Abstract
Estimates of the prevalence of Parkinson’s disease in North America have varied widely and many estimates are based on small numbers of cases and from small regional subpopulations. We sought to estimate the prevalence of Parkinson’s disease in North America by combining data from a multi-study sampling strategy in diverse geographic regions and/or data sources. Five separate cohort studies in California (2), Minnesota (1), Hawaii USA (1), and Ontario, Canada (1) estimated the prevalence of PD from health-care records (3), active ascertainment through facilities, large group, and neurology practices (1), and longitudinal follow-up of a population cohort (1). US Medicare program data provided complementary estimates for the corresponding regions. Using our age- and sex-specific meta-estimates from California, Minnesota, and Ontario and the US population structure from 2010, we estimate the overall prevalence of PD among those aged ≥45 years to be 572 per 100,000 (95% confidence interval 537–614) that there were 680,000 individuals in the US aged ≥45 years with PD in 2010 and that that number will rise to approximately 930,000 in 2020 and 1,238,000 in 2030 based on the US Census Bureau population projections. Regional variations in prevalence were also observed in both the project results and the Medicare-based calculations with which they were compared. The estimates generated by the Hawaiian study were lower across age categories. These estimates can guide health-care planning but should be considered minimum estimates. Some heterogeneity exists that remains to be understood.
Similar content being viewed by others
Introduction
Prevalence estimates of disease are important for public health planning. The upcoming demographic shifts toward older individuals in western nations have led to major efforts to project the health-care burden over the coming decades, particularly for diseases for which incidence rises considerably with age, such as Alzheimer’s disease and Parkinson’s disease (PD). The projected increases in dementia have been referred to as a “Rising tide,” emphasizing the sheer volume of this problem and warnings of the public health challenges of caring for these individuals have been issued.1 PD presents similar challenges as its prevalence in the world’s most populous nations has been projected to more than double between 2005 and 2030.2 These estimates do not account for changes in exposures that may further contribute to increased incidence or prevalence.3
A recent systematic review and meta-analysis examined the prevalence of PD worldwide as estimated by studies performed since 1985. Included in the review were studies that used door-to-door ascertainment or random population sampling followed by physical examination.4 Point estimates of age-specific prevalence across regions varied widely, and confidence intervals were broad, limiting the interpretability of these data for public health planning. Furthermore, only two such studies were identified in North America since 1985, both in Canada identifying 2 and 4 PD cases each.5,6 An earlier study of PD prevalence in Copiah County, Mississippi, USA conducted in 1978 is commonly used as the estimate of prevalence for PD in the US, although its calculations were based on only 26 cases of idiopathic PD ascertained from a small area.7 More recent estimates based on more robust data from a wider sampling frame are needed.
Commonly, medical records or health system claims data are used to estimate PD prevalence. The limitations of this approach with respect to diagnostic misclassification notwithstanding, an advantage of such studies is their size, often using data on millions of individuals to deliver more precise estimates than can be produced by studies that contact people directly. North American estimates of PD prevalence from such studies have varied widely and have noted geographical variation.8,9,10,11,12,13
Beginning in 2014, the Parkinson’s Foundation established the Parkinson’s Foundation Parkinson’s Prevalence Project (P4) to coordinate epidemiological investigations of prevalence conducted at disparate sites throughout North America. The P4 Project combines data from five different recent or current projects covering four different regions across North America and compares these to prevalence estimates generated using nationwide data from the US to provide an updated and more precise estimate of PD burden. Specifically, we aimed to address the following questions:
-
1.
Is the prevalence of PD uniform throughout North America or does it vary by study and/or geography?
-
2.
To the extent that these data can be considered consistent, what meta-estimates of prevalence do they provide?
