Abstract
COPD is increasingly common in China but is poorly understood by patients, medications are not used as prescribed and there is no access to recommended non-pharmacological treatment. We explored COPD patients’ and general practitioners’ (GPs) knowledge of COPD, views on its management and the acceptability of a flexible lung health service (LHS) offering health education, exercise, self-management, smoking cessation and mental health support. Using a convergent mixed methods design, data were collected from patients and GPs using focus groups (FGs) in four Chinese cities, questionnaires were also used to collect data from patients. FGs were audio-recorded and transcribed. Quantitative data were analysed descriptively, thematic framework analysis was used for the qualitative data. Two-hundred fifty-one patients completed the questionnaire; 39 patients and 30 GPs participated in ten separate FGs. Three overarching themes were identified: patients’ lack of knowledge/understanding of COPD, current management of COPD not meeting patients’ needs and LHS design, which was well received by patients and GPs. Participants wanted COPD education, TaiChi, psychological support and WeChat for social support. 39% of survey responders did not know what to do when their breathing worsened and 24% did not know how to use their inhalers. 36% of survey respondents requested guided relaxation. Overall, participants did not fully understand the implications of COPD and current treatment was sub-optimal. There was support for developing a culturally appropriate intervention meeting Chinese patients’ needs, health beliefs, and local healthcare delivery. Further research should explore the feasibility of such a service.
Similar content being viewed by others
Introduction
As a leading cause of disability and mortality, Chronic Obstructive Pulmonary Disease (COPD) is a significant global public health challenge1. In China, where smoking prevalence is high2, COPD is the third most common cause of death with a prevalence of 13·7% in those aged 40 years or older3. Poor management results in frequent exacerbations and hospitalisation, and therefore high medical costs. In China patients can spend from 33–118% of their average annual income on medical bills, and medical costs to the state attributable to COPD are estimated at ¥195.6 ($30.3) billion, nearly 10% of China’s total health expenditure4.
Globally recognised guidelines5 recommend tailored treatment for COPD based on symptom profile using a combination of pharmacological and behavioural interventions such as self-management, smoking cessation support or pulmonary rehabilitation (PR)6. Despite being shown to be an effective and cost-effective therapeutic strategy7, access to PR is problematic due to cost, staff limitations, equipment and widespread lack of GP interest in offering PR, regardless of level of countries’ development8,9,10,11.
Research indicates that Chinese patients with COPD do not use their medications regularly, have poor understanding of their disease and less than a third participate in regular exercise3,12,13,14. In addition, adherence to PR in trials has been poor15,16. Research among healthcare professionals in China shows that prescribing does not always follow international guidelines, knowledge of COPD and PR is poor and PR is not routinely offered17,18,19,20. However, self-management programmes involving home exercise21 and information about COPD and its management in community settings have been shown to be effective in research studies22.
PR originated in the West, and is therefore influenced by Western culture. The poor uptake of PR in China may be influenced by local values and beliefs15,16,23, which are supported by the inclusion of traditional Chinese medicine (TCM) departments in state hospitals. Therefore, alternative, integrated treatments need to be investigated. A lung health service (LHS) is a more flexible concept, which could be tailored to local need and might include education, exercise, self-management, smoking cessation and psychological support. Involving patients and practitioners in the design of a LHS could help to reduce barriers and improve participation.
Through links with the International Primary Care Respiratory Group, Peking University First Hospital joined with the University of Birmingham (UoB) NIHR Global Health Research Group on Global COPD in Primary Care, “Breathe Well”, to conduct a mixed methods study aiming to explore COPD patients’ and GPs’ knowledge of COPD, their views on its management and the acceptability of a LHS. This was conducted in four primary care community health centres (CHCs) in four different cities in China: Beijing (North), Chengdu (Southwest), Guangzhou (South) and Shenyang (Northeast).
Methods
This convergent mixed methods study using quantitative (questionnaires) and qualitative focus groups (FGs) methods was conducted from February 2019 to June 2020 with ethical approval from the Ethics Review Board at Peking University First Hospital [No: 2019/52, 13/03/2019] and the Internal Review Ethics Committee at University of Birmingham [IREC2018/1413420, 11/11/2019].
