Abstract
Primary care centers are ideal positions to identify chronic obstructive pulmonary disease (COPD). We determined the COPD prevalence among ever-smokers aged 40–65 years attending a 2-year program conducted in 22 Greek primary healthcare centers and made comparisons between genders, patients less than or greater than 55 years, and newly or previously diagnosed COPD patients. A total of 117 persons, after studying 1100 people, were diagnosed with previously unknown or known COPD, providing a COPD prevalence of 10.6% among the study population. In all, 7.5% of the participants were newly diagnosed with COPD. Women with COPD reported smoking less but experienced worse respiratory and depressive symptoms than men. A total of 19% of the COPD population below 55 years experienced wheezing and exacerbations more frequently than older patients. Newly diagnosed COPD patients were significantly younger, reported a significant burden of symptoms without seeking medical help. Primary health care has a crucial role in the early detection of COPD among unsuspecting smokers.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive chronic lung disease characterized by irreversible airflow obstruction1. COPD is already the third most common cause of adult mortality, something that the World Health Organization had not predicted to occur until 2030, and a leading cause of adult hospitalization globally2. Cigarette smoking is recognized as the leading cause of the disease. A total of 10–20% of smokers develop clinically significant COPD1. Importantly, the prevalence of COPD has increased in women, as the prevalence of smoking habit in females has grown progressively1.
There is a linear increase in COPD prevalence with patients’ age, suggesting that changes related to aging may contribute to COPD pathogenesis. Although COPD occurs most often in older adults, it can also affect people under 65 years old3. It has been reported that 44% of COPD patients are below the retirement age of 62 in the United Kingdom4. A subgroup of smokers appears particularly vulnerable to tobacco smoke and develops COPD in their early years5.
Greece has been suffering a high burden of COPD, although the reported prevalence rates are lower than expected when the high smoking rates in the country among European Union states are taken into account. An increasing COPD prevalence rate of up to 18.2% is apparent within the past 10 years in Greece6,7. COPD patients in Greece had a mean age between 60 and 70 years when first diagnosed according to studies that were conducted in the pre- and post-crisis periods6,7,8.
Since the radical cure is not clear for COPD, prevention is better than therapeutic management, and the screening for early diagnosis of COPD is of particular importance9,10,11. COPD causes breathlessness, manifesting initially during exertion, then it increases progressively along with the airflow obstruction and predisposes exacerbations and serious illness2. Therefore, distilling the essence of breathlessness is a specific responsibility of doctors, as dyspnea could be the first vital symptom of a chronic and reversible if identified and treated early enough respiratory disease10. Notably, several studies have revealed a high prevalence of COPD among smokers with minimal or no symptoms9.
A remarkable proportion of COPD patients are undiagnosed and made case finding worthwhile12. Primary care centers are ideal positions to identify COPD, constituting the first filter in the pathway to care for the majority of patients. The main objective of this study was to determine the COPD prevalence rate among ever-smokers in pre-retirement, aged 40–65 years, attending a 2-year primary care spirometry surveillance program in central Greece. The secondary objectives were to evaluate their demographic, clinical, and spirometric characteristics and make comparisons between patients less than or greater than 55 years of age, genders, and newly and previously diagnosed COPD patients.
Results
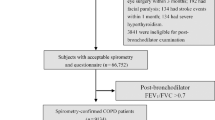
The flowchart of the study selection process is presented in Fig. 1. A total of 1100 smokers and ex-smokers aged 40–65 were included in the spirometry surveillance program according to inclusion criteria. A total of 117 newly diagnosed or previously known COPD patients were detected, providing a COPD prevalence of 10.6% among the study population. Of the 117 patients diagnosed with COPD after studying 1100 people, 83 (7.5%) were diagnosed for the first time, representing a rate of 70.94% of COPD underdiagnosis.