Results
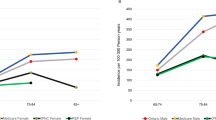
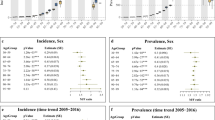
The populations studied (aged ≥45 years) ranged in size from 8006 (Honolulu-Asia Aging Study (HAAS)) to 5,525,787 (Ontario). The number of cases identified by project ranged from 207 to 28,065. Table 1 shows the case numbers, denominators, and prevalence estimates for each project by sex. The supplementary table provides prevalence further broken down by age group. Figure 1 displays the prevalence estimates closest to 2010 for each project and provides the meta-analytic estimate for each age group by sex. The prevalence within age strata below the age of 65 years for males and below the age of 75 years for females have confidence intervals for I2 containing nearly its entire possible range, which implies that our results do not contain enough information to rule heterogeneity in or out. For older ages, heterogeneity is demonstrated. The estimates were higher in men than in women and rose with age in both sexes. Using Kaiser Permanente Northern California Integrated Health Care System (KPNC), Ontario, Rochester Epidemiology Project (REP), and California Parkinson’s disease Registry-Pilot Project (CPDR-PP) data, the combined prevalence for men and women aged >45 years standardized by age and sex to the US population according to the 2010 US census was 572 per 100,000 (95% confidence intervals 537–614). For females, the prevalence was 488 (444–543), and for males 667 (612–732). Based on published data, we calculated the prevalence of parkinsonism as estimated by the Copiah County study7 standardized to the US population (2010) to be 301 per 100,000 (Table 2). Using our age- and sex-specific meta-estimates and applying these to the US population according to the 2010 census, we would expect 680,000 cases of PD in the US among individuals aged ≥45 years. Given the projected population structure for future years and assuming stable age and sex-specific prevalences, we estimate that this number would rise to 930,000 cases in 2020 and 1,238,000 by 2030.
Prevalence of PD aged ≥45 years by age group and sex: a Females. b Males. HAAS Honolulu-Asia Aging Study, REP Rochester Epidemiology Project, CPDR-PP California Parkinson’s disease Registry-Pilot Project, KPNC Kaiser Permanente Northern California Integrated Health Care System. In each row, the squares or diamonds are centered on the point estimate of the prevalence and whiskers represent 95% confidence intervals. Point estimates for HAAS are indicated by circles instead of squares because the meta-estimates exclude the HAAS study due to methodologic differences between this and the other studies
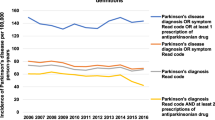
Figure 2 shows the prevalence estimates for the studies of California, Olmsted County, Minnesota, and Hawaii juxtaposed with the prevalence estimates derived from US Medicare data from the corresponding counties. Because Medicare beneficiaries are aged ≥65 years, we employ the portions of study subjects matching this age restriction. For two studies (CPDR-PP and HAAS), prevalence rates were statistically indistinguishable from the Medicare estimates. In contrast, the Rochester Epidemiology Project (Olmsted County) identified 14–27% more cases, and the KPNC approximately 30% more. However, the pattern of variation between regions is reproduced regardless of whether Medicare data or the P4 study data are used (Fig. 2).
Prevalence estimates by study compared to Medicare data from the corresponding counties. The corresponding counties were as follows: For California PD Registry Pilot Project: Fresno, Kern, Santa Clara, and Tulare, for Rochester Epidemiology Project: Olmsted, for KPNC: Alameda, Amador, Contra Costa, El Dorado, Fresno, Kings, Madera, Marin, Mariposa, Merced, Napa, Placer, Sacramento, San Francisco, San Joaquin, San Mateo, Santa Clara, Santa Cruz, Solano, Sonoma, Stanislaus, Sutter, Tulare, Yolo, and Yuba counties, for HAAS: Honolulu
Discussion
Our multi-study, multi-regional approach provides current estimates for PD prevalence among individuals over the age of 45 years, which overall is 572/100,000. The estimates from the individual studies are generally similar, and the meta-estimate confidence intervals are narrow, reflecting the large size of the component studies. Despite the overall similarity, there is evidence for heterogeneity, particularly a lower estimated prevalence from the HAAS study conducted on Japanese American men in Hawaii. HAAS has, since 1991, complemented its medical record-based case-finding with an in-person screening examination of participating individuals. This method would be expected to minimize missing cases, and as none of the other studies undertook unselected screening and examination of participants, one would expect the ascertainment in the HAAS study to be the most complete. In addition, loss to follow-up rates are very low.14 These observations suggest that the lower prevalence estimate reflects differences in environmental or genetic risk factors or could relate to the timing of the study that extends from 1965 to 2012. Incidence rates in the HAAS cohort reported in prior studies were reported as being comparable to rates in European and the US populations and were higher for Asians living in Asia.14 Interestingly, in a recent systematic review of PD prevalence studies using random sampling methods or door-to-door ascertainment with case verification through in-person examination, individuals 70–79 years of age in Asia were found to have a significantly lower prevalence of PD (646 per 100,000) compared with individuals of the same age in Europe, North America, and Australia (1602 per 100,000; P < 0.05).4 Using Medicare data, a lower prevalence in Asian individuals living in the United States than White or Hispanic individuals has been found8 and a non-significantly lower incidence in individuals of Asian ancestry has also been found using KPNC data from northern California.15 These findings are consistent with our own.
