Abstract
The aim of this observational, retrospective study was to describe characteristics, treatment patterns, and adherence among patients with asthma who initiated multiple-inhaler triple therapy (MITT) in Catalonia, Spain. This study used data of patients initiating MITT in 2016 from the SIDIAP (Information System for Research in Primary Care) database, which covers ~80% of the Catalonian population (5.8 million). Of 1,204 patients initiating MITT, 361 (30.0%) stepped down (discontinued ≥ 1 and continued ≥1 MITT component) and 89 (7.4%) stopped all three components of MITT for a period of 60 days during the following 12 months. In the follow-up period, 196 (16.3%) patients were considered adherent to MITT (>0.8 proportion of days covered [PDC]), with a mean (standard deviation) PDC of 0.52 (0.51) days. Given the low adherence and substantial rates of step down/discontinuation among patients initiating MITT, there is an urgent need to implement strategies to improve treatment adherence/persistence.
Similar content being viewed by others
Introduction
Asthma is a heterogeneous chronic inflammatory respiratory disease that is often both over- and underdiagnosed1,2,3. From 1990 to 2015, the prevalence of asthma increased by 12.6% globally, with over 358 million people worldwide suffering from asthma in 20154. Prevalence rates vary significantly between countries or even between regions of the same country, with the prevalence rate in Spain estimated to be between 2.5 and 13.5% overall, and the prevalence in Barcelona reported to be 6.3–6.6%5,6,7.
Between 30 and 50% of patients with moderate/severe asthma have inadequately controlled disease despite attempts to optimize adherence to inhaled corticosteroids in combination with a long-acting β2-agonist (ICS/LABA)8,9,10,11,12. In an observational, cross-sectional study conducted in Spain, the prevalence of uncontrolled severe persistent asthma among patients with asthma seen at pneumology and allergology hospital units based on a physician’s diagnosis was 3.9% (N = 36,649). Furthermore, the level of asthma control was shown to be underestimated by physicians, which may reflect issues with adopting and implementing treatment guidelines in clinical practice13. The most common treatments recommended for both moderate/severe asthma and uncontrolled severe persistent asthma are ICS/LABA alone or in combination with a short-acting β2-agonist (SABA) or a leukotriene receptor antagonist13. The Global Initiative for Asthma (GINA) also recommends adding long-acting muscarinic antagonists (LAMA) as an additional controller for patients with uncontrolled asthma on at least medium-dose ICS/LABA therapy2. The addition of a LAMA to ICS/LABA maintenance therapy as part of a multiple-inhaler triple therapy (MITT) regimen14 or, more recently, as single-inhaler triple therapy (SITT) has been shown to improve lung function and reduce exacerbation rates in patients with uncontrolled asthma15,16,17. These data indicate that escalation to triple therapy (ICS/LABA/LAMA) may benefit patients on ICS/LABA with uncontrolled asthma.
The use of multiple inhalers as dual therapy in asthma is associated with lower adherence rates, lower medication persistence, increased asthma-related symptoms, and increased hospitalization compared with single-inhaler dual therapy18,19. Currently, there is limited real-world data regarding demographics, clinical characteristics, treatment patterns, discontinuation, and adherence of patients with asthma initiating MITT in Europe. Therefore, the aim of this study was to describe the characteristics of patients with asthma who initiate MITT, treatment patterns before and after MITT initiation, and treatment adherence to MITT in Catalonia, Spain.
Method
Study design
This epidemiological study with retrospective analysis of longitudinal follow-up data used the SIDIAP database, which contains anonymized electronic patient records for 5.8 million people registered in 279 primary care centers of the Catalan Health Institute and covers approximately 80% of the population of Catalonia20. The SIDIAP database contains information on patient demographics and medical records from 2006. Additionally, the SIDIAP is linked to registers or databases that provide information regarding hospitalizations, medication prescribed in pharmacies within the Catalan Health Institute hospitals (Pharmacy Register), and mortality (National Mortality Register).