In our study, 1350 patients attended the 2-year spirometry surveillance program, from January 2018 to December 2019, in 22 Primary Health Centers in Central Greece. From all these patients, 1100 were smokers and ex-smokers aged 40–65 years old, the others 250 subjects were excluded according to the exclusion criteria of our study. From those subjects were eligible to participate, 117 subjects diagnosed with COPD (post FEV1/FVC<0.70) and 983 subjects had either normal postbronchodilator spirometry or positive bronchodilator response. Of the 117 patients diagnosed with COPD, 83 were diagnosed for the first time and 34 were previously known COPD patients. According to the gender, those with newly diagnosed COPD patients, 63 were males and 20 females, while of those with previously known COPD, 31 were males and only 3 were females. *Exclusion criteria: no smoking history, a history of lower or upper respiratory infection or antibiotic treatment within the last month, an operative procedure or acute myocardial infarction within the last three months, or inability to perform spirometry.
Characteristics of all COPD patients
The demographic, clinical, and spirometric characteristics of all COPD patients and comparisons between genders are shown in Table 1. Nearly four-fifths of all COPD patients were males with a mean age of 60.3 ± 5.8 years and a mean body mass index (BMI) within the overweight range. The majority were married, current smokers, and almost half of them were high school graduates. Importantly, 89% of the COPD population mentioned at least one respiratory symptom. Dyspnea was the most commonly reported symptom, followed by cough, wheezing, and sputum. One-third of COPD patients had dyspnea score greater than or equal to 2, i.e., breathlessness on level ground (grade 2), exercise limitation (grade 3), or dyspnea on rest (grade 4) according to modified Medical Research Council (mMRC) scale, while 40.2% of COPD patients reported COPD assessment test (CAT) total score of ≥10. More than half of the patients had at least one comorbidity and one exacerbation (Table 1).
A total of 92% of COPD patients were classified on Stages I/II. We found that 40% and 30% of COPD patients in GOLD Stage I/II scored more than 10 on the CAT score, and greater than or equal to 2 on mMRC score, respectively. COPD patients in GOLD Stage III/IV had more frequent wheezing symptoms than early-stage patients, as expected. No significant association was detected between different GOLD stages and BMI, educational level, marital status, or comorbidities. Interestingly, 54.7% of all COPD patients were classified into GOLD COPD Group A having fewer symptoms and a low risk of exacerbations, and more than one-third were classified into GOLD COPD Group B, having more symptoms and a low risk of exacerbation.
Almost 20% of all COPD patients were women. The majority of women (82.7%) diagnosed with COPD were in Group B, which means they had higher symptoms. The majority of men diagnosed with COPD were in Group A (66%), and one-third were in Group B (Table 1). Rates of newly diagnosed were higher among females compared to males (87% vs. 67%, P = 0.046). Women with COPD reported smoking fewer cigarettes than men, had an older age at starting smoking (24.3 ± 5.9 vs. 17.3 ± 6.7, P < 0.001), but experienced worse symptoms (CAT score ≥10) and had more frequent depression compared to males (Table 1).
Comparison of COPD patients’ characteristics according to age
A total of 19% (25/117) of the COPD population were below 55 years. Comparisons of demographic, clinical, and spirometric characteristics between COPD patients over and below 55 years of age are presented in Table 2.
COPD patients below the age of 55 years experienced wheezing and exacerbations more frequently than COPD patients older than 55 years. They were likely to have comorbidities, especially hypertension compared to older patients. Two-thirds of patients greater than or less than 55 years were newly diagnosed COPD patients.
Comparisons of newly and previously diagnosed COPD patients
Newly diagnosed COPD patients represented 70.9% of the COPD group. The differences between demographic, clinical, and spirometric characteristics of newly and previously diagnosed COPD patients are presented in Table 3.
Newly diagnosed COPD patients were significantly younger, were more likely to be female, had an older mean age of the first cigarette smoked, and smaller pack-year history than previously known COPD patients. Importantly, 85.5% of newly diagnosed COPD individuals reported at least one respiratory symptom, while 14.5% were asymptomatic. Moreover, we found that one-third of the newly diagnosed patients were highly symptomatic (mMRC ≥ 2 and CAT ≥ 10), and half of them had at least one exacerbation. Newly diagnosed and previously known COPD subjects have a similar percentage of cough and dyspnea. Patients with previously known COPD significantly more often suffered from coronary artery disease and depression than the newly diagnosed COPD group. Newly diagnosed patients had better lung function than known COPD patients.