Despite the fact that the P4 prevalence estimates other than HAAS are similar to each other, our sample sizes are large enough to document significant heterogeneity and this heterogeneity is mirrored in the subgroup over age 65 years by corresponding variations in estimates based solely on Medicare records when adjusting for age and sex. We find this suggestive that—even within North America—the prevalence of PD that has come to medical attention does vary by region. Geographic variations in PD prevalence within the US have also been reported previously using solely Medicare data: Willis et al.1 found two- to ten-fold variations in PD prevalence between US counties. Whether or not these differences reflect variations in health-care seeking practices or access to care (including access to neurologists) or regional differences in environmental or genetic determinants of disease cannot be determined by our study and remain an important question for future research.
The heterogeneity must be kept in mind when expressing the prevalence of PD in North America as a single number. The meta-estimate is generated from projects sampling from a few disparate regions and we did not account for the heterogeneity that likely exists in other regions of North America. There is additional evidence for ethnic, socioeconomic, and geographic variation in PD prevalence in North America. A study of continental American and Alaskan natives10 reported a prevalence of 822/100,000 over age 40 years standardized to the 2000 US population, which is higher than most estimates from other places and ethnic groups worldwide. As previously mentioned, analysis of the Medicare nationwide database found a higher prevalence in Whites and Hispanics than in Black or Asian individuals.8 That same study found Copiah County, Mississippi, USA to have one of the lowest prevalence rates in the country and also revealed other geographic variations within the US. The geographic areas from which our data are drawn have a lower proportion of individuals of Black race than the US overall. Thus not taking these racial distributions into account would result in a higher estimate of PD prevalence for the entire US. Despite this potential bias, we believe that our estimates underestimate the total burden for reasons explained further below.
Other variations in PD prevalence have also been observed. Using health-care claims, PD prevalence in the Canadian province of Manitoba in both rural and urban areas was higher in areas with lower average income.11 Rates of hospital discharges for PD across Canada have also been reported to vary significantly, suggesting that PD prevalence was higher in Western provinces.12 The reasons for these observed variations need to be understood. They support the need for a sampling scheme with wide geographic and socioeconomic variation if a representative sample is going to be obtained. However, our prevalence estimates are consistent enough to support the use of our meta-estimates excluding the HAAS for use in public health discussion and planning at least until more exhaustive region-specific studies within North America become available.
Previous PD prevalence estimates in North America have varied widely. The now historical study of PD prevalence in Copiah County7 ascertained cases of PD through door-to-door contact, conducting screening interviews by a non-medical interviewer followed by neurological evaluation by a physician and an extensive multi-source data-gathering method in those who screened positive.16 Despite this careful case ascertainment, the age- and sex-standardized prevalence estimate in individuals over age 45 years, standardized to the US 2010 population is 301/100,000, smaller than our estimate of 572. The authors of the Copiah County study appropriately cautioned readers on assuming generalizability of their findings beyond the geographical boundaries of Copiah County and emphasized the usefulness of their work as providing inter-racial comparisons.
Several other regional studies of PD prevalence within North America have been published. Using the health-care administrative data sources in Ontario, Canada, the average prevalence of PD in 1992–1998 was estimated to be 363/100,000 in men and 324/100,000 in women.13 Direct comparison is difficult, however, because this estimate was derived using different case identification criteria, included the entire lifespan (whereas our estimates are restricted to individuals over age 45 years), and these are estimates that were adjusted to the Ontario population structure. A prevalence of 144/100,000 in the Canadian province of British Columbia was reported using drug-tracer methodology, which would only detect treated PD.9 The Canadian Community Health Survey found that 200/100,000 of Canadians living in private households self-reported a diagnosis of PD.17 Although generally lower than our estimates, variations in ascertainment methods could account for these differences.