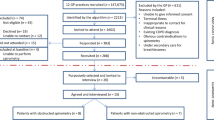
Participants and recruitment
Patients from urban CHCs in Beijing, Chengdu, Guangzhou and Shenyang, China with a spirometry-diagnosed COPD, and GPs with experience of managing COPD were eligible. We excluded those unable to give informed consent, to speak Mandarin or dialect of, and/or to travel to the FGs. Eligible patients were identified through hospital attendance records and through local GP lists. Researchers then telephoned potential participants to invite them to participate. Procedures for consent are explained below. All participants were free to withdraw at any time, but they were informed that their contributions could not be retrospectively removed from the FG analysis. The electronic data was archived to disc at the end of the study period (25.05.21) and will be destroyed after 5 years along with the paper consent forms.
Data collection (i): Questionnaires
We assessed patients’ knowledge and understanding of lung disease, identified their current treatment and explored their opinions on a future LHS using a self-constructed questionnaire incorporating validated questionnaires where available to assess outcomes. This included the Lung Information Needs Questionnaire24 to describe patients’ knowledge and understanding of their condition, the mMRC Questionnaire25 to measure breathlessness and the CAT26 to determine patients’ disease-specific health status. After data collection in Beijing was completed, the questionnaire design was reviewed and four additional questions added including the Godin-Shephard Leisure-time Physical Activity questionnaire27 to establish current physical exercise status (see Supplementary patient questionnaire). Patient consent was obtained and questionnaires completed when patients were next in attendance at the hospital. Patients participating in the FGs completed the questionnaires prior to the FG to avoid being influenced by other patients. Data were then entered onto REDCap28,29.
Sample size and statistical analysis
No formal sample size calculation was undertaken for this study but a pragmatic approach was taken to collect a representative sample of 100 patients in Beijing and 50 patients in each of the other three cities, around 250 in total. The primary outcome was treatment received by patients, reported as percentages of respondents. The secondary outcomes were patients’ knowledge of the disease and their preference for different treatment options. Descriptive statistics were conducted for all recorded variables using STATA v 15.130. For some questions, where data were missing, pragmatic assumptions were made in order to include the data in Supplementary Table 5.
Data collection (ii): Focus groups
We conducted two patient and two GP FGs with six to eight participants in Beijing; and one of each in the other three cities. Purposive sampling31 was used to ensure that all patient groups included at least one female, and as wide a mix of mMRC dyspnoea scores25 as possible. Prior to the COVID-19 pandemic, FGs in the first three cities were conducted face-to-face and written consent obtained on the day of the FG.
In response to COVID-19, FGs in Chengdu were conducted online using the Tencent Conference application, a popular conferencing platform in China, with video functioning. Written consent was obtained in the hospital, at participants’ convenience prior to the day of the FG. Structured topic guides (see Supplementary Topic guides) were used and refined iteratively as themes emerged. All FGs were audio-recorded and transcribed intelligent verbatim. Transcripts were anonymised. During the FG observational notes were taken by the co-facilitator (ZP).
Qualitative analysis
The transcribed FGs were independently coded by the FG facilitators (HP, ZP and ED) and discussed with the wider research team (RLA and NG). Definitions for each category and subcategory were developed during the process of coding and recorded in a coding diary. Once a coding framework had been agreed it was applied to the remainder of the FGs. The team met to critically reflect on and review interpretations throughout. The data were summarised in Excel using the Framework Method32 and themes identified. The analysis reported here focuses on data related to the development of a LHS.
Interpretation and synthesis of qualitative and quantitative data
The quantitative and qualitative data sets were analysed separately and independently from one another. Once both initial results were available, the lead researcher identified content areas represented in both data sets. The findings were then compared and contrasted in a table to aid understanding of perspectives from patients and GPs.
As findings emerged, the team discussed the extent to which, and in what ways, results from the two types of data converged and related to each other so as to produce a more complete understanding. Thus, both qualitative and quantitative data were used to answer our research question33,34.
Results
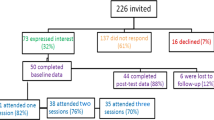
Flow of survey participants
Of 278 eligible COPD patients identified and invited, 23 declined to attend CHCs because of COVID-19 (see Supplementary Fig. 1). Of the 255 patients who provided consent, 4 withdrew because they did not have enough time to complete the questionnaire. In all, 251 patients completed the questionnaires.
Baseline characteristics
Baseline characteristics are given in Supplementary Table 1. Survey respondents had a mean age of 67.9 (SD 9.1) years, 183 (72.9%) were male, only 64 (25.5%) were current smokers. The majority had mild to moderate COPD with a range of co-morbidities, the top three being hypertension, asthma, and heart disease.
Thirty-nine patients (27 male) and 30 GPs (6 male) participated in ten separate FGs. FG patients had a mean age of 66.3 (SD 7.8) years and 23 patients had a COPD Assessment Test (CAT) score26 of 2 to 4, only 10 (25.6%) were current smokers. The majority of the GPs (20, 66.7%) had over 10 years clinical experience.
