Abstract
Parkinson’s disease is a neurodegenerative disorder involving the basal ganglia that results in a host of motor and cognitive deficits. Dopamine-replacement therapy ameliorates some of the hallmark motor symptoms of Parkinson’s disease, but whether these medications improve deficits in response inhibition, a critical executive function for behavioral control, has been questioned. Several studies of Parkinson’s disease patients “on” and “off” (12-h withdrawal) dopaminergic medications suggested that dopamine-replacement therapy did not provide significant response inhibition benefits. However, these studies tended to include patients with moderate-to-advanced Parkinson’s disease, when the efficacy of dopaminergic drugs is reduced compared to early-stage Parkinson’s disease. In contrast, a few recent studies in early-stage Parkinson’s disease report that dopaminergic drugs do improve response inhibition deficits. Based on these findings, we hypothesized that Parkinson’s disease duration interacts with medication status to produce changes in cognitive function. To investigate this issue, we conducted a meta-analysis of studies comparing patients with Parkinson’s disease and healthy controls on tests of response inhibition (50 comparisons from 42 studies). The findings supported the hypothesis; medication benefited response inhibition in patients with shorter disease duration, whereas “off” medication, moderate deficits were present that were relatively unaffected by disease duration. These findings support the role of dopamine in response inhibition and suggest the need to consider disease duration in research of the efficacy of dopamine-replacement therapy on cognitive function in Parkinson’s disease.
Similar content being viewed by others
Introduction
Response inhibition, the ability to suppress a pre-potent or habitual behavioral response, is a critical executive function. Of the various cognitive deficits that patients with Parkinson’s disease (PD) experience (e.g., working memory, planning, and visuospatial attention), response inhibition is of particular importance for the recognition of its negative impact on quality of life.1,2,3,4 Loss of response inhibition is associated with motor symptom severity5 and freezing of gait, a particularly debilitating feature of the disease.6,7,8,9 With a close link to broader clinical deficits and prediction of later dementia,10 response inhibition performance has been posited as a sensitive outcome measure for diagnosis and progression of PD.11 Thus, great emphasis has been placed on understanding the neurochemical basis of this deficit, and in particular, the role of dopaminergic medication in response inhibition.
Earlier investigations probed the role of dopaminergic medications, including levodopa, during response inhibition paradigms. However, while seemingly improving other cognitive functions, including task switching and working memory,12,13,14 dopaminergic medications did not appear to provide significant response inhibition benefits to individuals with PD.15,16,17,18 Some studies in particular suggested that dopamine (DA) deficiency does not underlie poor response inhibition, but postulated a role of other neurotransmitters, such as noradrenaline and serotonin.19, 20 Several studies in humans and animals have provided some evidence suggesting that response inhibition is supported by neurotransmitters other than DA.21, 22 For instance, atomoxetine, a noradrenaline uptake inhibitor, provides benefit for response inhibition in healthy adults,23, 24 adults with attention-deficit hyperactivity disorder (ADHD),25 and individuals with PD.26,27,28 In PD, atomoxetine may exert its effects by increasing connectivity of prefrontal circuits critical for response inhibition.29 The serotonin-boosting drug citalopram has also shown some beneficial effects on response inhibition in PD.27, 30 Studies in rats have come to similar conclusions; while DA transporter inhibition had minor effects on Stop-signal task (SST) performance, atomoxetine improved the stop-signal reaction time (SSRT).22 In addition, a recent optogenetics study showed that non-DA cell bodies in the basal forebrain of rats were critical for implementing stopping behavior on the SST.21 Together, these studies question a unique role of DA in response inhibition.