The majority of newly diagnosed COPD patients were classified into GOLD Stages I and II. Approximately two-thirds of newly diagnosed COPD individuals were classified into GOLD COPD risk Group A, had fewer symptoms, and a low risk of exacerbation. Almost one-third of those patients had noteworthy respiratory symptoms and low risk of exacerbations classified into GOLD COPD risk Group B. Only patients with a previous diagnosis of COPD reached GOLD Stage IV, and GOLD COPD Group D.
A total of 25% of newly diagnosed patients were women classified from Stage I to Stage III. No differences in demographic and clinical characteristics were found between genders. Males had a lower level of lung function than women (forced expiratory volume in 1st second (FEV1)/forced vital capacity (FVC) ratio: 65.1 ± 4.43 vs. 67.5 ± 1.9, P < 0.018, respectively). Most of the patients who received the first diagnosis of COPD were married. No differences were found in the demographic characteristics of newly diagnosed COPD patients according to different GOLD COPD groups.
Notably, 20.5% (17/83) of the newly diagnosed patients were equal to or under the age of 55. In all, 52.9% (9/17) of those patients had already reached Stage II COPD and one patient reached Stage III COPD. A total of 23.5% (4/17) of these patients were assigned to Group B and the rest to Group A. No specific differences in demographic or clinical characteristics of newly diagnosed COPD patients aged less than 55 according to GOLD stages or GOLD COPD stages were found.
Discussion
In the current study, a high COPD prevalence of 10.6% among 1100 current or ex-smokers aged 40–65 was estimated. In Greece, the reported COPD prevalence ranged from 8.6 to 18.4%7 (Table 4). The great variations observed in the prevalence rates were mainly attributed to the absence of comparable methodologies.
Conversely, our results differ from other national studies of those exposed to tobacco that found higher COPD prevalence13. The variations observed in the prevalence rates were mainly due to differences in age and sex distribution and other population characteristics evaluated in each study. More specifically, we limited the population to those 40–65 years of age, given that global estimates have reported that although COPD rises significantly in the sixth decade and beyond, COPD is not seen any longer as a disease of the elderly, as a significant proportion of patients (up to 40%) with COPD are aged less than 65 years14. We focused on the concept of early COPD diagnosis, which is an emerging area for research.
A prior study of our team has noted that the underdiagnosis and missed diagnosis of COPD among the primary care smoking population is an old problem that persists in Greece12. A total of 7.5% of the study population received a diagnosis of COPD for the first time. Of the 117 patients finally diagnosed after studying 1100 people, 83 were diagnosed for the first time, representing a rate of 70.94% of underdiagnosis. Similarly, a previous post-economic crisis study conducted in ten primary healthcare centers of Central Greece during a 7-month period, including 186 current smokers or ex-smokers aged ≥40 years, demonstrated a prevalence rate of first-time diagnosed COPD of 7.5%12. Another pre-economic crisis study (conducted from January 2006 to June 2007) included 15 primary healthcare centers in central Greece, with a total of 1526 subjects aged over 30 years, documented a higher prevalence rate of new COPD cases of 18.4%8. The leading causes of COPD underdiagnosis and misdiagnosis are attributable to the lack of training and feedback for diagnostic spirometry, the lack of adoption of GOLD guidelines into routine clinical practice, and the improper symptom assessment by healthcare professionals15,16. Moreover, as our research findings highlight that decreased patients’ awareness contributes to COPD underdiagnosis.
A total of 20.7% of all COPD patients and 25% of newly diagnosed patients were women. It has been reported that approximately 20% of the smoking population worldwide are women16. Owing to the rising prevalence of COPD in women, increasing mortality risk for females with COPD is expected. The relative risk of death from COPD is currently nearly equal for males and females17. There is increasing evidence that in COPD pathogenesis, sex differences describe biology-linked differences between men and women, and sex biology has been associated with increased risk for COPD in women18,19. Estrogen induces lung differentiation and maturation; however, by the age of menopause, there is a considerable loss of lung function associated with smoking and estrogen and progesterone decline18,19. Our results support previous findings claimed that women with COPD reported smoking fewer cigarettes than men, had an older age at starting smoking, but experienced worse symptoms19. Women manifest more severe COPD symptoms across life course19. Consistent with the literature, this research found that females were more depressed than males20. COPD is a severe treatment-resistant pulmonary disease with varying impacts on the patient’s general physical condition, functioning, and quality of life. Depressive symptoms are common in patients affected by COPD, even when their disease is mild21. Female patients appear to be more susceptible to psychological risks. Although being diagnosed with depression can be hard, not receiving a definite diagnosis can be even more difficult to deal with21.