Study findings
Patients’ knowledge of COPD
Supplementary Table 2 (Questions 1–5) reports patients’ responses regarding knowledge/understanding of COPD. In summary, patients reported not receiving enough advice from their doctors. Over 50% said that there was no advice on how much or what kind of exercise they should do and over 40% no advice on diet, prognosis, breathlessness and management of exacerbations. The main causes of COPD were perceived as smoking, second-hand smoke and air pollution, and the main exacerbation triggers as colds/coughs/flu, air pollution, gases, fumes and dust at work and own or others’ smoking.
Current management of lung condition
Supplementary Table 2 (Questions 6–10) reports patients’ report of current management of COPD, their leisure-time exercise (LTE) and affordability of prescribed COPD medication. Patients had been prescribed different treatment options, of which long acting inhalers, oral medication/tablets and short acting bronchodilators were the most common. Up to 39.0% did not know what to do when breathing worsened and 24.3% did not know how to use prescribed inhalers. The majority of the subgroup of patients in Chengdu, Guangzhou and Shenyang were “moderately active” or “active”27. Only 42.6% could afford all their treatment.
Acceptability of a LHS to patients
Patient views regarding a LHS can be seen in Supplementary Table 3. In summary, the idea of the LHS was well received by patients. The top five preferred components were practicing breathing techniques and advice on: breathlessness, diet, education about lung condition and self-management techniques. Few prioritised stopping smoking, exercise, or psychological counselling. Distance from home was the most important factor influencing their decision to attend a LHS, followed by cost and ease of travel. Over 80% of the subgroup of patients would not pay more than ¥10 ($1.5), equivalent to the cost of five bus rides.
There were 3 main themes (Supplementary Fig. 2) identified from the focus groups:
Theme 1: Knowledge/understanding and experience of COPD
Patients were unfamiliar with symptoms of COPD, attributing them, for example, to heart disease and age and not seeking appropriate treatment
Over ten years ago, I felt tired all the time and my heart beat rapidly so I thought there was something wrong with my heart… I had a coronary angiography but found my heart very good [patient did not take any further action]. [P1, FG3]
I had always been in good health so did not pay attention to it [breathlessness]. [P9, FG1]
Patients lacked understanding about COPD medications. They were worried about dependence and side effects, so did not use them regularly.
I have an oxygen cylinder at home, but I seldom use it unless I have a fever or catch a cold…If I always passively inhale oxygen, then I might be unable to breathe by myself. That would be terrible. [P7, FG5]
I feel better after using my inhalers. But I’m afraid of becoming reliant on them, so stopped them. [P2, FG5]
Patients reported the negative impact of COPD on sleep, daily activities, memory, ability to work and mood, e.g., depression and short temperedness. They also reported the effect of weather on symptoms. The impact of COPD was worse in young patients and those with severe COPD.
Sometimes I feel uncomfortable and keep coughing at night, which makes me unable to fall asleep. The next day…I get angry with my family members because of small matters. [P2, FG1]
When I go to the south, where the air is moist, my throat becomes better and I rarely cough. [P17, FG2]
Every morning I must open the window, or I cannot breathe… I am very afraid when short of breath. [P9, FG5]
Both GPs and patients reported the burden COPD placed on families.
He [patient] cannot go out…His wife does everything…All he can do is to ask others [to do things]. So for his partner or caregiver, it may be a huge burden, economic burden. [GP3, FG4]
I am interested in photography …but this winter, I was very careful not to catch a cold…my children need to work, my husband is over 70…how could I trouble them? [P7, FG1]
Theme 2: Current management of COPD
Inhalers and lung function tests (LFTs) were rarely available in CHCs, so COPD was not assessed or treated locally. Therefore, GPs received minimal relevant training and lacked confidence in the management of COPD. A local LHS was deemed more effective if run alongside free COPD treatments and tests
We really hope to have medications recommended by guidelines…we have no medications to prescribe to patients so we do not know their effectiveness, which limits our ability to diagnose and provide treatment. [GP1, FG5]
Some doctors do not even know how to use the devices [inhalers] so GPs need education on COPD too. [GP9, FG2]
I think they would like to go to big hospitals, but I’m not sure if they would come here. If we can provide free medical tests, such as lung function tests, or pills, gifts, they will be more likely to come. [GP4, FG5]
Similarly, there were no smoking cessation clinics or cessation drugs in CHCs. While some GPs were happy to recommend specialist cessation advice, others doubted the efficacy of cessation drugs, believing that motivation and peer support were the most effective tools. These latter views were seen in patients too.