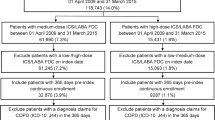
Patients initiating MITT were identified from January 1st to December 31st, 2016. The index date was the date of initiation of the third component of MITT, defined as overlapping prescriptions for ICS, LABA, and LAMA (in two or three devices) for ≥60 days (Fig. 1). Data were collected for the 12 months prior to (pre-index) and 12 months following (post-index) the index date.
Study population
Patients included in this study were aged 18–75 years with at least one protocol-defined ICD 10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification21) asthma medical code, an overlapping prescription of at least 60 days for each of the three components of MITT during the study inclusion period, and available medical records in the SIDIAP database pre- and post-index.
Patients were excluded if they had a diagnosis of COPD (including emphysema and chronic bronchitis), cystic fibrosis, heart failure, or lung cancer at any time in their medical records, or had used MITT or LAMA monotherapy pre-index (to ensure exclusion of patients with COPD incorrectly classified as having asthma).
Study endpoints
The primary objective of the study was to describe the demographics, comorbidities, clinical characteristics, and treatment patterns in the overall study population pre- and post-index.
The secondary objectives were to describe discontinuation of MITT post-index (including the number of patients discontinuing and the number of patients stepping down and subsequent treatment patterns); describe patient characteristics according to MITT persistence or discontinuation post-index; describe the characteristics and treatment patterns of patients who experienced severe exacerbations pre-index; to describe treatment adherence in patients on MITT post-index, and to describe characteristics and treatment patterns in patients who discontinued MITT according to the timing of discontinuation (first 90 days or Days 181–364).
Three different MITT treatment patterns were assessed post-index: persistence on MITT; step down from MITT; and discontinuation of MITT. Persistence on MITT included patients who did not discontinue and did not step down; step down from MITT included patients who discontinued at least one of the three MITT components but continued to be prescribed at least one component; and discontinuation of MITT included patients who experienced a 60-day gap in subsequent prescriptions for all three components (i.e., ICS, LABA, LAMA). The rationale of using a 60-day gap to define discontinuation was based on requirements of the healthcare system in Catalonia where regular prescription of inhaled therapies by clinicians lasts for 2 months; after 2 months it is mandatory for the physician to renew or modify the prescription. The date of step down or discontinuation was defined as the last date of overlapping prescription of ICS, LABA, and LAMA.
Outcomes
Demographics, comorbidities, and clinical characteristics including lung function (FEV1 % predicted value and FEV1/FVC ratio), the percentage of eosinophils in peripheral blood, severe exacerbations, and treatments patterns were identified from the SIDIAP database pre- and post-index. Severe exacerbations were defined as the need for one hospitalization or emergency visit or the use of oral/systemic corticosteroids (or increase in the maintenance dose) for ≥3 days due to asthma, and were captured by the Catalan Health Institute hospitals. Additional outcomes assessed post-index included adherence to MITT, defined as the extent to which a patient acts in accordance with the prescribed interval and dose of a dosing regimen. In this study, treatment adherence was assessed in terms of PDC.
Sample size and statistical analysis
All patients in the SIDIAP registry (~5.8 million people) who met the eligibility criteria were included in the study. Based on an estimated asthma prevalence of 3% in Spain, a sample size of 1,117 patients was considered to be sufficient to address the main study objective with a 95% CI. For patients who discontinued MITT, assuming a 95% CI in a two-sided test, 195 patients in each group (discontinued or not discontinued) were sufficient to find statistically significant differences with a minimum statistical power of 80%.
Continuous variables are reported as a mean and SD and categorical variables are presented as number and percentage of patients. For spirometry data, paired analyses (when available) for a small subgroup of patients are presented.
MITT discontinuation was calculated based on the number of patients who discontinued treatment in relation to the total number of patients in the 12 months pre-index date.
Adherence to MITT was calculated according to the number of adherent patients in relation to the total number of patients in the 12 months post-index date. PDC was calculated during the 12-month post-index period by dividing the total number of days that MITT was prescribed by the number of days post-index and ranged from 0 to 1. A patient was considered adherent when the PDC value was >0.8.