One of the most interesting findings of our study was that two out of ten patients among the COPD population were below 55 years. The vast majority of them were newly diagnosed COPD patients. Severe early-onset COPD is an interesting phenotype defined as COPD development in individuals younger than 50–55 years and often with a light pack-year smoking history22,23. There is evidence that these patients progress quickly24. Half of the newly diagnosed patients below 55 years had already reached Stage II COPD in our study. No information is available on the true impact of COPD of recent onset mainly because COPD has been previously considered a disease of the elderly25. The global prevalence of COPD in smokers or ex-smokers aged <50 years has been roughly estimated at 4.1% (95% CI 2.9–5.4%)25,26.
A few data regarding the age distribution of newly diagnosed COPD patients in Central Greece reported a higher mean age of new COPD diagnosis between 65 and 69 years8,12. In this study, we found that newly diagnosed COPD patients were significantly younger (59.6 ± 6.2 vs. 62.0 ± 4.7), had an older mean age of the first cigarette smoked, a smaller pack-year history than previously known COPD patients. Therefore, our findings supported that COPD patients were first diagnosed at a younger age than the national average of COPD diagnosis. COPD is a disease of accelerated aging. However, COPD is not considered any longer as an illness of the aged, as it can also affect younger adults under 65 years old3. Furthermore, COPD risks may already occur in adolescents, on the assumption that some are born with reduced pulmonary function and that infection and exposure to toxins at an early age may greatly reduce their pulmonary capacity3.
Ever-smokers with respiratory symptoms should have more careful health care. Importantly, 85.5% of newly diagnosed COPD individuals reported at least one respiratory symptom, while approximately two-thirds of newly diagnosed COPD individuals were classified into GOLD COPD risk Group A, had fewer symptoms, and a low risk of exacerbation. Indeed, many people with COPD symptoms do not meet the criteria for diagnosis according to lung-function tests indicating that they are healthy27,28. However, it has been documented that nearly 40% of the people who did not meet the definition of COPD when they joined an epidemiological study had late-stage disease 5 years later29,30,31.
This study found that one-third of the newly diagnosed patients were highly symptomatic (mMRC ≥ 2 and CAT ≥ 10), and half of them had at least one exacerbation. Despite the burden of symptoms, they did not seek medical help, as they felt COPD symptoms as part of their daily smoking routine or due to aging. These data indicate that COPD awareness is poor among smokers, and strategies to increase COPD awareness should be developed32,33,34. The smoking population underestimates their respiratory symptoms; however, exercise activity is many times reduced. Therefore, to detect new COPD cases, questions related to respiratory vulnerability and deconditioning are required27,35. Besides, recent studies showed that exacerbations are frequent in smokers, even they had normal spirometry tests. Another recent study showed that the presence of symptoms in ever-smokers with preserved pulmonary function is correlated with more exacerbations, activity limitation, and greater airway-wall thickening with or without emphysema28,36,37.
On the other hand, a significant percentage of 14.5% of the newly diagnosed COPD population was asymptomatic. This finding also accords with earlier observations, which showed a high prevalence of COPD among smokers with no symptoms9,38. Even among subjects with severe airflow obstruction, a substantial proportion did not report symptoms39,40. About 40% of those in the GOLD severe category denied being breathless39. Therefore, a mass screening on all smokers to detect COPD is suggested9,38. This case-finding strategy of COPD detection by screening for symptoms that patients may not themselves perceive is very important in primary care38. In addition, it is of high importance to screen smokers who had minimal or no symptoms or limited activity, regardless of their age, gender, or how long they have been smoking, for COPD to establish an early diagnosis for COPD patients to stop disease progression and improve the quality of life via the motivation for physical activity, smoking cessation, and potential pharmacological treatment38.