I do not know the effectiveness [of cessation drugs] …What if patients quit smoking but become addicted to smoking cessation drugs? [GP6, FG4]
If patients have no motivation to stop smoking, they will not follow advice from their doctors at all. However, if they have the motivation, you [doctors] only need to say a few words and then they quit. [GP2, FG1]
I do not want to use cessation drugs because relying on willpower is okay. But most people have not quit because they would change a lot after quitting…they will be fat once quit. (smoker) [P2, FG5]
Only a few patients visited the TCM department for COPD and held mixed opinions. A couple felt it was useless while another couple found it controlled phlegm well.
TCM has a drug called “Sanfu patch” [a kind of patch applied to acupuncture points], which is used to treat chronic bronchitis. I used it several times but it did not work. [P3, FG1]
I took TCM for nearly half a year and my phlegm stopped. [P14, FG2]
Theme 3: Lung Health Service Design
Subtheme 3.1: COPD education: GPs thought that patients were uninterested in knowing more about COPD, but actually, patients stated that they wanted to learn more
Our team organised several COPD talks this year but patients were not enthusiastic at all…It was because that they did not think COPD was important. [GP4, FG4]
When I visit the outpatient clinic, treatment is a secondary thing. I just want to consult [health information], listen to advice from doctors to improve my knowledge. [P13, FG2]
GPs were too busy to deliver COPD education, but thought nurses might be able to do so since they had more experience in this area. Both patients and GPs favoured a 1-hour session, once or twice a week.
Nurses might be more appropriate to give talks since they are more experienced in delivering education than doctors. [GP5, FG1]
Twice a week would be appropriate. Sometimes delivering talks on specific topics would be good, and sometimes interactions would be fine. [P7, FG4]
Some GPs suggested peer education as patients seemed to enjoy meeting with each other and exchanging experiences.
Some patients I meet would trust their neighbours more [compared with doctors]. When they first attend CHCs, you [GPs] may tell them a lot, but the effectiveness is not as good as what their neighbours said. [GP7, FG2]
WeChat, an extremely popular social media app in China, has potential for supporting patients.
During COVID-19 pandemic, it is not feasible to bring patients together so health education is mostly done online…Many people messaged me to say that this form is quite good. [GP4, FG3]
Patients with COPD could be in the same [WeChat] group to share our medications and experience in treating COPD. This would be great. [P2, FG5]
Subtheme 3.2: Exercise training: GPs were concerned about the risk of injuries from exercise training, and subsequent litigation so wanted written consent beforehand.
If we want to get PR to work, patients need to do intensive exercise, then there will be risks…patients’ written consent is insufficient, their children need to consent, too. [GP1, FG1]
Some GPs felt that they had insufficient time or knowledge to deliver exercise training so suggested specialists as an alternative. However, those with experience in teaching TaiChi were keen to receive more training so they could deliver this themselves.
If delivering PR in CHCs, the first problem would be personnel. We could not ask clinicians to do this because they are unable to do it well. I think we could recruit some rehabilitation doctors and physiotherapists. [GP5, FG3]
I advise patients to do TaiChi… A few days ago, we worked with the TCM Department to bring together a dozen COPD patients to do Liuzijue [a moderate-low intensity form of traditional Chinese exercise]…patients are happy to learn it and our medical staff need to do more [to be able to help them]. [GP1, FG4]
While patients with mild COPD were agreeable to the idea of strenuous exercise, others were not.
I think that I would become more breathless if taking exercise…Anyway, I cannot take strenuous exercise but mild exercise might be acceptable. [P3, FG5]
Chinese people are not as strong as foreigners and many elderly people have co-morbidities. [GP3, FG1]
Subtheme 3.3: Psychological support: There were mixed views about the management of psychological wellbeing. Some GPs and patients felt that better education about COPD would alleviate patient anxiety, while more formalised psychological support would need specialists.
I would not feel anxious if I understand the disease. [P9, FG5]
I think the best way is to let them understand that COPD can be prevented and controlled. Then they will not be worried anymore. [GP4, FG3]
I provided psychological counselling before, but it was not useful. I think it is better to provide psychological support from specialists. After all, I’m not good at that. [GP1, FG4]
Integration of the survey and FG findings can be seen in Supplementary Table 4.