However, studies of other specific populations and healthy adults suggests that DA deserves reconsideration in response inhibition. Several studies found that a single dose of methylphenidate (which boosts DA as well as noradrenaline) improved response inhibition behavior in individuals with ADHD,31 cocaine dependence32 and in healthy adults33, 34 (but see35, 36). More convincingly, PET studies have found that higher levels of striatal D1 and D2/D3 receptor availability predict better performance on the SST37, 38 and that response inhibition performance evokes DA release in prefrontal, parietal, and temporal cortex in healthy adults.39
How then, can we reconcile these divergent findings? An important starting place is to consider the characteristics of the PD populations that did not show significant response inhibition improvement with dopaminergic medication.15,16,17,18 Many previous studies typically include patients in the moderate-to-advanced stages of PD (i.e., individuals with Hoehn and Yahr rating >2 or studies with a wide range of disease duration). This is worth noting because of the profound DA loss in the later stages of PD, and the diminished efficacy of dopaminergic drugs when there are few remaining dopaminergic cells for the drugs to operate on.40 Indeed, recent studies provided evidence that early-stage patients with response inhibition impairment seem to benefit from DA treatment.41, 42 Thus, studies of patients with moderate-to-advanced PD may not be the best model for examining the role of dopaminergic medication effects on response inhibition.
To re-examine the effects of dopaminergic medications on response inhibition in PD with disease duration in consideration, we performed a meta-analysis of studies in PD populations that used several common response inhibition paradigms (the SST, Go-NoGo, Simon, Flanker, Stroop, and anti-saccade tasks) and looked for an interaction between disease duration and medication status on response inhibition performance while controlling for age effects. We expected to find that studies enrolling patients in the earlier stages (e.g., Hoehn & Yahr I and II or within several years of diagnosis) of PD would show the largest benefit of dopaminergic medication, and hence show performance that was less impaired relative to healthy controls.
Materials and methods
We performed a literature search using PubMed (www.ncbi.nlm.nih.gov/pubmed) to identify studies that compared a PD cohort with an age-matched healthy adult group on one of six common response inhibition tasks (Stop-Signal, Go-NoGo, Simon, Flanker, Stroop, and Antisaccade tasks). A systematic search up to September 2016 was conducted using the terms [(“Stop-Signal Task” OR “Stop Signal Task” OR “Go-NoGo” OR “Go NoGo” OR “GoNoGo” OR “Go/NoGo” OR “Go No-Go” OR “Antisaccade” OR “Anti-saccade” OR “Simon Task” OR “Flanker” OR “Stroop”) AND (Parkinson OR Parkinson’s)]. This initial search covered a range of studies dated from 1988 to 2016), and only included articles from peer-reviewed journals and written in English. This initial search yielded 305 results. An additional six studies were identified from previous knowledge and recursive reference searching.
We then searched through the text of the 311 studies to screen for: (1) review papers, case studies, book chapters or other non-original research papers; (2) evidence of dementia or surgical intervention; (3) no adequate age-matched control group; (4) atypical versions of the response inhibition tasks that mixed response inhibition with other behavioral contingencies or obvious additional cognitive demands (e.g., Go-NoGo tasks that had a reward component); (5) no information reported on medication status or disease duration for the PD group. Where possible, we included studies that had subsets of data meeting our inclusion criteria. For instance, some studies with a surgical intervention group had an additional PD cohort without surgery; if the non-surgical cohort met our inclusion criteria, we included data from only the non-surgical cohort.
Forty-seven comparisons from 40 studies remained following application of the exclusion criteria. Corresponding authors were contacted for studies that satisfied all other criteria but did not report sufficient statistics for response inhibition performance, and/or medication status and disease duration. This resulted in the addition of three more comparisons and two more studies. Thus, for the final analysis, data were extracted from 50 comparisons from 42 studies and entered into a spreadsheet (for the full flow-chart, see Fig. 1a). No studies of the Flanker Task or the Simon Task remained after screening for exclusion criteria; thus, we only report on studies of the Anti-Saccade (number of comparisons k = 13), Go-NoGo (k = 6), SST (k = 11), and Stroop tasks (k = 20). For analysis, we chose the primary outcome measure of each response inhibition task that was most often reported across studies: for the Anti-Saccade/Go-NoGo tasks, this was the commission error (false alarm) rate, for the SST, the SSRT, and for the Stroop task, the interference effect on response time (i.e., incongruent response time (RT) minus congruent RT; Fig. 1b). We coded studies based on whether patients were taking their dopaminergic medications (“on” medication) or if they underwent a medication washout of at least 12 h (“off” medication) prior to task performance. We also included the average disease duration (years since diagnosis) and mean age of the PD group in data analyses. We chose years since diagnosis as a measure of disease severity instead of Hoehn and Yahr staging for two reasons: first, Hoehn and Yahr staging is not a linear metric and therefore is not suitable for the linear regression analysis we employed (see section on meta-regression in methods below), and second, Hoehn and Yahr staging was not reported for 15 of the studies (and 17 of the 50 comparisons) used here.