Another important finding of this study was that 60% of newly diagnosed COPD patients had at least one comorbidity. Tobacco smoking is a risk factor for many comorbidities, as well as for COPD. Systemic inflammation appeared to be shared across multiple chronic diseases41,42. Besides, we found that cardiovascular disease and depression were more likely to be developed in known COPD patients with higher smoking intensity than newly diagnosed patients. Certainly, people with COPD have a higher risk of cardiovascular disease43. COPD severity and duration have been correlated with increased risk of cardiovascular disease or depression43,44. On the other hand, patients with pre-existing depression or developed depression after COPD diagnosis were more likely to suffer from heightened COPD symptoms, such as increased breathlessness, reduced exercise tolerance, and hopelessness44.
The findings in this study are subject to a major limitation. The study was carried out on a local scale, which reduces the generalizability of the results. Moreover, this study limits the study population to those 40–65 years of age. It is expected that prevalence will increase in older age groups as a function of age and cumulative pack-years.
This primary care COPD screening program was implemented in ever-smokers younger than 65, and an increased prevalence rate of new COPD diagnosis comes to light. Women with COPD reported smoking fewer cigarettes than men, had an older age at starting smoking, but experienced worse respiratory and depressive symptoms. COPD is not considered any longer as an illness of the aged as it can also afflict the younger population. The findings clearly indicate that most newly diagnosed COPD patients reported a significant burden of symptoms without seeking medical help and finally diagnosed at a moderate stage of the disease. Approximately half of them had at least one exacerbation during the last year and complained of comorbid diseases. The underestimation of respiratory symptoms by smokers is a thorn in COPD diagnosis. A reasonable approach to tackle this issue could be to screen all smokers who report minimal or limited activity or even no respiratory symptoms, regardless of their age, gender, or how long they have been smoking, for COPD, and to implement smoking cessation counseling to control the disease’s progressiveness. Strategies to increase COPD awareness and change the natural history of COPD should be developed. The rule is that there are no rules in COPD; thus, primary health care has a crucial role in the early detection of COPD among unsuspecting smokers. The challenge is to find tactics accelerating the early detection of disease in primary care.
Methods
A 2-year (January 2018–December 2019) spirometry surveillance program was conducted in 22 primary healthcare centers in rural and semirural areas in Thessaly, Central Greece. All current smokers or ex-smokers resided near a primary healthcare setting, aged 40–65 years, and were willing to participate in a spirometry surveillance program, were included in the study. Smoking status was categorized into: (1) former smokers included adults who have smoked at least 100 cigarettes in their lifetime but who had quit smoking for at least a year and (2) current smokers included adults who have smoked 100 cigarettes in their lifetime and currently smoke cigarettes daily or nondaily. Smoking status for all subjects was measured in pack-years of cigarette smoking (pys). Exclusion criteria included no smoking history, a history of lower or upper respiratory infection or antibiotic treatment within the last month, recent eye surgery, an operative thoracic or abdominal procedure, or acute myocardial infarction within the last 3 months, and inability to perform spirometry. People with a lower or upper respiratory infection or antibiotic treatment within the last month were temporarily excluded from the study and scheduled for inclusion some weeks later. Ethical approval for this study was obtained from 5th Dypethessaly (Regional Health Authority of Thessaly & Sterea Ellada, Greek Ministry of Health) (Ref no: 20227/April 25, 2018 and Ref no: 2163/January 9, 2019 from 5th Dypethessaly). All subjects provided written informed consent.
Study design
Pre- and postbronchodilator spirometry tests were performed to establish the diagnosis of COPD, using portable spirometers. COPD patients filled out a questionnaire including questions on demographics, smoking status, occupational exposure, chronic respiratory symptoms (cough, sputum, wheezing, and dyspnea), history of respiratory infections, comorbidities, and exacerbations within the last 2 years. In addition, the CAT and the mMRC were completed by COPD participants to measure the impact of COPD on their life.