Discussion
We found that participants did not fully understand the implications of COPD and how best to manage it. Current health service availability did not meet patients’ needs and for some was too costly. TCM was not as important to patients as expected. There was support for a LHS among both COPD patients and GPs, one tailored to meet Chinese patients’ needs, health beliefs and local healthcare delivery, e.g., type of exercise, patient led topics, user-friendly appointments and use of WeChat. Patients wanted a flexible service, GPs suggested that nurses and physiotherapists would be best placed to provide this. There were concerns about safe and acceptable levels of exercise; TaiChi and walking might be fitting alternatives to other forms of exercise. Psychological support was not considered necessary by patients or GPs.
This study used questionnaires and FGs to gather data from both patient and GP perspectives to inform the design of a flexible and culturally appropriate intervention. The triangulation of data from different methods enabled the team to access the perspectives of different groups, for instance, those with severe COPD were not able to participate in FGs, but were able to engage with the survey. The survey also offered anonymity for the research participants enabling the team to engage with challenging topics such as finance, whereas those in FGs denied any concerns about being able to afford their healthcare. Either this was a skewed sample or participants did not feel comfortable sharing financial difficulties. Recruitment sites represented different geographic areas of China, where exposure, lifestyle and the prevalence of COPD differed, enriching the data’s diversity.
There were some limitations to the study. In some cases, the research team felt that qualitative responses lacked depth or explanation, such as in the online FGs where patient participation was much lower than face-to-face, potentially due to unstable network connections and the mode of communication, or where facilitators were trained but not experienced in FG facilitation, so did not probe further. Study participants were limited to provincial capital cities, which may affect the external validity of the study. In addition, variable recall may have affected participants’ responses. In order to maximise diversity within the qualitative data we purposively sampled different kinds of people and analysed the data alongside collection to ensure data saturation, that is, the point at which no new themes were emerging31. A larger survey sample could potentially have provided the opportunity to examine whether the results differed by population subgroups.
In line with previous research3,35,36,37, we found that COPD was poorly understood by patients and that current management was sub-optimal with GPs having limited clinical skills in this area38. A potential solution suggested in studies from Europe, which is also emphasised in China’s recent government policies, is to develop postgraduate training programmes, which address the value of PR in supporting the management of COPD in primary care36,39,40.
A systematic review comparing PR programmes globally revealed that the current availability of PR services among individuals with COPD was less than 1.2%41. The importance of offering a flexible tailored service was highlighted, failure to do so may explain why some services experience low uptake13. In addition to providing user-friendly appointments, the use of novel modes of delivery and culturally acceptable elements are important factors - in 2019 1.15 billion users a month logged onto WeChat, a social media app popular in China42. This app is known to be effective in delivering health education, remote intervention and follow-up43,44,45,46,47,48. Favourable comments about WeChat’s potential for COPD education were made by both patients and GPs in our study. The poor inhaler technique identified in this study is a global issue with little improvement over the past 40 years49. Video applications used to monitor patients’ inhaler techniques at home have found that errors in technique start appearing as early as the first day after training50. WeChat might be a useful tool for improving inhaler technique.
In keeping with other studies in China and also America51,52, patients in our study were reluctant to take strenuous exercise due to shortness of breath, gentle exercise like TaiChi, QiGong and walking were considered more appropriate51. However, it should be recognised that they may not be as effective in building endurance and strength as other forms of exercise usually used in PR53,54,55,56,57,58. A new finding was GPs’ concern about litigation. These concerns may be explained by recent research in China reporting increasing litigation in medicine, some of which have resulted in, verbal or physical abuse towards doctors59,60.
These findings can be used to design a feasibility study testing a culturally appropriate LHS, including education on COPD, exercise, diet, oxygen therapy and medication use, which contrary to GP beliefs, patients are likely to be receptive to. The lack of lung function testing and COPD drugs in community health centres limits GPs’ ability to identify and therefore treat COPD locally, negatively impacting on their expertise in this area. Preliminary evidence demonstrates the ease with which this could be achieved within community settings in China61. If government policy regarding COPD is to be more effectively implemented these limitations need addressing. The burden imposed upon family members by patients’ exacerbations and hospitalisations also needs to be considered and addressed, similarly a review of healthcare costs could further improve COPD patients’ health. Further work could explore acceptability in rural locations, which was not directly addressed in this study. In addition to the issues regarding provision of PR services, not just in China, but globally41, uptake is also a factor. The suggestion in our study that this may be due to design issues, which do not meet local needs emphasises the benefits of studies like ours being conducted in other countries, as locally tailored, flexible LHS’s might be more culturally acceptable.