We used Comprehensive Meta-Analysis software to perform the meta-analysis.43 As in previous studies in this field44 we used a random-effects model. We calculated the effect size (Hedges’ g) of mean between-group (PD vs. control) differences in response inhibition performance for each comparison, which corrects for within-study variance that, among other causes, can be a consequence of small sample size. We also assessed the heterogeneity (Q) and inconsistency (I2) across studies. Heterogeneity is the ratio of between-study to within-study variance, and inconsistency refers to the ratio of heterogeneity to total variance across studies, i.e. the percentage of heterogeneity that results from differences between studies.45 We used the PD vs. control comparisons instead of within-subject comparisons (i.e., direct comparison of patients “on” vs. “off” medications) because too few studies meeting our inclusion criteria reported data from an “on” vs. “off” manipulation (ten studies; see Supplementary Material for a preliminary analysis on these datasets).43
Further, we performed meta-regression46 to assess the relationship between disease duration and response inhibition performance in the “on” and “off” medication state. Meta-regression carries the same assumptions of a standard regression analysis, except that in the meta-regression here, each data point referred to the effect size of performance difference between the PD group and control group for an entire study, rather than, e.g., across-subject performance on a response inhibition task. Because effect sizes in this analysis were weighted by within-study variation, studies with the highest variability contributed the least to the regression model. In the final analysis, we performed two regressions: one that included the studies with patients “on” medication, and another regression with “off” medication studies. Both regressed average disease duration (years) on the effect size of response inhibition deficit (Hedges’ g). To assess the interaction between disease duration and medication status, we conducted a z-test to compare the slopes of the “on” and “off” regressions.47 We also conducted additional multiple regression analyses that were identical except that we included the average age of the PD group in each study as a covariate, to account for any potential effects of aging on response inhibition performance that may be independent of medication status and disease duration.48, 49 Finally, to account for a possible diminution effect (the finding that effect sizes tend to be larger in older studies and diminish with replication in more recent studies50) we performed additional multiple regression analyses while including publication year as a covariate. It would be useful to account for differences in drug dosage amounts across studies by including average levodopa dose equivalency values51 as a covariate in the multiple regression analysis; however, many studies do not report these values, and so we were unable to perform formal analysis on all 50 comparisons. Therefore, we performed an analysis on the subset of 14 studies reporting Levodopa-dose (LEDD, see Table 1 for a summary).
Data availability
The datasets analysed during the current study were acquired from the references listed in Table 1 and are available from the corresponding author on reasonable request.
Results
The final sample included 50 comparisons from 42 studies, which are described in Table 1.
To assess differences in response inhibition performance for PD on and off medication in comparison to healthy control, we extracted means and standard deviations from the PD and control groups from the critical outcome measure of each task: SSRT for the SST, false alarm rate for Go-NoGo and Anti-saccade tasks, and the Stoop interference effect (i.e., incongruent RT minus congruent RT); all outcome measures were continuous variables. For five studies of which standard deviations were not reported, we extracted the mean for each group, or the mean difference between groups, and the t-value or p-value of the PD vs. control comparison to calculate effect sizes. Table 1 describes the samples included from each study, including average age and disease duration of the PD group. Effect sizes for each comparison are shown in the Forest plot in Fig. 2. The average effect size for “on” and “off” samples was moderate and significant, suggesting that patient groups with PD showed response inhibition deficits relative to their matched controls (“off” Hedges’ g = −.86; “on” Hedges’ g = −.66; all studies; Hedges’ g = −.72, all p’s < 10−6). There was no significant difference in effect size between “on” and “off” samples, two-sample t-test: t(48) = .88, p = .38, and post-hoc t-tests indicated no significant “on” vs. “off” differences within any of the four tasks (all p’s > .05). The average effect size for the Anti-saccade (Hedges’ g = −.85), SST (Hedges’ g = −.75), and Stroop (Hedges’ g = −.72) tasks were moderate and significant (p’s < 10−6), while the average Go-NoGo effect size was not (Hedges’ g = −.35; p = .09). However, there was no significant difference in effect size across the four tasks; One-way analysis of variance: F(3,46) = 1.50; p = .23.