The validity of our estimates relies on accurate and complete case ascertainment. Our estimates likely underestimate the true prevalence for several reasons: (1) Except for cases in HAAS, PD cases in the other studies included were all identified through accessing medical records or claims data of health-care systems and thus would miss those not seeking care, seeking care from other types of health-care providers, or without access to care. (2) Ascertainment through assigned diagnostic codes is inevitably incomplete due to incomplete or inaccurate coding. For example, the sensitivity of the ascertainment algorithm for cases in Ontario, the largest of the P4 projects, is estimated to be approximately 72%. (3) Some studies could not conduct complete ascertainment: for example, in the CPDR-PP not all providers were contacted due to limited resources and CPDR-PP and Medicare estimates do not include cases treated by providers whose data were not shared owing to strict privacy or administrative rules. Thus our estimates are best considered minimum prevalence estimates. At the same time, we must acknowledge that without individual case validation, which was not possible in several of our datasets, there is risk of both false-positive and false-negative determinations of case status. Despite many sources of variation, however, we derived fairly consistent estimates of prevalence among the component projects.
The projections of PD case numbers over the next 12 years assume stable prevalence within age and sex strata. However, if incidence rises or mortality from PD lessens, then prevalence would rise and our projections would underestimate the case burden above and beyond the issues of incomplete ascertainment mentioned above. There is evidence that incidence may be increasing18 and this is consistent with the fact that our lowest prevalence estimates came from the HAAS project, which spanned earlier years than the other projects in P4.
Our projected minimum estimates of PD case burden, rising to more than one million people in the US by 2030, highlight the growing importance of optimizing care and treatment for people with PD, lessening the burden of care on the caregivers, and easing the strain on health and elder care systems. Furthermore, our data and data from other studies suggest regional variation that deserves to be studied in order to reveal whether or not this variation stems from differences in susceptibility to the disease or differences in access to or utilization of health-care services. Accurate estimates of PD incidence and mortality in different geographic regions are also needed to assist in answering these questions.
Methods
Data collection
Prevalence was estimated for individuals aged ≥45 years from 5 different projects undertaken in 4 different regions of USA and Canada: (1) Ontario, Canada, (2) Olmsted County, Minnesota, USA: The REP,19 (3) California, USA: KPNC15 and the CPDR-PP, and (4) Honolulu County, Hawaii, USA: The HAAS.14 In addition, data from the US Medicare program, which provides health insurance to 98% of the population aged ≥65 years was used as a complementary data source. The study populations and case ascertainment methods are described in Table 3. For comparison purposes, data from Copiah County, Mississippi, USA were taken from the published literature.7
To be designated as a prevalent case in all projects except HAAS, the individual must have been alive and residing in the geographic area on the prevalence day or during the prevalence year. Diagnostic criteria (Table 3) needed to be met prior to the prevalence day or during the prevalence year in all projects except the REP where symptom onset before the prevalence day was sufficient to satisfy the designation of prevalent. The ascertainment years were 2010 for Ontario, KPNC, and CPDR-PP and 2006 for REP. For the cohort study, HAAS, a prevalent case was defined as having PD within the period (i.e., age stratum) of interest at any time between 1965 and 2012.
The work was approved by the following research ethics committees:
Ontario, Canada: The Research Board at Sunnybrook Health Sciences Centre, Toronto.
CDPR-PP: The ascertainment activity was reviewed by the State of California IRB and determined to be public health surveillance. Use for research was approved as part of the PRIDE project, approved by the State of California IRB and the University of California at San Francisco IRB. The University of California at Los Angeles IRB also approved the CPDR-PP.
KPNC: The University of California at San Francisco IRB.
HAAS: Kuakini Medical Center, Honolulu, HI, and Veterans Affairs Pacific Islands Health Care System, Honolulu, HI Institutional Review Boards.
REP: The Institutional Review Boards of Mayo Clinic and Olmsted Medical Center, Rochester, MN.