Overall, this study showed that participants did not fully understand the implications of COPD and current treatment was sub-optimal. There was support for developing a culturally appropriate intervention among COPD patients, one tailored to meet Chinese patients’ needs, health beliefs, and local healthcare delivery. TaiChi was suggested as an acceptable intervention with WeChat for social support. Further research is needed to explore the feasibility of such a service.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data supporting the findings of this study are available from the corresponding author upon written application and completion of appropriate data sharing agreements.
References
WHO. World Health Statistics 2017-Monitoring Health for the SDGs. http://www.indiaenvironmentportal.org.in/content/442747/world-health-statistics-2017-monitoring-health-for-the-sdgs/. (WHO, 2021) (accessed January 29, 2021).
Bi, Y. et al. Status of cardiovascular health in Chinese adults. J. Am. Coll. Cardiol. 65, 1013–1025 (2015).
Wang, C. et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 391, 1706–1717 (2018).
Zhu, B., Wang, Y., Ming, J., Chen, W. & Zhang, L. Disease burden of COPD in China: a systematic review. Int. J. Chron. Obstruct Pulmon. Dis. 13, 1353–1364 (2018).
Agusti, A. G. et al. 2021 Global Strategy for Prevention, Diagnosis and Management of COPD. https://goldcopd.org/2021-gold-reports/ (accessed January 29, 2021)
Wagg, K. Unravelling self-management for COPD: what next. Chron. Respir. Dis. 9, 5–7 (2012).
McCarthy, B. et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. CD003793 (2015).
Brooks, D., Lacasse, Y. & Goldstein, R. S. Pulmonary rehabilitation programs in Canada: national survey. Can. Respir. J. 6, 55–63 (1999).
Levack, W. M., Weatherall, M., Reeve, J. C., Mans, C. & Mauro, A. Uptake of pulmonary rehabilitation in New Zealand by people with chronic obstructive pulmonary disease in 2009. N. Z. Med. J. 125, 23–33 (2012).
Molin, K. R., Egerod, I., Valentiner, L. S., Lange, P. & Langberg, H. General practitioners’ perceptions of COPD treatment: thematic analysis of qualitative interviews. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 1929–1937 (2016).
Sandelowsky, H. et al. COPD management by Swedish general practitioners-baseline results of the PRIMAIR study. Scand. J. Prim. Health Care 36, 5–13 (2018).
Kurmi, O. P. et al. Patterns and management of chronic obstructive pulmonary disease in urban and rural China: a community-based survey of 25 000 adults across 10 regions. BMJ Open Respir. Res. 5, e000267 (2018).
Wong, C. K. & Yu, W. C. Correlates of disease-specific knowledge in Chinese patients with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 2221–2227 (2016).
Yan, R., Wang, Y., Bo, J. & Li, W. Healthy lifestyle behaviors among individuals with chronic obstructive pulmonary disease in urban and rural communities in China: a large community-based epidemiological study. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 3311–3321 (2017).
Li, D. & Zhu, S. Influencing factors of refusing pulmonary rehabilitation treatment for patients with COPD: a qualitative study. J. Nurs. Sci. 32, 6–9 (2017). (in Chinese).
Deng, R. et al. Difference in community rehabilitation compliance between urban and rural patients with COPD. Chin. Gen. Pract. 15, 2598–2600 (2012). (in Chinese).
Chan, K. P. et al. Adherence to a COPD treatment guideline among patients in Hong Kong. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 3371–3379 (2017).
Li, F. et al. The evaluation of general practitioners’ awareness/knowledge and adherence to the GOLD guidelines in a Shanghai suburb. Asia Pac. J. Public Health 27, NP2067–NP2078 (2015).
Chen, X., Jin, X., L, M., Li, S. & Zhu, H. Knowledge level about pulmonary rehabilitation: a questionnaire analysis in respiratory physicians in Shanghai. Chin. J. Respiratory Crit. Care Med. 11, 375–377 (2012). (in Chinese).
Gao, L. & Zhao, H. A nationwide online questionnaire survey of the understanding and implementation of pulmonary rehabilitation at all levels of medical institutions in China in 2017. Chin. J. Tuberculosis Respiratory Dis. 42, 275–278 (2019). (in Chinese).
Li, Y., Feng, J., Li, Y., Jia, W. & Qian, H. Assessment of a domiciliary integrated pulmonary rehabilitation program for patients with a history of acute exacerbation of chronic obstructive pulmonary disease: a retrospective 12-month observational study. Med. Sci. Monit. 24, 5054–5063 (2018).
Lou, P. et al. A COPD health management program in a community-based primary care setting: a randomized controlled trial. Respir. Care 60, 102–112 (2015).