A logistic regression model was developed to identify independent factors associated with adherence to and discontinuation of MITT. The Hosmer–Lemeshow test22 was used and independent variables were age, sex, BMI, smoking status, comorbidities (pneumonia, sleep apnea syndrome, polyposis, allergic rhinitis, atopic dermatitis, conjunctivitis, gastroesophageal reflux, diabetes mellitus, hypertension, anxiety, depression), exacerbations, eosinophil count, chest X-ray, computerized tomography scan, allergy test, GP, nurse and pulmonologist visits, pneumologist and allergy referrals, sick leave, sick leave due to a respiratory cause, influenza and pneumococcal vaccines, and previous treatment (ICS, ICS/LABA, ICS/LABA/anti-leukotrienes, ICS/LABA/OCS/anti-leukotrienes, ICS/LAMA, LAMA, LABA/LAMA, LAMA/anti-leukotrienes, anti-leukotrienes, OCS, no treatment). Adherence to MITT refers to the collection of over 80% of the prescribed treatment from pharmacies, whereas discontinuation refers to not having a prescription renewal by the doctor. Analyses were performed using the R (version 3.3.2) statistical package. For statistical tests performed with the outcome variables, a significance level of 0.05 was used, with no adjustments for multiplicity.
Results
Characteristics and treatment patterns pre- and post-index
Details of patient selection from the Information System for Research in Primary Care (SIDIAP) database are summarized in Fig. 2. Of 1,204 patients included in this study, 851 (70.7%) were female and the mean (standard deviation [SD]) age at MITT initiation was 54.8 (13.8) years (Table 1). Body mass index (BMI), smoking status, and percentage of eosinophils measured in peripheral blood were comparable pre- and post-index (Table 1). Mean (SD) forced expiratory volume in 1 s (FEV1) % predicted was 70.8 (19.1) pre-index and 75.4 (19.6) post-index (Table 1). Among the 1,204 patients included, 881 (73.2%) had previously been receiving ICS/LABA and 162 (13.5%) were not receiving any treatment (Fig. 3).
Percentages may not total 100% due to rounding. *ICS/LABA category includes: ICS/LABA, ICS/LABA/anti-leukotrienes, ICS/LABA/OCS, ICS/LABA/OCS/SAMA, ICS/LABA/anti-leukotrienes/OCS; †other category includes: ICS, ICS/LAMA, ICS/anti-leukotrienes, ICS/OCS, ICS/OCS/LAMA, LABA/LAMA, LABA/anti-leukotrienes, LAMA, LAMA/anti-leukotrienes, anti-leukotrienes, OCS, OCS/LAMA, OCS/LAMA/anti-leukotrienes. ICS inhaled corticosteroid, LABA long-acting β2-agonist, LAMA long-acting muscarinic antagonist, MITT multiple-inhaler triple therapy, OCS oral corticosteroid, SABA short-acting β2-agonist, SAMA short-acting muscarinic antagonist.
Patients stepping down and discontinuing MITT and subsequent treatments
Among the patients that initiated MITT, 754 (62.6%) persisted with MITT, 361 (30.0%) stepped down (discontinued ≥ 1 and continued ≥1 MITT component) and 89 (7.4%) discontinued MITT (stopped all three components of MITT for a period of 60 days) during the following 12 months. During the pre-index period, 589 (78.1%) patients who persisted with MITT, 257 (71.2%) who stepped down and 35 (39.3%) who discontinued MITT were on ICS/LABA (Fig. 4a). During the post-index period, among the patients that stepped down, 305 (84.5%) were on ICS/LABA and, of the patients that discontinued MITT completely, 61 (68.5%) were not treated and 18 (20.2%) were receiving treatment with SABA or SAMA (Fig. 4b).
a 12 months prior to (pre-index) and b 12 months following (post-index) MITT initiation. Percentages may not total 100% due to rounding. *ICS/LABA category includes: ICS/LABA, ICS/LABA/anti-leukotrienes, ICS/LABA/OCS, ICS/LABA/OCS/SAMA, ICS/LABA/anti-leukotrienes/OCS; †other category includes: ICS, ICS/LAMA, ICS/anti-leukotrienes, ICS/OCS, ICS/OCS/LAMA, LABA/LAMA, LABA/anti-leukotrienes, LAMA, LAMA/anti-leukotrienes, anti-leukotrienes, OCS, OCS/LAMA, OCS/LAMA/anti-leukotrienes. ICS inhaled corticosteroid, LABA long-acting β2-agonist, LAMA long-acting muscarinic antagonist, MITT multiple-inhaler triple therapy, OCS oral corticosteroid, SABA short-acting β2-agonist, SAMA short-acting muscarinic antagonist.