Spirometry procedure
Spirometry test was performed with a dry spirometer (Spirolab FCC ID: TUK-MIR045) according to American Thoracic Society recommendations45. Calibration checks were performed every morning before the beginning of the spirometry program. Spirometry testing was performed by eight physicians and two nurses who had undergone a special training program. Forced expiratory maneuvers were repeated until three acceptable reproducible tests were obtained and the best FEV1, FVC, and FEV1/FVC ratio were recorded. The spirometric reference values used were those proposed by the ERS statement46. An acceptable maneuver was defined using the previously described criteria47.
Diagnosis of COPD
COPD diagnosis was established with the presence of a postbronchodilator FEV1/FVC ratio less than 0.70 following GOLD guidelines48,49. All patients under inhaled medication were instructed to avoid their inhalers for 12 or 24 h depending on the drug formulation (for instance, SABA ≥ 4 h, LABA ≥ 15 h, LAMA ≥ 12 or 24 h) before spirometry. A bronchodilator reversibility test with 400 µg of salbutamol was performed in all patients with a baseline prebronchodilator obstructive spirometry. A positive response to bronchodilators was defined as an increase in the FEV1 of 200 ml and 12% from the prebronchodilator value (baseline value). All participants with a positive bronchodilator response were excluded from the analyses. Classification of COPD was based on the postbronchodilator FEV1 (%) according to GOLD guidelines (Stage I/mild COPD, FEV1 ≥ 80%; Stage II/moderate COPD, 50% ≤ FEV1 < 80%; Stage III/severe COPD, 30% ≤ FEV1 < 50%; Stage IV/very severe COPD, FEV1 ≤ 30% or FEV1 < 50% with respiratory failure)49. Patients with COPD were also allocated into four groups by GOLD (GOLD Groups A, B, C, and D) according to the 2020 GOLD guidelines49.
Statistical analyses
Demographic data were presented as mean ± standard deviation. Categorical variables are presented as percentages. Differences in numerical variables were evaluated with independent-samples t-test or Mann–Whitney U test and Tukey’s multiple comparisons test for normally and skewed data, respectively, whereas comparisons of proportions were performed using χ2 test with applying the Bonferroni correction. P values < 0.05 were considered statistically significant. The results were analyzed statistically with SPSS 26, and graphs were made using PRISM 8.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study are available on request from the corresponding authors, O.S.K. and E.G. The data are not publicly available due to restrictions, e.g., their containing information that could compromise the privacy of research participants.
References
Huang, X. et al. The etiologic origins for chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 14, 1139–1158 (2019).
Pommer, P. Chronic obstructive pulmonary disease (COPD). Dtsch. Med. Wochenschr. 137, 2589 (2012).
Sin, D. D., Stafinski, T., Ng, Y. C., Bell, N. R. & Jacobs, P. The impact of chronic obstructive pulmonary disease on work loss in the United States. Am. J. Respir. Crit. Care Med. 165, 704–707 (2002).
Britton, M. The burden of COPD in the U.K.: results from the Confronting COPD survey. Respir. Med. 97 Suppl C, S71–S79 (2003).
De Marco, R. et al. An international survey of chronic obstructive pulmonary disease in young adults according to GOLD stages. Thorax 59, 120–125 (2004).
Mitsiki, E., Bania, E., Varounis, C., Gourgoulianis, K. I. & Alexopoulos, E. C. Characteristics of prevalent and new COPD cases in Greece: the GOLDEN study. Int. J. Chron. Obstruct. Pulmon. Dis. 10, 1371–1382 (2015).
Kotsiou, O. S., Zouridis, S., Kosmopoulos, M. & Gourgoulianis, K. I. Impact of the financial crisis on COPD burden: Greece as a case study. Eur. Respir. Rev. 27, 170106 (2018).
Minas, M. et al. COPD prevalence and the differences between newly and previously diagnosed COPD patients in a spirometry program. Prim. Care Respir. J. 19, 363–370 (2010).
Sansores, R. H. et al. Prevalence of chronic obstructive pulmonary disease in asymptomatic smokers. Int. J. Chron. Obstruct. Pulmon. Dis. 10, 2357–2363 (2015).
Currow, D. C. & Johnson, M. J. Distilling the essence of breathlessness: the first vital symptom. Eur. Respir. J. 45, 1526–1528 (2015).