Liu, T., Li, X., Zou, Z. Y. & Li, C. The prevalence and determinants of using traditional Chinese medicine among middle-aged and older Chinese adults: results from the china health and retirement longitudinal study. J. Am. Med. Dir. Assoc. 16, e1–e5 (2015). 1002.
Hyland, M. E., Jones, R. C. & Hanney, K. E. The lung information needs questionnaire: development, preliminary validation and findings. Respir. Med. 100, 1807–1816 (2006).
Bestall, J. C. et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54, 581–586 (1999).
Jones, P. W. et al. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 34, 648–654 (2009).
Amireault, S., Godin, G., Lacombe, J. & Sabiston, C. M. The use of the Godin-Shephard Leisure-Time Physical Activity Questionnaire in oncology research: a systematic review. BMC Med. Res. Methodol. 15, 60 (2015).
Harris, P. A. et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inf. 95, 103208 (2019).
Boston, R. C. & Sumner, A. E. STATA: a statistical analysis system for examining biomedical data. Adv. Exp. Med Biol. 537, 353–369 (2003).
Palinkas, L. A. et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health 42, 533–544 (2015).
Gale, N. K., Heath, G., Cameron, E., Rashid, S. & Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 13, 117 (2013).
Creswell, J. W., Fetters, M. D. & Ivankova, N. V. Designing a mixed methods study in primary care. Ann. Fam. Med. 2, 7–12 (2004).
Tashakkori A. & Teddlie C. Mixed Methodology: Combining Qualitative and Quantitative Approaches (Sage Publications, Inc, 1998).
Hu, H. et al. The investigation of health education and the treatment conditions in stable COPD patients in communitis of Chengdu. Natl. Med. Front. China 8, 117–118 (2013). (in Chinese).
Göktalay, T. et al. Knowledge level of the primary healthcare providers on chronic obstructive pulmonary disease and pulmonary rehabilitation. Pulm. Med. 2015, 538246 (2015).
Abrahamsen, C. S., Lang-Ree, H. M., Halvorsen, K. & Stenbakken, C. M. Patients with COPD: Exploring patients’ coping ability during an interdisciplinary pulmonary rehabilitation programme: a qualitative focus group study. J. Clin. Nurs. 30, 1479–1488 (2021).
Zeng, Y. et al. Current status of the treatment of COPD in China: a multicenter prospective observational study. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 3227–3237 (2020).
National Health Commission of the People’s Republic of China. Notice on implementation “China’s plan on the prevention and control of chronic disease (2012-2015)” http://www.nhc.gov.cn/wjw/gfxwj/201304/b8de7b7415ca4996b3567e5a09e43300.shtml. (accessed January 29, 2021; in Chinese).
National Health Commission of the People’s Republic of China. Notice on formulating tiered care system of chronic obstructive pulmonary disease. http://www.nhc.gov.cn/yzygj/s3594q/201702/50511229a68c41dda3c14cedfb92cdae.shtml (accessed January 29, 2021; in Chinese).
Desveaux, L., Janaudis-Ferreira, T., Goldstein, R. & Brooks, D. An international comparison of pulmonary rehabilitation: a systematic review. COPD 12, 144–153 (2015).
2019 WeChat Annual Data Report https://www.sohu.com/a/365785252_624184 (access in 21 Feb 2021; in Chinese).
Bi, J. et al. WeChat as a platform for Baduanjin intervention in patients with stable chronic obstructive pulmonary disease in China: retrospective randomized controlled trial. JMIR Mhealth Uhealth 9, e23548 (2021).
Guo, Y. et al. Effect of a WeChat-Based Intervention (Run4Love) on depressive symptoms among people living with HIV in China: a randomized controlled trial. J. Med. Internet Res. 22, e16715 (2020).
Liu, G. et al. The efficacy of WeChat-based parenting training on the psychological well-being of mothers with children with autism during the COVID-19 pandemic: quasi-experimental study. JMIR Ment. Health 8, e23917 (2021).
Zhang, Q., Xu, N., Huang, S., Chen, Q. & Cao, H. Effect of the use of wechat to disseminate preoperative health education to parents of children with restrictive ventricular septal defects: a prospective randomized controlled study. Heart Surg. Forum 23, E897–897.E901 (2020).
Zhang, Q. L. et al. Application of remote follow-up via the wechat platform for patients who underwent congenital cardiac surgery during the COVID-19 epidemic. Braz. J. Cardiovasc. Surg. 36, 530–534 (2020).