There were no clinically relevant differences between patients that stepped down or discontinued MITT compared with those who persisted in terms of age, BMI, or smoking status pre-index (Table 2) and post-index (Supplementary Table 1). Patients who persisted with MITT had similar FEV1 % predicted value and mean FEV1/forced vital capacity (FVC) ratio pre-index (Table 2) and post-index (Supplementary Table 1) compared with patients who did not maintain MITT. Additionally, in patients who discontinued treatment, the mean (SD) percentage of eosinophils measured in peripheral blood post-index was lower (3.2% [2.0]) compared with patients who persisted (4.0% [3.2]) or stepped down (4.4% [3.0]) from MITT (Supplementary Table 1). Prior to MITT initiation, the percentage of patients experiencing severe exacerbations was similar in patients who persisted, stepped down, or discontinued MITT (55.8% vs 55.1% and 52.8%, respectively) (Table 2).
Demographics, clinical characteristics, and treatment patterns were generally similar across patients that stopped MITT in the first 90 days (Supplementary Table 2) and those who stopped between Days 181–364 (Supplementary Table 3).
Characteristics and treatment patterns of patients who experienced severe exacerbations during the 12 months prior to MITT initiation
In the pre-index period, 667 (55.4%) patients experienced at least one severe exacerbation compared with 503 (41.8%) patients post-index (Table 1). Among the patients who experienced severe exacerbations prior to initiation of MITT, 491 (73.6%) were female with a mean (SD) age at asthma diagnosis of 45.4 (15.8) years and a mean (SD) BMI of 30.4 (6.4) kg/m2 (Table 3). Additionally, post-index, 352 (52.8%) patients in this subgroup experienced a severe exacerbation. There was no change in the percentage of eosinophils measured in peripheral blood prior to and following MITT initiation (Table 3). Prior to MITT, 494 (74.1%) patients were previously treated with ICS/LABA and 80 (12.0%) patients received no treatment (Fig. 5). Post-index, 169 (25.3%) patients received ICS/LABA and 29 (4.3%) patients did not receive any treatment (Fig. 5).
Percentages may not total 100% due to rounding. *ICS/LABA category includes: ICS/LABA, ICS/LABA/anti-leukotrienes, ICS/LABA/OCS, ICS/LABA/OCS/SAMA, ICS/LABA/anti-leukotrienes/OCS; †other category includes: ICS, ICS/LAMA, ICS/anti-leukotrienes, ICS/OCS, ICS/OCS/LAMA, LABA/LAMA, LABA/anti-leukotrienes, LAMA, LAMA/anti-leukotrienes, anti-leukotrienes, OCS, OCS/LAMA, OCS/LAMA/anti-leukotrienes. ICS inhaled corticosteroid, LABA long-acting β2-agonist, LAMA long-acting muscarinic antagonist, MITT multiple-inhaler triple therapy, OCS oral corticosteroid, SABA short-acting β2-agonist, SAMA short acting muscarinic antagonist.
Adherence to MITT: Independent factors associated with adherence and discontinuation, and patient characteristics
Adherence to MITT was assessed using proportion of days covered (PDC), which was calculated as follows: PDC = total days all drugs available/days post-index. A patient was considered adherent when PDC was >0.8.
In the 12 months post-index, 196 (16.3%) patients were adherent to MITT and the mean (SD) PDC was 0.52 (0.51) days. The logistic regression model showed that greater adherence was associated with having anxiety and depression, taking sick leave due to a respiratory cause, and no previous ICS/LABA treatment prior to initiation of MITT (Table 4). Although older age at MITT initiation showed a significant association with greater adherence, the odds ratio was only marginally above 1.0 (1.047; 95% confidence interval [CI]: 1.025–1.070) (Table 4).
