. A univariable Cox-proportional hazards model was initially performed to identify significant predictors of restarting ICS therapy at the level of α = 0.05. These significant predictors were used to develop a two-sided multivariable predictive model using backwards variable selection at the level of α = 0.2 to produce a parsimonious complete-case model adjusting for confounders. Hazard function (hazard ratio) for patients on maintenance therapy and for patients without maintenance therapy after withdrawal are assumed to be proportional, with a constant hazard ratio over time. Potential interactions were also tested using the final multivariable model. For these analyses, those who received their first maintenance therapy prescription after the first 6 months of withdrawal were considered not on maintenance therapy at the index to avoid immortal time bias.
In a sensitivity analysis, we used a time-dependent variable, which changed from no maintenance therapy to the use of maintenance therapy in patients who received their first maintenance therapy after the first 6 months. In an additional sensitivity analysis, the median duration of ICS-free time was repeated based on a minimum 9 months of ICS-free time prior to the index date to understand whether a longer baseline ICS-free time would influence the number of exacerbations in patients receiving maintenance treatment or not receiving maintenance treatment.
The analyses were performed in accordance with relevant regulations and guidelines. This study was reviewed and approved by the Independent Scientific Advisory Committee for Medicines and Healthcare products Regulatory Agency (MHRA) database research (ISAC number 17195RA) and by an internal scientific committee of the study sponsor. As this was a non-interventional study using anonymised data, no patient consent was necessary. Primary and secondary database access and data extraction were restricted to the corresponding author who was also responsible for the creation of the final study population and statistical analysis. Raw data extracts were assessed for outliers and cleaned to provide a clinically and statistically complete dataset. Data linkage between primary and secondary care data was performed by merging and appending based on a common patient identification number for both databases. Covariates were stratified by clinical thresholds and aggregated for n < 10 patients. All cleaning methods and analyses were conducted using SAS (SAS Institute Inc., Cary, NC, USA) and STATA/IC 15.0.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Cohort identification and characteristics
We identified 76,808 COPD patients that had ≥1 prescription of ICS in the study period. Of these patients, 11,093 (14.4%) withdrew an ICS therapy at least once during the study period having had >12 months use of ICS prior to this withdrawal (Fig. 1). Overall, these patients had a mean age of 70 (SD 15.6) and 52.8% were female. During the observed withdrawal period, 3849 patients (34.7%) were prescribed ≥1 maintenance therapy and 7244 patients (65.3%) were not prescribed any maintenance therapy. Of those who were prescribed maintenance therapy, 343 (8.9%) received their first prescription after the initial 6-month window that defined withdrawal. Patients who were prescribed a maintenance therapy during the withdrawal period were more likely to have FEV1% of <50% (maintenance therapy: 22.7%; no maintenance therapy: 10.7%; P < 0.001), MRC dyspnoea score of ≥3 (maintenance therapy: 47.5%; no maintenance therapy: 21.5%; P < 0.001) and be classified as GOLD group D (maintenance therapy: 20%; no maintenance therapy: 7.9%; P < 0.001). In addition, patients on maintenance therapy had higher hospitalised or non-hospitalised exacerbations (maintenance therapy: 59.3%; no maintenance therapy: 41.3%) and a higher percentage of pneumonia diagnosis (maintenance therapy: 23.2%; no maintenance therapy: 17.2%; P < 0.001) in the year prior to the withdrawal of ICS (Table 1).