Csikesz, N. G. & Gartman, E. J. New developments in the assessment of COPD: early diagnosis is key. Int. J. Chron. Obstruct. Pulmon. Dis. 9, 277–286 (2014).
Stafyla, E., Kotsiou, O. S., Deskata, K. & Gourgoulianis, K. I. Missed diagnosis and overtreatment of COPD among smoking primary care population in central Greece: old problems persist. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 487–498 (2018).
Llordés, M. et al. Prevalence, risk factors and diagnostic accuracy of COPD among smokers in primary care. COPD 12, 404–412 (2015).
Adeloye, D. et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J. Glob. Health 5, 020415 (2015).
Albitar, H. A. H. & Iyer, V. N. Adherence to Global Initiative for Chronic Obstructive Lung Disease guidelines in the real world: current understanding, barriers, and solutions. Curr. Opin. Pulm. Med. 26, 149–154 (2020).
World Health Organization. Gender, health and tobacco. Heal. San. Fr. 1–4 (2003).
World Health Organization. Burden of COPD. https://www.who.int/respiratory/copd/burden/en/.
Mustonen, T. K., Spencer, S. M., Hoskinson, R. A., Sachs, D. P. L. & Garvey, A. J. The influence of gender, race, and menthol content on tobacco exposure measures. Nicotine Tob. Res. 7, 581–590 (2005).
Jenkins, C. R. et al. Improving the management of COPD in women. Chest 151, 686–696 (2017).
Quint, J. K., Baghai-Ravary, R., Donaldson, G. C. & Wedzicha, J. A. Relationship between depression and exacerbations in COPD. Eur. Respir. J. 32, 53–60 (2008).
Di Marco, F. et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir. Med. 100, 1767–1774 (2006).
Foreman, M. G. et al. Early-onset chronic obstructive pulmonary disease is associated with female sex, maternal factors, and African American race in the COPD Gene study. Am. J. Respir. Crit. Care Med. 184, 414–420 (2011).
Silverman, E. K. et al. Genetic epidemiology of severe, early-onset chronic obstructive pulmonary disease: risk to relatives for airflow obstruction and chronic bronchitis. Am. J. Respir. Crit. Care Med. 157, 1770–1778 (1998).
Brandsma, C. A. et al. Lung ageing and COPD: is there a role for ageing in abnormal tissue repair? Eur. Respir. Rev. 26, 1–15 (2017).
Soriano, J. B., Polverino, F. & Cosio, B. G. What is early COPD and why is it important? Eur. Respir. J. 52, 1801448 (2018).
Miravitlles, M. et al. Prevalence of COPD in Spain: impact of undiagnosed COPD on quality of life and daily life activities. Thorax 64, 863–868 (2009).
Woodruff, P. G. et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N. Engl. J. Med. 374, 1811–1821 (2016).
De Jesús Hernández-Zenteno, R., Flores-Trujillo, F., Javier Vázquez-Cortés, J., Espinosa De Los Monteros-Sánchez, C. & Cosío, M. G. Symptomatic and asymptomatic smokers without airflow obstruction: a new clinical entity? Rev. Invest. Clin. 71, 64–69 (2019).
Young, K. A. et al. Pulmonary subtypes exhibit differential global initiative for chronic obstructive lung disease spirometry stage progression: the COPDGene® study. Chronic Obstr. Pulm. Dis. 6, 414–429 (2019).
Hangaard, S., Helle, T., Nielsen, C. & Hejlesen, O. K. Causes of misdiagnosis of chronic obstructive pulmonary disease: a systematic scoping review. Respir. Med. 129, 63–84 (2017).
Herrera, A. C. et al. COPD underdiagnosis and misdiagnosis in a high-risk primary care population in four Latin American countries. a key to enhance disease diagnosis: the PUMA study. PLoS ONE 11, e015226609 (2016).
Hwang, Y. I. et al. Male current smokers have low awareness and optimistic bias about COPD: field survey results about COPD in Korea. Int. J. Chron. Obstruct. Pulmon. Dis. 14, 271–277 (2019).
Baiardini, I. et al. Disease awareness in patients with COPD: measurement and extent. Int. J. Chron. Obstruct. Pulmon. Dis. 14, 1–11 (2019).