Forest plot of effect sizes for all studies that compared performance on a response inhibition task between a PD group and a matched healthy control group. a Studies sorted by medication status. b Studies sorted by task. Effect sizes to the left of the vertical dashed line indicate that performance of the PD group was poorer than controls. Note: Avg., Average; SST, Stop-Signal Task; GNG, Go-NoGo; A-S, Anti-Saccade
While the vast majority of studies reported poorer performance among the PD groups relative to each of their control group (48 out of 50 comparisons), effect sizes were variable across studies. We found 35 out of 50 studies that showed a significant effect size for PD vs control group differences in response inhibition performance. There was significant heterogeneity in the “off” and “on” samples (“off” sample: Q = 37.24, p < .001, I 2 = 65.09; “on” sample: Q = 57.07, p = .01, I 2 = 38.68), but heterogeneity did not significantly differ by medication status (Q = .47, p = .49). There was significant heterogeneity in the Anti-saccade (Q = 28.44, p < .01, I 2 = 57.80), Go-NoGo (Q = 11.61, p < .05, I 2 = 56.94) and Stroop tasks (Q = 34.90, p < .02, I 2 = 45.53), but not the SST (Q = 15.58, p = .11, I 2 = 35.83). However, heterogeneity did not significantly differ across the four tasks (Q = 4.26; p = .24).
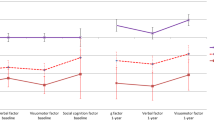
Next, we performed meta-regression to examine how the effect size of PD vs. control group differences in response inhibition varied across studies with relation to disease duration for each medication status. For “on” vs. control comparisons, the effect of disease duration was significant (z = −3.24, r 2 = .55, p = .001), while the effect was not significant for “off” vs. control comparisons (z = −0.84, r 2 = .00, p = .40; Fig. 3). In other words, in the “on” medication state, patients with longer average disease duration showed more severe response inhibition deficits, whereas the deficits were relatively unaffected by disease duration when patients were “off” dopaminergic medication. Disease duration thus explained more variance in response inhibition deficits across studies with participants “on” medication compared to the “off” medication studies, with the test for differences in slopes significant (z = −2.05, p = .04). The same pattern of disease duration effects remained even when age was controlled for in the regression analysis. Specifically, effect of age was not significant for both on and off medication state (z’s < 0.8, p’s > .42), with disease duration remaining significant in the “on” sample (z = −3.12, r 2 = .47, p = .002) but again not significant in the “off” sample (z = −.79, r 2 = .00, p = .43); the slope difference between “on” and “off” samples remained significant (z = −2.05, p = .04). To explore the potential role of medication dosage in the meta-regression results described above, we examined the association of LEDD for the 14 studies in the “on” state that included an average LEDD score. Such analysis showed negligible effects of LEDD when included in a model together with disease duration (effect of disease duration: z = −2.35, p = .018; effect of LEDD: z = 0.38, p = .705), or when simply including LEDD as the only predictor variable (z = 0.39, p = .70, R 2 = 0.00). There was a significant effect of publication date for both the “on” and “off” samples, such that earlier studies showed larger effect sizes between PD and controls (i.e., the diminution effect; z’s > 2.3, p’s < .05). However, including publication year as a covariate did not change the primary findings: the effect of disease duration remained significant in the “on” sample (z = −3.20, p = .001) and not significant in the “off” sample (z = .67, p = .51); and slope difference between “on” and “off” samples remained significant (z = −5.55, p < .001).