The proportion of patients who were current smokers and those experiencing a severe exacerbation was higher in adherent patients compared with non-adherent patients, whereas the percentage of eosinophils in peripheral blood was slightly higher in non-adherent versus adherent patients (Supplementary Table 4). Being male, not receiving a previous allergy test, or no previous treatment prior to initiation of MITT were all associated with discontinuation of MITT (Supplementary Table 5). Anxiety/depression was marginally but non-significantly (p = 0.052) associated with discontinuation of MITT (OR [95% CI]: 1.562 [0.996–2.448]).
Discussion
This retrospective observational study analyzed characteristics and treatment patterns of 1,204 patients with asthma initiating MITT in Catalonia, Spain. Overall, while persistence rates were relatively high, the rates of step down and discontinuation of MITT were also high, and adherence was poor. Most of the patients who initiated MITT during the study period were on ICS/LABA prior to index date, while 13% were untreated. In the 12 months after initiating MITT, 63% of patients persisted on MITT, 30% stepped down and 7% discontinued MITT. The proportion of adherent patients (>0.8 PDC) was only 16%; being older, having anxiety and/or depression, taking sick leave due to respiratory symptoms, and no previous treatment with ICS/LABA prior to initiation of MITT were all associated with greater adherence to treatment.
In our study, the unexpected finding that 14% of patients were not receiving any treatment prior to initiation of MITT could perhaps be attributed to a late diagnosis of severe asthma or a failure of physicians to adhere to guideline recommendations leading to potential overtreatment. Additionally, the high rates of treatment discontinuation/stepping down might be associated with both physician behavior (e.g., justified discontinuation/step-down due to lack of symptom control) and patient behavior (e.g., missed GP appointments, having a prescription but not filling it, and difficulties using multiple inhalers).
Suzuki et al published a similar observational cohort study in patients with asthma and asthma/chronic obstructive pulmonary disease (COPD) overlap who initiated triple therapy in Japan23. Persistence rates among patients with asthma were lower than those reported here (38.5% over 12 months)23. Furthermore, in our study, most patients (73%) initiating MITT were on ICS/LABA prior to the index date, compared with nearly 100% of patients in the observational study in Japan23. However, the sample size was much smaller. Studies on COPD using data from the SIDIAP database used in this study showed that 16.5% of patients initiated triple therapy 1 year after diagnosis24, and reported similar persistence rates with 62.5% of patients continuing to receive MITT 12 months following MITT initiation 25.
The benefits of initiating triple therapy on lung function, symptoms, and asthma control in patients with uncontrolled asthma have been demonstrated in multiple studies14,15,16,17. This study was not designed to determine any change in clinical outcomes before and after MITT initiation; however, a reduction in the number of patients experiencing a severe exacerbation was seen in the 12 months following MITT initiation compared with the previous 12 months (55.4 and 41.8% of patients, respectively). A reduction was observed in the aforementioned Japanese study (64.0% vs 45.8%)23. Interestingly, in our study, a greater reduction was observed in the subgroup of patients that had a severe exacerbation in the 12 months prior to MITT, with MITT reducing the number of patients experiencing exacerbations by half.
Triple therapy with ICS/LABA plus tiotropium has been shown to improve lung function and reduce the risk of exacerbations in patients with asthma26; however, the addition of tiotropium requires the use of multiple inhalers with different dosing regimens14. More recently, the TRIMARAN, TRIGGER, CAPTAIN, and IRIDIUM studies15,16,17 evaluated the efficacy and safety of various triple ICS/LABA/LAMA combinations administered via single inhalers. These studies demonstrated favorable effects on asthma clinical and patient-reported outcomes with no new safety concerns15,16,17. Observed differences between these studies (e.g., on asthma exacerbations) were likely due to differences in study populations and outcome definitions used 27.