Statistical analysis
Using prevalence data from the individual studies, we employed the metafor20 package within the R programming environment21 to fit random-effects models for each sex and 10-year age stratum 45–54 through 85+. We represent heterogeneity using the I2 statistic of Higgins and colleagues;22 this statistic describes the percentage of variation across studies that appears to be due to study heterogeneity rather than chance. 95% confidence intervals for the I2 statistic were calculated using published methods.23
For females and males, we apply the random-effects regression separately to each of our five 10-year age groups \(i\), resulting in summary coefficients \(\hat \beta _i\) such that the age-specific prevalence is \(e^{\hat \beta _i}\). Similarly, our age-standardized meta-estimate is \(\hat r = \mathop {\sum }\limits_i w_i\left( {e^{\hat \beta _i}} \right)\), where \(w_i\) is the proportional representation of each age group in the 2010 US population24 such that \(\mathop {\sum }\limits_i w_i = 1\). Confidence intervals for \(\hat r\) were made by replacing \(\hat \beta _i\) in the above formula with \(\beta _i\sim N\left( {\hat \beta _i,\hat \sigma _i^2} \right)\), where \(\hat \sigma _i^2\) is the variance of each coefficient \(\hat \beta _i\). We report the 2.5th and 97.5th percentiles of \(\hat r\) based on an arbitrarily large number of samples (1 million of each \(\beta _i\)). Estimates of the number of expected cases in 2020 and 2030 are calculated using the population projections for the entire nation of the US published by the US Census Bureau.24
Unique among the P4 efforts, HAAS is a longitudinal study following a fixed cohort of men over an extended period of time (1965–2012). The total number of years each subject was alive constitutes the number of person-years at risk (denominator), while the number of years over which a subject had a diagnosis of PD defines the case number within a period of interest (numerator). While common assumptions regarding the Poisson distribution of rare diseases can be applied to the other efforts to generate measures of uncertainty, HAAS data require a bootstrap resampling approach.25 As such, we report prevalence estimates from the HAAS cohort for comparison alongside those from other research efforts and do not incorporate them into the random-effects models to derive the summary estimates.
To compare prevalence estimates generated by the four P4 projects to those produced by US Medicare records, we calculated prevalence from Medicare data for each group of US counties included in the US P4 project catchment areas (see legend to Fig. 2 for the corresponding counties).
All rates are presented for males and females aged ≥65 years and standardized to the US 2010 population using 5-year age strata;24 confidence intervals are calculated using the method of Tiwari and colleagues.26
Data availability
Data for this project are not owned by or under the control of the authors. Owing to either privacy regulations or data-sharing agreements, data cannot be made available.
Code availability
Analytic code can be made available upon request to the corresponding author.
References
Smetanin, P. et al. Rising Tide: The Impact of Dementia in Canada 2008 to 2038 (RiskAnalytica, 2009).
Dorsey, E. R. et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 68, 384–386 (2007).
Rossi, A. et al. Projection of the prevalence of Parkinson’s disease in the coming decades: revisited. Mov. Disord. 33, 156–159 (2017).
Pringsheim, T., Jette, N., Frolkis, A. & Steeves, T. D. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov. Disord. 29, 1583–1590 (2014).
Moghal, S., Rajput, A. H., D’Arcy, C. & Rajput, R. Prevalence of movement disorders in elderly community residents. Neuroepidemiology 13, 175–178 (1994).
Moghal, S., Rajput, A. H., Meleth, R., D’Arcy, C. & Rajput, R. Prevalence of movement disorders in institutionalized elderly. Neuroepidemiology 14, 297–300 (1995).
Schoenberg, B. S., Anderson, D. W. & Haerer, A. F. Prevalence of Parkinson’s disease in the biracial population of Copiah County, Mississippi. Neurology 35, 841–845 (1985).
Wright Willis, A., Evanoff, B. A., Lian, M., Criswell, S. R. & Racette, B. A. Geographic and ethnic variation in Parkinson disease: a population-based study of US Medicare beneficiaries. Neuroepidemiology 34, 143–151 (2010).
Lai, B. C., Schulzer, M., Marion, S., Teschke, K. & Tsui, J. K. The prevalence of Parkinson’s disease in British Columbia, Canada, estimated by using drug tracer methodology. Park. Relat. Disord. 9, 233–238 (2003).
Gordon, P. H., Mehal, J. M., Holman, R. C., Rowland, A. S. & Cheek, J. E. Parkinson’s disease among American Indians and Alaska natives: a nationwide prevalence study. Mov. Disord. 27, 1456–1459 (2012).
Lix, L. M. et al. Socioeconomic variations in the prevalence and incidence of Parkinson’s disease: a population-based analysis. J. Epidemiol. Community Health 64, 335–340 (2010).
Svenson, L. W. Regional disparities in the annual prevalence rates of Parkinson’s disease in Canada. Neuroepidemiology 10, 205–210 (1991).
Guttman, M., Slaughter, P. M., Theriault, M. E., DeBoer, D. P. & Naylor, C. D. Burden of parkinsonism: a population-based study. Mov. Disord. 18, 313–319 (2003).