Regression plot of response inhibition deficits on average disease duration for the “off” medication (blue) and “on” medication (red) samples. Effect sizes less than 0 indicate that PD patients demonstrated poorer response inhibition performance than healthy controls. Each bubble represents a comparison from one study, weighted by within-study variance. Smaller bubbles represent studies with higher variance than others and thus, have less influence on the regression. The regression line of best fit for each sample is also shown. The difference in slopes was significant (z test; p = .04), indicating that “off” medication, deficits were moderate and relatively unaffected by disease duration, whereas “on” medication, deficits were significantly associated by disease duration. *p < .05; ***p = .001
Discussion
The primary results from the meta-analysis demonstrated that individuals with PD show deficits in response inhibition performance, specifically on tasks that test cognitive control of behavioral responses, including SST, Go-NoGo, Anti-saccade, and Stroop tasks. These deficits were of moderate effect size and significant for both the “on” and “off” medication samples, comparable to those in a previous meta-analysis examining a broader range of cognitive tasks in PD.44 However, our meta-analysis revealed a differential effect of dopaminergic medication status by disease duration on response inhibition performance across studies. Specifically, “off” medication, patient groups tended to show moderate deficits relative to controls regardless of disease duration, but “on” medication, disease duration predicted the severity of response inhibition deficit. Thus, in the earlier stages of PD, patients on dopaminergic medication tend to show performance that is more comparable to healthy control levels.
These results suggest that disease duration is an important factor when considering medication effects on response inhibition performance in PD. Previous work has compared dopaminergic effects on response inhibition directly within subjects “on” and “off” medication and emphasized null findings,15,16,17,18 but these studies tended to include patients with moderate to advanced PD (e.g., individuals with Hoehn & Yahr rating >2 or studies with a wide range of disease duration). We suggest that these studies observed no significant effects of DA-replacement therapy because of severe loss of dopaminergic midbrain cells in the later stages of PD.52, 53 It is routinely observed that dopaminergic drugs lose their efficacy in more advanced PD,40 putatively because diminishing numbers of DA cells render few targets for the drugs to exert their effects. Although the evidence is indirect, the current findings provide a starting point to suggest that the role of DA in response inhibition deserves reconsideration, particularly in early-stage PD. Thus, a critical next step is to directly test dopaminergic medication effects on response inhibition in a within-study design with patients in the early stages of PD.
It is important to consider the possibility that impulse control disorders may play a role in these findings. That is, advanced PD patients “on” medication show poor response inhibition due to increased likelihood of having impulse control disorders. It is estimated that 15–20% of individuals using dopaminergic medications long-term, especially DA agonists, are susceptible to developing impulse control problems over time.54 However, several lines of evidence suggest that impulse control problems would not be the most likely contributor to response inhibition deficits in PD. Recent studies have delineated separable neural and behavioral substrates of motivational vs. cognitive/motor impulsivity (e.g., gambling addiction vs. stop-signal inhibition55). While PD patients with impulse control disorders are prone to compulsive motivational behaviors including gambling, shopping, sex, and binge-eating,54 they do not demonstrate increased cognitive/motor impulsivity on the Stroop and SST compared to matched PD patients without impulse control disorder.56, 57 Further, acute withdrawal of dopaminergic medication did not help improve impulsive error rates relative to the “on” medication state in the Simon task.42, 58 Finally, although DA agonists specifically have been implicated in impulse control disorders in PD, a recent investigation by van Wouwe and colleagues42 found no significant differences on Simon task performance between PD groups on agonist monotherapy vs. levodopa monotherapy or combination therapy. Thus, the type of impulsivity described with long-term medication use in PD does not map on well to the type of impulsivity investigated in the response inhibition literature. Still, longitudinal studies are needed to determine more definitively whether long-term medication use impairs response inhibition in PD.