Withdrawal period characteristics
Among patients prescribed maintenance therapy during the ICS-withdrawal period, 77% (n = 2965 of 3849) received a LAMA monotherapy. Despite lower utilisation of dual therapy compared with monotherapy, patients receiving LAMA/LABA fixed-dose or LAMA + LABA free-dose combination were observed to remain on ICS-free therapy on average longer than patients taking monotherapy (LAMA/LABA: 18.3 months, LAMA + LABA: 20.2 months; LAMA: 13.6 months, LABA: 14.7 months), respectively. Of all patients that withdrew with maintenance therapy, 22.8% (n = 877 of 3849) had a COPD review recorded which coincided at the start of their withdrawal period and 10.5% (n = 364 of 3849) at the end of withdrawal. Similarly, patients without maintenance therapy prescribed were more likely to have a COPD review at the start of withdrawal (7.1%, n = 517 of 7244) than at the end (4.5%, n = 326 of 7244). Withdrawal period ended due to a subsequent prescription of an ICS therapy (70.7%; n = 7846 of 11,093) compared with patients that were lost to follow-up which included patients records that were no longer of research quality (14.1%, n = 1567 of 11,093), transferred out of a GP (4.5%, n = 497 of 11,093), or died (4%; n = 446 of 11,093). In this study, 6.7%, 739 of 11,093 patients reached the study end date without restarting ICS (Supplementary Table 1).
Patients with a subsequent ICS prescription were likely to commence the same drug and device as the last ICS therapy prior to withdrawal (83%; n = 6515 of 7846). Although patients were overall less likely to be prescribed a different ICS therapy at the end of withdrawal, patients receiving maintenance therapy were more likely to switch to a different ICS therapy (25%, n = 627 of 2521) than those without maintenance therapy (13.2%; n = 704 of 5325) (Table 2).
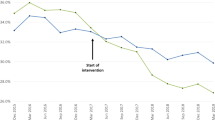
The observed median ICS-free time was 9 months (IQR 7–13.9). This differed slightly when comparing whether patients were prescribed a maintenance therapy during the withdrawal period or not (median: 9.6 months vs. 8.7 months, respectively) (Fig. 2). After accounting for censoring, the estimated median time without ICS in patients withdrawing with maintenance therapy and without maintenance therapy was 10.4 months (95% CI: 10.1, 10.8) and 9.5 months (95% CI: 9.3, 9.7), respectively as illustrated in the Kaplan–Meier curve (Fig. 3). The mean withdrawal period was consistently higher in patients receiving maintenance therapy in each calendar year compared with patients not receiving maintenance therapy (Supplementary Fig. 1).
The duration of withdrawal for patients receiving or not receiving maintenance therapy during withdrawal and or ICS after withdrawal is illustrated in this figure. Data shown represent the minimum, lower quartile, median, and upper quartile. Maximum values not shown (maximum = 76 months among patients receiving a subsequent prescription of ICS; maximum = 77 months in all other groups).
Characteristics associated with time without ICS
The Cox-proportional hazards model presented in Table 3 illustrates the predictors associated with ICS-free time. In the univariable analysis, the use of maintenance therapy, a COPD review at start of withdrawal of ICS, absence of heart disease, and higher FEV1% predicted were each more likely to be associated with a longer time without ICS. Patients with an asthma history, increasing blood eosinophil count, prior exacerbations, and vaccination history were associated with a shorter time without ICS. The multivariable model illustrated that patient with asthma history of >2 years before COPD diagnosis and ≤2 years before COPD diagnosis or withdrawal were 28% (HR: 1.28; 95% CI: 1.18, 1.38; P < 0.001) and 12% (HR: 1.12; 95% CI: 1.04, 1.22; P < 0.001) more likely to restart ICS compared with patients without a history of asthma, respectively. Although statistically significant (P < 0.001), FEV1% and exacerbation history were marginally associated with ICS-free time (Table 3).
In the multivariable model, the effect of maintenance therapy alone on ICS-free time was diminished (HR: 0.95; 95% CI: 0.88, 1.02; P = 0.16), but with statistical evidence of an interaction with the presence of COPD review period at the start of withdrawal. The interaction between maintenance therapy and COPD review suggested that patients on maintenance therapy who had a COPD review coded coinciding with withdrawal date were 28% less likely (HR: 0.72; 95% CI: 0.61, 0.85; P < 0.001) to restart ICS compared with patients with no maintenance therapy that did not have a COPD review at the start of withdrawal (Table 4).
In addition, COPD review at the start of withdrawal was independently shown to be associated with a longer withdrawal period until ICS restart in both the univariable (HR: 0.67; 95% CI: 0.62, 0.72; P < 0.001) and multivariable (HR: 0.86; 95% CI: 0.76, 0.97; P = 0.01) models (Table 3).