Deng, N. et al. Using mobile health technology to deliver a community-based closed-loop management system for chronic obstructive pulmonary disease patients in remote areas of china: development and prospective observational study. JMIR Mhealth Uhealth 8, e15978 (2020).
Sanchis, J., Gich, I. & Pedersen, S., Aerosol Drug Management Improvement Team (ADMIT). Systematic review of errors in inhaler use: has patient technique improved over time. Chest 150, 394–406 (2016)..
Dhadge, N. et al. Monitoring of inhaler use at home with a smartphone video application in a pilot study. NPJ Prim. Care Respir. Med. 30, 46 (2020).
Liu, Z., Speed, S. & Beaver, K. Perceptions and attitudes towards exercise among Chinese elders-the implications of culturally based self-management strategies for effective health-related help seeking and person-centred care. Health Expect. 18, 262–272 (2015).
Farris, S. G., Abrantes, A. M., Bond, D. S., Stabile, L. M. & Wu, W. C. Anxiety and fear of exercise in cardiopulmonary rehabilitation: patient and practitioner perspectives. J. Cardiopulm. Rehabil. Prev. 39, E9–E13 (2019).
Wu, W. et al. Effects of Tai Chi on exercise capacity and health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 1253–1263 (2014).
Polkey, M. I. et al. Tai Chi and pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest 153, 1116–1124 (2018).
Liu, X. et al. Home-based prescribed pulmonary exercise in patients with stable chronic obstructive pulmonary disease. J. Vis. Exp. https://doi.org/10.3791/59765 (2019).
Lewis, A. & Hopkinson, N. S. Tai Chi movements for wellbeing - evaluation of a British lung foundation pilot. Perspect. Public Health 140, 172–180 (2020).
Kantatong, T., Panpanich, R., Deesomchok, A., Sungkarat, S. & Siviroj, P. Effects of the tai chi qigong programme on functional capacity, and lung function in chronic obstructive pulmonary disease patients: a ramdomised controlled trial. J. Tradit. Complement Med. 10, 354–359 (2020).
Zhang, Y. P. et al. Evidence base of clinical studies on Qi Gong: a bibliometric analysis. Complement.Ther. Med. 50, 102392 (2020).
Wu, Y. et al. Experience of medical disputes, medical disturbances, verbal and physical violence, and burnout among physicians in China. Front. Psychol. 11, 556517 (2020).
Violence against doctors: Why China? Why now? What next. Lancet 383, 1013 (2014).
Pan, Z. et al. Study to evaluate the effectiveness and cost-effectiveness of different screening strategies for identifying undiagnosed COPD among residents (≥40 years) in four cities in China: protocol for a multicentre cross-sectional study on behalf of the Breathe Well group. BMJ Open 10, e035738 (2020).
Acknowledgements
We gratefully acknowledge: The IPCRG for introducing us to the primary care networks involved in this study and for its continued facilitation of clinical engagement. The trial steering and international scientific advisory committees: Zhiwei Zhang (patient), Xueying Zhou (clinician), Semira Manaseki-Holland, David Mannino, Debbie Jarvis and Niels Chavannes. All the participants, and staff of Xinjiekou CHC, Beijing; Beishi CHC, Shenyang; ShaYuan CHC, Guangzhou; Nanxin CHC, Chengdu and Xue Jin, Chang Gao from Peking University First Hospital. This research was funded by the National Institute for Health Research (NIHR) NIHR global group on global COPD in primary care, University of Birmingham, (project reference: 16/137/95) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
R.J., P.A., C.C., K.K.C., Z.P., X.K., B.C., J.C., A.D., A.E., A.F., N.G., K.J., S.J., M.M., T.M., S.M., A.S., K.S., R.S., A.T. and S.W. made substantial contributions to the study concept. E.D., Z.P. and H.P. designed the study and protocol with supervision from R.J., C.C., P.A., N.G., R.A. Data acquisition was undertaken by H.P., Z.P. and E.D., supervised by C.C. (China) and R.A. (UK). Data analysis was undertaken by H.P., Z.P. and E.D., supported by R.A., A.D. and N.G. H.P. wrote the initial draft of the paper, with support from Z.P., supervised by R.A. and N.G., and critical revisions made by all other authors. All authors have approved the final manuscript and are accountable for the work and its content. C.C. and R.J. are the study guarantors. We would like to acknowledge Radmila Ristovska (1955–2020), also involved in the initiation of this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pang, H., Pan, Z., Adams, R. et al. Community lung health service design for COPD patients in China by the Breathe Well group. npj Prim. Care Respir. Med. 32, 27 (2022). https://doi.org/10.1038/s41533-022-00286-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-022-00286-8