Adherence to therapy is complex and it is influenced by interdependent factors related to the patient, the healthcare provider, and the healthcare system. In Spain, low adherence rates to triple therapy in COPD have been associated with high costs to the Spanish National Health System28. In this study, adherence to triple therapy in the 12 months following MITT initiation was 16.3% and the mean (SD) PDC was 0.52 (0.51) days. A similar low adherence rate was reported in the Japanese study discussed previously with a PDC of 0.51 in the asthma-only group as well as in the asthma-COPD overlap group23. It has been reported that persistence and adherence rates are lower when using multiple inhalers versus single-inhaler dual therapy in both asthma and COPD18,28,29. While the reasons for poor adherence in this study are unknown, possible explanations include the high cost of asthma medications and requirements for copayments (even in publicly funded healthcare systems such as in Spain), lack of patient understanding/awareness, limited supervision, or follow-up with a healthcare professional, lack of awareness of disease severity, and complexities for patients and for caregivers in using multiple inhalers with different dosing regimens (e.g., once vs twice daily)30,31,32,33. Additionally, an observational study conducted in Australia showed that over 80% of patients stepped-up to GINA Step 5 therapies while showing poor adherence to ICS/LABA34. Based on this, further analyses to determine the PDC before initiation of MITT might give important insights into the low adherence rates reported here. Notably, although adherence to MITT was low in this study, most patients (62.6%) persisted on MITT, which may indicate that patients experienced benefits on triple therapy. Nonetheless, the poor adherence rates we observed highlight a need for improvement. Offering SITT could benefit these patients and improve adherence. Interestingly, in this study greater adherence was associated with having anxiety and/or depression, taking sick leave due to a respiratory cause, and no previous ICS/LABA treatment. Studies have shown that treatment adherence tends to be higher among patients with uncontrolled and severe asthma35,36. The fact that taking sick leave was associated with higher adherence may indicate that patients in this study were perhaps more symptomatic or perceived their asthma as severe.
Strengths of our study include the large sample size, good representation of the population, and lack of a recall bias as this is a database study. However, as this was an observational retrospective study, it has inherent limitations including under-reporting of exacerbations, miscoding biases, and invalid/unknown data. To mitigate the impact of invalid/unknown data, we have used a range of diagnostic codes that delimited the study disease. Finally, spirometry and blood eosinophil data were limited due to the small number of patients with available data.
Overall, results from this study in patients with asthma initiating MITT showed that a significant proportion of patients step down, discontinue MITT, and are poorly adherent during the first 12 months of treatment. The poor adherence and substantial rates of step down/discontinuation we observed in this study, highlights an urgent need to implement strategies to improve treatment adherence. Addressing factors such as accuracy of diagnosis, inhaler technique, complexity of dosing regimens, and regularly checking treatment adherence in patients currently on ICS/LABA prior to initiating MITT may all be beneficial.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study belong to the Catalan Healthcare. System and are not publicly available. Anonymised individual participant data and study documents can be requested for further research from www.clinicalstudydatarequest.com.
References
Kavanagh, J., Jackson, D. J. & Kent, B. D. Over- and under-diagnosis in asthma. Breathe 15, e20–e27 (2019).
GINA. Global Strategy for Asthma Management and Prevention, www.ginasthma.org (2021).
Aaron, S. D. et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA 317, 269–279 (2017).
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 5, 691–706 (2017).
5.0., G. Guía Española para el Manejo del Asma (2020), https://www.gemasma.com (2020).
Morell, F. et al. La población de asmáticos ambulatorios y su control tras adaptar el tratamiento a las recomendaciones internacionales (ASMACAP I). Arch. Bronconeumol. 43, 29–35 (2007).
To, T. et al. Global asthma prevalence in adults: Findings from the cross-sectional world health survey. BMC Public Health 12, 204 (2012).
Bateman, E. D. et al. Global Initiative for Asthma 2016-derived asthma control with fluticasone propionate and salmeterol: A Gaining Optimal Asthma Control (GOAL) study reanalysis. Ann. Allergy Asthma Immunol. 123, 57–63 e52 (2019).
Bernstein, D. I. et al. Fluticasone furoate (FF)/vilanterol (100/25 mcg or 200/25 mcg) or FF (100 mcg) in persistent asthma. J. Asthma 52, 1073–1083 (2015).
Lee, L. K., Obi, E., Paknis, B., Kavati, A. & Chipps, B. Asthma control and disease burden in patients with asthma and allergic comorbidities. J. Asthma 55, 208–219 (2018).