Patient outcomes
During the ICS-free period studied, the majority of patients that had withdrawn ICS did not experience any exacerbations (N = 7654; 69%), COPD-related hospitalisation (N = 9873; 89%), primary care recorded pneumonia episodes (N = 9651; 87%), or hospitalised pneumonia episodes (N = 10,316; 93%) (Fig. 4). COPD exacerbations were higher in the maintenance therapy group with most of these patients experiencing ≥1 exacerbation event prior to the start of maintenance therapy (N = 1693 of 3849 patients, 44%; P < 0.001) compared to patients without maintenance therapy (N = 2622 of 11,093 patients; 24%). The overall rate of hospitalised pneumonia episodes remained similar but slighter higher in patients receiving maintenance therapy (maintenance therapy: 0.45 per 1000 person-days, P = 0.02; no maintenance therapy: 0.41 per 1000 person-days) (Supplementary Table 3).
Sensitivity analysis
Increasing the minimum time defining the ICS-free period from 6 months to 9 months reduced the number of patients defined as withdrawing ICS therapy from 11,093 to 5544. Of those withdrawing, 2116 patients (38.2%) received maintenance therapy during the withdrawal period and 3428 patients (61.8%) did not receive any maintenance therapy. As in the main analysis, the observed median withdrawal time up to the restart of ICS was longer in patients receiving maintenance therapy than in those that did not (12.6 months; IQR 10.3–17.1) vs. (11.7 months; IQR 10–15.4).
A minority of patients receiving the first maintenance therapy after the first 6 months of ICS-free time (8.9%, N = 343 of 3849) were originally categorised in the regression models as having no maintenance therapy to prevent immortal time bias. These patients were reassigned to the maintenance therapy group at the point of their first maintenance therapy prescription to understand the impact of a time-dependent variable in the association between use of maintenance therapy and ICS-free time. The reanalysis of time to ICS restart for these patients showed comparable results to the primary analysis (Supplementary Table 2).
Lastly, the proportion of patients with long-term (12 or more months) ICS termination without an observed restart was calculated for patients receiving maintenance therapy and for patients without maintenance therapy. Patients on maintenance therapy were more likely to remain ICS free for ≥12 months. Approximately 1.4% (n = 52 of 3849) patients receiving therapy had an ICS withdrawal >5 years compared with 0.73% (n = 53 of 7244) patients without therapy. Although it is not known whether patients restarted ICS after the end of the study period, this subgroup of patients with >5 years of ICS withdrawal may indicate a permanent shift to non-ICS maintenance therapies.
Discussion
This study describes COPD patients on regular ICS therapy who underwent a period without evidence of ICS prescription of at least 6 months. Of patients who had at least 12 months of ICS use prior to withdrawal, 11,093 (14.4%) withdrew ICS with approximately one-third receiving maintenance therapy at some point during the period following withdrawal. The remaining (65%) of patients that did not receive maintenance therapy in the period following ICS withdrawal may include patients with mild or improving symptoms that needed minimal intervention. In addition, these patients may have been prescribed a short-acting muscarinic antagonist (SAMA) and or short-acting beta-agonist inhaler (SABA) inhaler to control symptoms when needed. In addition, GOLD classification and exacerbation rates between patients receiving maintenance therapy compared to those not receiving maintenance therapy may indicate that this cohort overall had the less severe disease when contrasted to patients receiving inhaled maintenance therapy.
Overall, patients that received maintenance therapy had a longer predicted and observed withdrawal time than those without maintenance therapy and were marginally less likely to restart ICS. Routine COPD review recording coinciding with the start of maintenance therapy and a previous asthma diagnosis were key predictors of time to restarting ICS in the multivariable model. The major concern when withdrawing ICS is the possibility of triggering an exacerbation, but in this population, we found that most patients withdrawing ICS did not experience an exacerbation in the study period.