Morens, D. M. et al. Epidemiologic observations on Parkinson’s disease: incidence and mortality in a prospective study of middle-aged men. Neurology 46, 1044–1050 (1996).
Van Den Eeden, S. K. et al. Incidence of Parkinson’s disease: variation by age, gender, and race/ethnicity. Am. J. Epidemiol. 157, 1015–1022 (2003).
Schoenberg, B. S., Anderson, D. W. & Haerer, A. F. Racial differentials in the prevalence of stroke. Copiah County, Mississippi. Arch. Neurol. 43, 565–568 (1986).
Wong, S. L., Gilmour, H. & Ramage-Morin, P. L. Parkinson’s disease: prevalence, diagnosis and impact. Health Rep. 25, 10–14 (2014).
Savica, R., Grossardt, B. R., Bower, J. H., Ahlskog, J. E. & Rocca, W. A. Time trends in the incidence of Parkinson disease. JAMA Neurol. 73, 981–989 (2016).
Melton, L. J. 3rd History of the Rochester Epidemiology Project. Mayo Clin. Proc. 71, 266–274 (1996).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36, 48 (2010).
R Core Team. R: a language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, (2017).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ (Clin. Res. Ed.) 327, 557–560 (2003).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
USC Bureau. IDB Population Pyramids (Washington, DC).
Efron, B. Bootstrap methods: another look at the jackknife. Ann. Stat. 7, 1–26 (1979).
Tiwari, R. C., Clegg, L. X. & Zou, Z. Efficient interval estimation for age-adjusted cancer rates. Stat. Methods Med. Res. 15, 547–569 (2006).
Gordon, N. P. Similarity of the Adult Kaiser Permanente Membership in Northern California to the Insured and General Population in Northern California: Statistics from the 2011-12 California Health Interview Survey (Kaiser Permanente Division of Research, Oakland, CA, 2015.
Bower, J. H., Maraganore, D. M., McDonnell, S. K. & Rocca, W. A. Incidence and distribution of parkinsonism in Olmsted County, Minnesota, 1976-1990. Neurology 52, 1214–1220 (1999).
Ward, C. D. & Gibb, W. R. Research diagnostic criteria for Parkinson's disease. Adv. Neurol. 53, 245–249 (1990).
Butt, D. A. et al. A validation study of administrative data algorithms to identify patients with Parkinsonism with prevalence and incidence trends. Neuroepidemiology 43, 28–37 (2014).
Turcano, P. et al. Clinicopathologic discrepancies in a population-based incidence study of parkinsonism in Olmsted county: 1991-2010. Mov. Disord. 32, 1439–1446 (2017).
Acknowledgements
This study was supported by the Parkinson’s Foundation with the support of the Parkinson’s community and their families. The work was also supported by USAMRAA W81XWH-07-1-0261 and W81XWH-13-1-0054 and a grant from the Michael J Fox Foundation to Caroline Tanner, PI. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of CIHI.
The Parkinson's Foundation P4 Group
Roy Alcalay, Michael Schwarzschild,Brad Racette, Honglei Chen, Tim Church, Bill Wilson and James M Doria.
Author information
Authors and Affiliations
Consortia
Contributions
All authors meet the following criteria for authorship: (1) Substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of the data; (2) Drafting the work or revising it critically for important intellectual content; (3) Final approval of the completed version; and (4) Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Other members of the Parkinson's Foundation P4 Group: Roy Alcalay, Michael Schwarzschild, Brad Racette, Honglei Chen, Tim Church, Bill Wilson, and James M Doria.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marras, C., Beck, J.C., Bower, J.H. et al. Prevalence of Parkinson’s disease across North America. npj Parkinson's Disease 4, 21 (2018). https://doi.org/10.1038/s41531-018-0058-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-018-0058-0
This article is cited by
-
An ensemble classification and binomial cumulative based PCA for diagnosis of parkinson’s disease and autism spectrum disorder
International Journal of System Assurance Engineering and Management (2024)
-
Exclusion of older patients from randomized clinical trials in Parkinson’s disease
GeroScience (2024)
-
Associating white matter microstructural integrity and improvements in reactive stepping in people with Parkinson’s Disease
Brain Imaging and Behavior (2024)
-
Development and internal validation of a prognostic model for loss of balance and falls in mid- to late-stage Parkinson’s disease
Neurological Sciences (2024)
-
The reciprocal interactions between microglia and T cells in Parkinson’s disease: a double-edged sword
Journal of Neuroinflammation (2023)