Sulaiman, I. et al. A randomised clinical trial of feedback on inhaler adherence and technique in patients with severe uncontrolled asthma. Eur. Respir. J. https://doi.org/10.1183/13993003.01126-2017 (2018).
David, J., Trudo, F., Sidall, J. & Small, M. Burden of asthma among patients adherent to ICS/LABA: A real-world study. J. Asthma 56, 332–340 (2019).
Quirce, S., Plaza, V., Picado, C., Vennera, M. & Casafont, J. Prevalence of uncontrolled severe persistent asthma in pneumology and allergy hospital units in Spain. J. Investig. Allergol. Clin. Immunol. 21, 466–471 (2011).
Kerstjens, H. A. et al. Tiotropium in asthma poorly controlled with standard combination therapy. N. Engl. J. Med. 367, 1198–1207 (2012).
Virchow, J. C. et al. Single inhaler extrafine triple therapy in uncontrolled asthma (TRIMARAN and TRIGGER): Two double-blind, parallel-group, randomised, controlled phase 3 trials. Lancet 394, 1737–1749 (2019).
Kerstjens, H. A. M. et al. Once-daily, single-inhaler mometasone-indacaterol-glycopyrronium versus mometasone-indacaterol or twice-daily fluticasone-salmeterol in patients with inadequately controlled asthma (IRIDIUM): A randomised, double-blind, controlled phase 3 study. Lancet Respir. Med. 8, 1000–1012 (2020).
Lee, L. A. et al. Efficacy and safety of once-daily single-inhaler triple therapy (FF/UMEC/VI) versus FF/VI in patients with inadequately controlled asthma (CAPTAIN): A double-blind, randomised, phase 3A trial. Lancet Respir. Med. 9, 69–84 (2020).
Stempel, D. A. et al. Adherence to asthma controller medication regimens. Respir. Med. 99, 1263–1267 (2005).
O’Connor, R. D. et al. Asthma-related exacerbations, therapy switching, and therapy discontinuation: a comparison of 3 commonly used controller regimens. Ann. Allergy Asthma Immunol. 95, 535–540 (2005).
Bolibar, B. et al. SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. Med. Clin. 138, 617–621 (2012).
CMS. 2020 ICD-10-CM Coding Guidelines, https://www.cms.gov/Medicare/Coding/ICD10/2020-ICD-10-CM (2020).
Fagerland, M. W., Hosmer, D. W. & Bofin, A. M. Multinomial goodness-of-fit tests for logistic regression models. Stat. Med. 27, 4238–4253 (2008).
Suzuki, T., Fairburn-Beech, J., Sato, K. & Kaise, T. Clinical characteristics, treatment patterns, disease burden, and persistence/adherence in patients with asthma initiating inhaled triple therapy: Real-world evidence from Japan. Curr. Med. Res. Opin. 36, 1049–1057 (2020).
Monteagudo, M. et al. Clinical characteristics and factors associated with triple therapy use in newly diagnosed patients with COPD. NPJ Prim. Care Respir. Med. 31, 16 (2021).
Monteagudo, M. et al. Treatment pathways before and after triple therapy in COPD: A population-based study in primary care in Spain. Arch. Bronconeumol. 57, 205–213 (2021).
Singh, D. et al. Determinants of response to inhaled extrafine triple therapy in asthma: Analyses of TRIMARAN and TRIGGER. Respir. Res. 21, 285 (2020).
Ojanguren, I. & Pilia, M. F. Efficacy and safety of once-daily single-inhaler triple therapy in patients with inadequately controlled asthma: The CAPTAIN trial. Breathe 17, 200279 (2021).
Miravitlles, M. et al. Estimation of the clinical and economic impact of an improvement in adherence based on the use of once-daily single-inhaler triple therapy in patients with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 1643–1654 (2020).
Stoloff, S. W., Stempel, D. A., Meyer, J., Stanford, R. H. & Carranza Rosenzweig, J. R. Improved refill persistence with fluticasone propionate and salmeterol in a single inhaler compared with other controller therapies. J. Allergy Clin. Immunol. 113, 245–251 (2004).