Despite the higher probability of being prescribed LAMA during withdrawal, patients that received dual therapy (LAMA/LABA or LAMA + LABA) were most likely to benefit with a longer observed ICS-free time compared with patients receiving monotherapies. Although NICE guidelines recommend dual therapy when ICS-based regimens are not needed, the finding in this study provides evidence of varied prescribing behaviour in primary care but further underscores the value of LAMA and LABA dual therapy as a more favourable maintenance treatment32.
Patients had a longer period without ICS when routine COPD review was recorded at the start of ICS withdrawal and maintenance therapy was prescribed, compared with patients without a maintenance therapy prescription. Annual patient COPD review with the GP is suggested within the primary care of Quality and Outcomes Framework33, but a GP-coded review cannot conclusively indicate that a formal COPD review with the patient took place. Alternatively, it is possible that the codes reflect the GP performing a review of the notes and prescriptions. Despite this possible rationale, COPD review codes were strongly and independently associated with ICS-free time suggesting a possible planned withdrawal and re-evaluation of a current treatment or supportive therapy. Additionally, these codes may also suggest that more reviewing of COPD medication is taking place in primary care.
Although this study was able to demonstrate the varying lengths of ICS-withdrawal period by patient characteristics and exposure to maintenance therapy, the electronic medical records did not include the reason for clinicians to initiate maintenance therapy or ICS re-initiation. As observed, just over one-half of patients receiving maintenance therapy had COPD exacerbations prior to the start of the maintenance therapy. This observation may suggest a confounding by indication bias such that clinicians maybe more likely to prescribe maintenance therapy in those they consider at higher risk of future exacerbations34. Consequently, the association between maintenance therapy and clinical outcomes during withdrawal must be interpreted with caution as the directionality of the association cannot be confirmed in this study. The effect of escalating or changing treatment class on withdrawal duration, COPD exacerbations, hospitalisations, and pneumonia episodes was not tested in this study but may provide insight as to how patient outcomes are linked with prescribing behaviours of physicians. Lastly, at baseline, the severity of COPD disease based on FEV1% was unknown in approximately one-half of all patients without maintenance treatment, which may indicate variability of how spirometry results are documented and coded. This variation in practice may result in a possible misdiagnosis of COPD or a possible misrepresentation of airflow limitation severity.
Based on the conclusions of recent meta-analyses, ICS withdrawal does not significantly increase the overall risk of COPD exacerbations; there are differences regarding FEV1 decline and quality of life metrics, which are on average below the minimal clinically important difference35,36. However, the authors note that current evidence does not evaluate the impact of ICS withdrawal after clustering COPD patients with regard to phenotype characteristics (e.g. frequent exacerbators, emphysema- hyperinflation or COPD with an asthma component), the rate of exacerbations/year (i.e.<1; ≥1 and ≤2; >2), the decline of lung function (rapid decliners vs. slower decliners) or the quality of life37,38,39. Recent studies examining primary and secondary care electronic records in the UK and Germany have also found that withdrawal of ICS is not associated with an increased risk of exacerbations compared to a cohort of COPD patients who continue ICS therapy40,41,42. A specific UK study using a large administrative healthcare database comparing a cohort of patients withdrawing from a triple-therapy ICS-based regimen also suggested no increase in moderate and severe exacerbations due to a higher number of pneumonia consultations recorded in primary care at baseline42. The current study adds further information as to the way ICS therapy is withdrawn in a primary care setting. Although a minority of patients received a COPD review when prescriptions for ICS were ceased, these patients were least likely to restart ICS, which suggests that withdrawing ICS may be a part of an ICS-step down plan, an approach that is recommended by The Primary Care Respiratory Society (PCRS)43. In this cohort, patients that experienced exacerbations were also more likely to be on maintenance therapy, but it is not possible to draw conclusions from this observation as there may be confounding factors that were not considered, unclassified disease severity groups at baseline, and a likely reverse causality between the need for maintenance therapy and clinical outcomes. For example, in the Copenhagen General Population Study44, adherence to maintenance medication for COPD was low, although this increased with the progressive severity of the disease as defined by the GOLD stage.