Xu, G., Fan, G. & Niu, W. COPD awareness and treatment in China. Lancet Respir. Med. 6, e38 (2018).
Erbas, B. et al. Critical age windows in the impact of lifetime smoking exposure on respiratory symptoms and disease among ever smokers. Environ. Res. 164, 241–247 (2018).
Jetmalani, K. et al. Peripheral airway dysfunction and relationship with symptoms in smokers with preserved spirometry. Respirology 23, 512–518 (2018).
Thomson, N. C. Respiratory symptoms and small airway dysfunction in current and former smokers without spirometric COPD. Respirology 23, 446–447 (2018).
Kaplan, A. & Thomas, M. Screening for COPD: the gap between logic and evidence. Eur. Respir. Rev. 26, 1–6 (2017).
Agusti, A. et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir. Res. 11, 122 (2010).
Lu, M. et al. Asymptomatic patients of chronic obstructive pulmonary disease in China. Chin. Med. J. (Engl.) 123, 1494–1499 (2010).
Chatila, W. M., Thomashow, B. M., Minai, O. A., Criner, G. J. & Make, B. J. Comorbidities in chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 5, 549–555 (2008).
Agustí, A. Systemic effects of chronic obstructive pulmonary disease: What we know and what we don’t know (but should). Proc. Am. Thorac. Soc. 4, 522–525 (2007).
Rabe, K. F., Hurst, J. R. & Suissa, S. Cardiovascular disease and COPD: dangerous liaisons? Eur. Respir. Rev. 27, 180057 (2018).
Hanania, N. A. et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am. J. Respir. Crit. Care Med. 183, 604–611 (2011).
Crapo, O. et al. Standardization of spirometry: 1994 Update. Am. J. Respir. Crit. Care Med. 152, 1107–1136 (1995).
Quanjer, P. H. et al. Lung volumes and forced ventilatory flows. Eur. Respir. J. 6, 5–40 (1993).
Moore, V. C. Spirometry: step by step. Breathe 8, 232–240 (2012).
Global Initiative for Chronic Obstructive Lung Disease. Global Initiative for Chronic Obstructive. GOLD, Global Obstructive Lung Disease. http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Apr2.pdf (2017).
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 Report). https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
Gourgoulianis, K. I., Katikos, P., Moraitis, M., Argiriou, N. & Molyvdas, P. A. Chronic bronchitis in rural and industrial areas. Ann. Agric. Environ. Med. 27, 29–31 (2000).
Tzanakis, N., Anagnostopoulou, U., Filaditaki, V., Christaki, P. & Siafakas, N., COPD Group of the Hellenic Thoracic Society. Prevalence of COPD in Greece. Chest 125, 892–900 (2004).
Sichletidis, L. et al. Prevalence of chronic obstructive pulmonary disease and rhinitis in northern Greece. Respiration 72, 270–277 (2005).
Kourlaba, G., Hillas, G., Vassilakopoulos, T. & Maniadakis, N. The disease burden of chronic obstructive pulmonary disease in Greece. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 2179–2189 (2016).
Spyratos, D., Chloros, D., Michalopoulou, D. & Sichletidis, L. Estimating the extent and economic impact of under and overdiagnosis of chronic obstructive pulmonary disease in primary care. Chron. Respir. Dis. 13, 240–246 (2016).
Acknowledgements
The authors would like to thank the health professionals in the primary healthcare centers in Thessaly for the valuable collaboration.
Author information
Authors and Affiliations
Contributions
K.I.G., C.H., and E.G. conceived of the presented idea and designed the study. E.G., O.S.K., D.S.S., M.P., C.V., F.B., and I.G. contributed to sample collection, sample preparation, and data analysis. O.S.K. and E.G. contributed equally to the writing of the paper. However, Ο.S.K. took finally the lead in writing the manuscript. K.I.G. supervised the study. All authors provided critical feedback and approved the final draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gogou, E., Kotsiou, O.S., Siachpazidou, D.S. et al. Underestimation of respiratory symptoms by smokers: a thorn in chronic obstructive pulmonary disease diagnosis. npj Prim. Care Respir. Med. 31, 14 (2021). https://doi.org/10.1038/s41533-021-00226-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-021-00226-y