Rodriguez-Garcia, C., Lourido-Cebreiro, T. & Gonzalez-Barcala, F. J. The ATAUD Study: The need to improve adherence. Arch. Bronconeumol. 55, 509–510 (2019).
Laba, T. L. et al. Cost-related underuse of medicines for asthma-opportunities for improving adherence. J. Allergy Clin. Immunol. Pr. 7, 2298–2306 e2212 (2019).
Melero Moreno, C., Quirce, S., Huerta, A., Uria, E. & Cuesta, M. Economic impact of severe asthma in Spain: multicentre observational longitudinal study. J. Asthma 56, 861–871 (2019).
Martinez-Moragon, E. et al. Economic cost of treating the patient with asthma in Spain: The AsmaCost study. Arch. Bronconeumol. 45, 481–486 (2009).
van Boven, J. F. M. et al. Trajectory analyses of adherence patterns in a real-life moderate to severe asthma population. J. Allergy Clin. Immunol. Pr. 8, 1961–1969 e1966 (2020).
Gon, Y., Ohyanagi, N. & Kobayashi, A. The association between control level and self-reported treatment adherence across different treatment types in Japanese asthma patients. Respir. Investig. https://doi.org/10.1016/j.resinv.2021.02.003 (2021).
Souza-Machado, A., Santos, P. M. & Cruz, A. A. Adherence to treatment in severe asthma: Predicting factors in a program for asthma control in Brazil. World Allergy Organ J. 3, 48–52 (2010).
Acknowledgements
This study was funded by GlaxoSmithKline (GSK; HO-18-18550). Editorial support (in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing, and referencing) was provided by Lucia Correia and Chloe Stevenson, of Fishawack Indicia Ltd, UK, part of Fishawack Health, and was funded by GSK.
Author information
Authors and Affiliations
Contributions
M. Monteagudo contributed to the conception/design of the study, acquisition of data, and data analysis/ interpretation. I.O. and M.B. contributed to conception/design of the study, and data analysis/interpretation. M. Miravitlles, X.F., J.O., A.N., and X.M. contributed to data analysis/interpretation. All authors were involved in the preparation and review of the manuscript and approved the final version to be submitted. All authors take complete responsibility for the integrity of the data and accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
I.O. has received travel grants, consulting fees, speaking fees or research grants from AstraZeneca, Bial, Boehringer Ingelheim, Chiesi, GSK, Mundipharma, Novartis, Teva, Sanofi, MSD and Puretech; I.O. is a researcher supported by the “Pla Estratègic de Recerca i Innovació en Salut PERIS)” 2016–2020 (SLT008/18/00108;G60594009). M.B. has received speaker fees from CSL Behring, Grifols, Menarini, GSK and Boehringer Ingelheim, consulting fees from GSK, Novartis and Boehringer Ingelheim. X.M. has received fees as a speaker, scientific advisor, or participant of clinical studies from AstraZeneca, Boehringer Ingelheim, Chiesi, Faes, GSK, Menarini, Mundipharma, Novartis, and Teva. M. Miravitlles has received speaker fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Menarini, Rovi, Bial, Zambon, CSL Behring, Grifols and Novartis, consulting fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GSK, Bial, Gebro Pharma, CSL Behring, Laboratorios Esteve, Ferrer, Mereo Biopharma, Verona Pharma, Teva, pH Pharma, Novartis and Grifols and research grants from Grifols. X.F. has received speaking fees from AstraZeneca, Chiesi, GSK, Mundipharma and Teva. M. Monteagudo, A.N., and J.O. declare no competing interests.
Ethical approval and informed consent
The study was conducted in compliance with local legislation for observational trials and it was approved by the IDIAP Jordi Gol Clinical Research Ethics Committee. As this is an observational study based on a database that uses anonymised patient records, patient informed consent is not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barrecheguren, M., Monteagudo, M., Miravitlles, M. et al. Characteristics and treatment patterns of patients with asthma on multiple-inhaler triple therapy in Spain. npj Prim. Care Respir. Med. 32, 11 (2022). https://doi.org/10.1038/s41533-022-00270-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-022-00270-2