This study has several strengths to understand the characteristics of patients and associated periods of ICS withdrawal. We utilised data from a large, well-validated primary care database with linkage to secondary care data. The identification of acute exacerbations of COPD from electronic health records is well-validated, and since it is based on data from routine care, the prescription data are likely to be entered correctly as the electronic health record system is required to generate a patient prescription30,45. This study provides a good capture of general prescribing behaviour in the COPD patient population as these patients are predominately managed in primary care.
Nevertheless, we cannot know if the prescription was dispensed, nor whether the patient took the medication, and adherence to maintenance medication in COPD is known to be poor44. In this study, we were interested in the effects of ICS withdrawal, so we can be relatively confident that the absence of a prescription record indicates that medication has not been supplied. It is likely that these patients were prescribed short-acting bronchodilation therapy or supportive care therapies for the relief of both respiratory and non-respiratory symptoms respectively, suggestive that patients had regular or routine visits to the GP to manage symptoms during the withdrawal period, however; we cannot confirm that all cases of withdrawal are genuinely deliberate attempts to withdraw ICS at the direction of a GP. For some patients, experiencing unusually longer gaps between withdrawal date and re-uptake of ICS therapy could be attributed to failure to refill prescriptions (i.e. patient-driven withdrawal) or stockpiling of previously issued prescriptions of ICS monotherapy or ICS combined therapy with LAMA or LABA. Although previous studies have described how to minimise the risk of steroid withdrawal22,23,24,25, this study seeks to describe a steroid withdrawal population in practice. The comparison of patients in this study to those that did not withdraw ICS for a minimum of 6 months may provide insight on COPD exacerbations and outcomes, but we cannot guarantee a sufficient patient population of continuous long-term ICS use in addition to the historical 12-month persistent ICS use prior to index date. Patients are more likely to start and stop ICS perhaps due to changing clinical signs or higher exacerbations events compared to those on long-acting therapies only. For this reason, comparison ICS withdrawn patients to ICS persistent users may lead to differential misclassification of outcomes thus weakening the association between clinical outcomes and ICS withdrawal.
This study has also shown that many patients in the withdrawing population had an historic or concurrent asthma diagnosis and the decision to withdraw may be confounded by the coded diagnosis of asthma rather than COPD, with asthma diagnosis possibly over-recorded in individuals with COPD46. This may explain why concomitant asthma increased the risk of restarting ICS, as these patients were being managed more as asthma patients than COPD, although severity criteria specifically for asthma (e.g. Asthma Control Test score) were not captured in this study. Historical asthma diagnosis was also more prevalent in patients who did not receive maintenance therapy, which may suggest that these patients have stepped off ICS due to improvement of asthmatic symptoms.
Results from the IMPACT39 and SUNSET47 clinical trials suggest that the risk of exacerbations following ICS withdrawal, although small, primarily occurs in the first 28 days37 and the step down from LAMA/LABA in combination with ICS-based regimen to LAMA/LABA dual maintenance therapy show no significant difference in COPD exacerbations, especially in patients with blood eosinophils <0.3 × 109 cells/L45. Although the IMPACT trial has highlighted that sudden step down from triple therapy to dual maintenance therapy can introduce exacerbations, it may be due to the fact these patients were frequent exacerbators and characterised with asthmatic features who may have otherwise benefited from continued ICS treatment. Overall, these findings suggest that withdrawal must be carefully investigated on a case-by-case basis based on multiple patient-based factors. Our definition of withdrawal included a minimum 6-month ICS-free period and therefore could not specifically identify the immediate increased risks of ICS- withdrawal within this study, and therefore direct comparison with IMPACT and SUNSET is not possible. Our data provided insight into characteristics and longer-term outcomes of patients that were not restarted on ICS due to short-term reactions to withdrawal.
Whether withdrawal of ICS occurs in a planned or unplanned way, the majority of COPD patients withdrawing ICS did not experience exacerbations and COPD-related hospitalisations. When ICS-withdrawal occurs in a planned way with a COPD review taking place and maintenance therapy prescribed, the ICS-free period is longer compared to patients without a prescribed maintenance therapy or a recorded COPD review. This may result in the reduction of side effects and enable more cost-effective prescribing. This study provides evidence that ICS withdrawal results in minimal exacerbations of COPD, thus supporting the guidance on recent ERS ICS withdrawal21. Withdrawal success can be optimised by carefully planning COPD reviews whilst optimising the use of available maintenance therapies.
Data availability
Datasets are available on request from the CPRD. Their provision requires the purchase of a license, and our license does not permit us to make them publicly available to all. We used data from the version collected in January 2019 and have clearly specified the data selected in our Methods section. To allow identical data to be obtained by others, via the purchase of a license, we will provide the code lists on request. Licences are available from the CPRD (http://www.cprd.com): The Clinical Practice Research Datalink Group, The Medicines and Healthcare products Regulatory Agency, 5th Floor, 151 Buckingham Palace Road, Victoria, London SW1 W 9SZ.
Code availability
Statistical programming code that is customised for this manuscript analysis is completed in STATA version 15 and can be accessed upon request.
References
Initiative for Chronic Obstructive Lung Disease (GOLD) 2020 Report: Global strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease; 2020 (accessed April 4, 2021); https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf.
Agustí, A., Vogelmeier, C. & Faner, R. COPD 2020: changes and challenges. Am. J. Physiol. Lung Cell Mol. Physiol. 319, 879–883 (2020).
Singh, D. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur. Respir. J. 53, 1900164 (2019).
Suissa, S., Dell’Aniello, S. & Ernst, P. Comparative effectiveness of LABA-ICS versus LAMA as initial treatment in COPD targeted by blood eosinophils: a population-based cohort study. Lancet Respir. Med. 6, 855–862 (2018).
Siddiqui, S. H. et al. Blood eosinophils: a biomarker of COPD exacerbation reduction with inhaled corticosteroids. Int J. Chron. Obstruct Pulmon Dis. 13, 3669–3676 (2018).
Mathioudakis, A., Foden, P. & Vestbo, J. Late breaking abstract—blood eosinophil count (EOS) can accurately predict responsiveness to inhaled corticosteroids (ICS) in COPD, but only if measured while patients are not receiving steroids. Eur. Respiratory J. 52, OA2125 (2018).
Harries, T. H. et al. Blood eosinophil count, a marker of inhaled corticosteroid effectiveness in preventing COPD exacerbations in post-hoc RCT and observational studies: systematic review and meta-analysis. Respir. Res. 21, 3 (2020).
Ashdown, H. F. et al. Blood eosinophils to guide inhaled maintenance therapy in a primary care COPD population. ERJ Open Res. 8, 00606–02021 (2021).
White, P., Thornton, H., Pinnock, H., Georgopoulou, S. & Booth, H. P. Overtreatment of COPD with inhaled corticosteroids-implications for safety and costs: cross-sectional observational study. PLoS ONE 8, e75221 (2013).
Wurst, K. E., Punekar, Y. S. & Shukla, A. Treatment evolution after COPD diagnosis in the UK primary care setting. PLoS ONE 9, e105296 (2014).
Brusselle, G. et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int. J. Chron. Obstruct Pulmon Dis. 10, 2207–2217 (2015).
Seaman, J., Leonard, A. C. & Panos, R. J. Health care utilization history, GOLD guidelines, and respiratory medication prescriptions in patients with COPD. Int. J. Chron. Obstruct Pulmon Dis. 5, 89–97 (2010).
Corrado, A. & Rossi, A. How far is real life from COPD therapy guidelines? An Italian observational study. Respir. Med. 106, 989–97. (2012).
Chalmers, J. D. et al. Determinants of initial inhaled corticosteroid use in patients with GOLD A/B COPD: a retrospective study of UK general practice. npj Prim. Care Respir. Med. 27, 43 (2017).
Barnes, P. J. Inhaled corticosteroids in COPD: a controversy. Respiration 80, 89–95 (2010).
Chalmers, J. D. et al. Assessing the healthcare resource use associated with inappropriate prescribing of inhaled corticosteroids for people with chronic obstructive pulmonary disease (COPD) in GOLD groups A or B: an observational study using the Clinical Practice Research Datalink (CPRD). Respir. Res. 19, 63 (2018).
Gartlehner, G., Hansen, R. A., Carson, S. S. & Lohr, K. N. Efficacy and safety of inhaled corticosteroids in patients with COPD: a systematic review and meta-analysis of health outcomes. Ann. Fam. Med. 4, 253–262 (2006).
Magnussen, H. et al. WISDOM Investigators. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N. Engl. J. Med. 371, 1285–1294 (2014).
Wouters, E. F. et al. COSMIC (COPD and Seretide: a Multi-Center Intervention and Characterization) Study Group. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomised controlled trial. Thorax 60, 480–487 (2005).
Rossi, A., Guerriero, M. & Corrado, A., OPTIMO/AIPO Study Group. Withdrawal of inhaled corticosteroids can be safe in COPD patients at low risk of exacerbation: a real-life study on the appropriateness of treatment in moderate COPD patients (OPTIMO). Respir. Res. 15, 77 (2014).
Chalmers, J. D. et al. Withdrawal of inhaled corticosteroids in COPD: a European Respiratory Society guideline. Eur. Respir. J. 55, 2000351 (2020).
Kaplan, A. G. Applying the wisdom of stepping down inhaled corticosteroids in patients with COPD: a proposed algorithm for clinical practice. Int J. Chron. Obstruct Pulmon Dis. 10, 2535–2548 (2015).
Miravitlles, M. et al. A proposal for the withdrawal of inhaled corticosteroids in the clinical practice of chronic obstructive pulmonary disease. Respir. Res. 18, 198 (2017).
Yawn, B. P., Suissa, S. & Rossi, A. Appropriate use of inhaled corticosteroids in COPD: the candidates for safe withdrawal. npj Prim. Care Respir. Med. 26, 16068 (2016).
Chalmers, J. D. et al. Withdrawal of ICS treatment in primary care: a practical guide. Pr. Nurs. 28, 22–27 (2017).
Thio, S. L., Nam, J., van Driel, M. L., Dirven, T. & Blom, J. W. Effects of discontinuation of chronic medication in primary care: a systematic review of deprescribing trials. Br. J. Gen. Pract. 68, e663–e672 (2018).
Herrett, E. et al. Data resource profile: clinical practice research datalink (CPRD). Int. J. Epidemiol. 44, 827–836 (2015).
García Rodríguez, L. A. & Pérez Gutthann, S. Use of the UK general practice research database for pharmacoepidemiology. Br. J. Clin. Pharmacol. 45, 419–425 (1998).
Quint, J. K. et al. Validation of chronic obstructive pulmonary disease recording in the Clinical Practice Research Datalink (CPRD-GOLD). BMJ Open. 4, e005540 (2014).
Rothnie, K. J. et al. Validation of the recording of acute exacerbations of COPD in UK primary care electronic healthcare records. PLoS ONE 11, e0151357 (2016).
BNF Publications. Respiratory System. 2015. Airways Disease, Obstructive. (accessed February 25, 2022); https://www.bnf.org/wp-content/uploads/2015/08/Sample-pages-from-BNF-70.pdf.
NICE Guideline Updates Team (UK). Predicting and Preventing Exacerbations: Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management: Evidence Review E (National Institute for Health and Care Excellence (UK), 2018).
Baxter, N. Updated Respiratory QOF indicators included in the GP contract 2020. Prim. Care Respir. Soc. https://www.pcrs-uk.org/resource/updated-respiratory-qof-indicators-included-gp-contract-2020 (2020).
Signorello, L. B. et al. Confounding by indication in epidemiologic studies of commonly used analgesics. Am. J. Ther. 9, 199–205 (2002).
Calzetta, L. et al. Withdrawal of inhaled corticosteroids in COPD: a meta-analysis. Pulm. Pharm. Ther. 45, 148–158 (2017).
Gedebjerg, A. et al. Prediction of mortality in patients with chronic obstructive pulmonary disease with the new Global Initiative for Chronic Obstructive Lung Disease 2017 classification: a cohort study. Lancet Respir. Med. 6, 204–212 (2018).
Harlander, M., Barrecheguren, M., Turel, M. & Miravitlles, M. Should patients switched from D to B in the GOLD 2017 classification be discontinued from inhaled corticosteroids? COPD 14, 465–468 (2017).
Calverley, P. et al. Evaluating blood eosinophils and exacerbation history to predict ICS response in COPD. Pneumo 71, 251 (2017).
Suissa, S. & Drazen, J. M. Making sense of triple inhaled therapy for COPD. N. Engl. J. Med. 378, 1723–1724 (2018).
Oshagbemi, O. A. et al. Blood eosinophil counts, withdrawal of inhaled corticosteroids and risk of COPD exacerbations and mortality in the Clinical Practice Research Datalink (CPRD). COPD 16, 152–159 (2019).
Vogelmeier, C. et al. Real-life” inhaled corticosteroid withdrawal in COPD: a subgroup analysis of DACCORD. Int J. Chron. Obstruct Pulmon Dis. 12, 487–494 (2017).
Magnussen, H. et al. Withdrawal of inhaled corticosteroids versus continuation of triple therapy in patients with COPD in real life: observational comparative effectiveness study. Respir. Res. 22, 25 (2021).
Román-Rodríguez, M. Evaluation of Appropriateness of Inhaled Corticosteroids (ICS) Therapy in COPD and Guidance in ICS Withdrawal. (accessed 4 April, 2021); http://www.pcrs-uk.org/sites/pcrs-uk.org/files/SteppingDownICS_FINAL5.pdf.
Ingebrigtsen, T. S. et al. Low use and adherence to maintenance medication in chronic obstructive pulmonary disease in the general population. J. Gen. Intern Med. 30, 51–59 (2015).
Sperrin, M. et al. Chronic obstructive pulmonary disease exacerbation episodes derived from electronic health record data validated using clinical trial data. Pharmacoepidemiol Drug Saf. 28, 1369–1376 (2019).
Nissen, F. et al. Concomitant diagnosis of asthma and COPD: a quantitative study in UK primary care. Br. J. Gen. Pract. 68, e775–e782 (2018).
Chapman, K. R. et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am. J. Respir. Crit. Care Med. 198, 329–339 (2018).
Acknowledgements
The authors would like to thank Dr. Ruth Farmer and *Dr. Alicia Gayle for their input in the data analysis. In addition, the authors would like to thank Abigail Tebboth and Dr. Andrew Ternouth for their contribution in editing and interpreting the study findings, respectively. *Alicia Gayle is no longer an employee at Boehringer Ingelheim Ltd.; she is now, an employee of AstraZeneca plc, Cambridge, UK.
Author information
Authors and Affiliations
Contributions
S.P. contributed to the final data analysis, interpretation, and drafting of the final manuscript. S.D., K.M., Dr. H.F.A., and Prof. J.D.C. contributed to the plan, design, and interpretation of the study. All authors were involved in drafting the manuscript and commenting on the draft versions.
Corresponding author
Ethics declarations
Competing interests
S.P., S.D., and K.M. are employees of Boehringer Ingelheim Ltd. Dr. J.C. has received research grants from Boehringer Ingelheim, AstraZeneca, GlaxoSmithKline and Pfizer. Dr. J.C. has also received fees for consultancy and speaking from Boehringer Ingelheim. Dr. Helen Ashdown’s academic department receives money for her role in a collaborative project with Boehringer Ingelheim Ltd. We declare that none of the authors has competing financial or non-financial interests as defined by Nature Portfolio.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patel, S., Dickinson, S., Morris, K. et al. A descriptive cohort study of withdrawal from inhaled corticosteroids in COPD patients. npj Prim. Care Respir. Med. 32, 25 (2022). https://doi.org/10.1038/s41533-022-00288-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-022-00288-6
This article is cited by
-
Rational use of inhaled corticosteroids for the treatment of COPD
npj Primary Care Respiratory Medicine (2023)