Our findings correspond with several recent studies that found an association between dopaminergic function and response inhibition performance in both healthy adults and clinical populations.31,32,33,34, 37,38,39 There are some notable exceptions, however: some studies in healthy adult humans59, 60 and rats22, 61 have found that pharmacologically manipulating DA transmission had minor effects on response inhibition performance. There are several possible explanations for these seemingly discrepant findings. For one, it is possible that there are subtle differences in how DA supports performance on different response inhibition tasks. Indeed, average response inhibition deficits in PD were fairly similar for Antisaccade, SST, and Stroop, but not Go-NoGo (average Hedges’ g: Antisaccade: −.85; Go-NoGo: −.35; SST: −.75; Stroop task: −.72), perhaps due to differences in task difficulty. For instance, no significant group differences were observed when accuracy was >95% for both groups in one Go-NoGo study,62 whereas SSRT deficits can be profound on challenging SSTs that induce roughly 50% error rates on stop trials2, 15; this is in accord with recent suggestions that Go-NoGo may not be sufficiently sensitive to detect response inhibition deficits in PD.11 While a previous meta-analysis demonstrated highly overlapping neural correlates of Go-NoGo and SST, differences were also noted;63 and others have also noted that response inhibition performance does not always correlate neatly between tasks,64 perhaps because of differences in task demand and/or performance strategy.11 Notably, effect sizes for the antisaccade task were large in our meta-analysis, despite the fact that this was the only task not requiring hand movements. Thus, response inhibition deficits in PD are not simply due to motor deficits in the most-affected extremities. Our findings that SST effect sizes were rather large and, compared to the other three tasks, had the least heterogeneity across studies, suggests that the SST may be a more sensitive task for identifying response inhibition deficits and drug effects. Another possible reasons for discrepant findings on DA’s role in response inhibition may be related to baseline levels of DA function. Previous attempts to boost DA transmission in healthy adults59, 60 might not improve response inhibition performance because most healthy adults should presumably already have optimal levels of DA to support task performance, based on the inverted U-shape theory of dopaminergic function in cognition.65 In support, Colzato et al.66 found that L-Tyrosine (DA precursor) administration improved SSRT only in the subset of healthy adults with the T/T polymorphism of the dopamine D2 receptor, which confers low levels of striatal DA. These considerations highlight the need for systematic assessment of DA’s role in response inhibition in various populations, using a variety of behavioral tasks and medication statuses.
While this meta-analysis suggests an association between dopaminergic medication and response inhibition performance, there is substantial evidence that other neurotransmitters also play a critical role in these behaviors in PD. Animal studies have found that drugs which alter noradrenaline and serotonin can have marked effects on response inhibition behavior.67 This has prompted researchers to find non-dopaminergic therapies for response inhibition deficits in PD. Recent studies have reported some success with noradrenergic and serotonergic drugs in SST performance in moderate-to-advanced PD.26, 27, 68 A current challenge is thus to find optimal combination therapies that might promote response inhibition in PD. Given the current findings on how disease duration interacts with DA-replacement therapy, it seems likely that medication regimes for cognition may need to be adjusted throughout the course of the disease. These results also highlight the therapeutic potential to restore the deteriorating dopaminergic system in PD69; our study suggests this might benefit response inhibition in addition to the primary motor symptoms of PD.
There are a number of limitations to acknowledge. While all meta-analyses must deal with many sources of heterogeneity across independent studies, studies of PD may involve additional sources of variance that cannot all be accounted for. The current study examined the role of disease duration and medication status in cognitive task performance, and controlled for the possible effects of age and publication date. Yet, many variables are not consistently reported could explain additional variance, such as drug type, dosage differences, motor subtype and global assessments of cognitive function. Future reports should strive to include levodopa dose equivalency values,51 as well as comprehensive data on motor (Unified Parkinson’s Disease Rating Scale70) and cognitive (e.g., Montreal Cognitive Assessment71) function to help account for these variables. Other clinical differences across patient groups may also obscure findings, such as levels of comorbid depression and fatigue, which are common in PD and may relate to response inhibition performance. Studies with “on” vs. “off” medication within-subject designs would be important, as they at least control for subject variability within studies. To date, there were insufficient numbers of these studies that met our inclusion criteria (k = 10) to perform the critical meta-analysis using within-subject comparisons (preliminary analyses on these data are reported in Supplementary Material, which are generally in line with the conclusions of the primary analysis presented here). In addition, it should be noted that “off” medication groups are typically defined by a 12-h washout procedure. While this is sufficient to produce significant differences in motor symptom severity from the medicated state, significant loss of motor function can continue for weeks after discontinuation of medication in early-stage PD.72 To our knowledge no studies have examined changes in response inhibition performance follow a similar timecourse with medication washout. Future work is needed to determine what the optimal washout duration is for probing dopaminergic function in response inhibition. Another limitation regards sample size. This is because we chose to select only studies that used relatively pure cognitive versions of response inhibition tasks, and hence could not report on the many studies that used variations on these paradigms, e.g. reward-based Go-NoGo tasks. Nonetheless, these findings supplement previous analyses44 that explored how dopaminergic medications are related to cognitive deficits in PD more broadly.
Overall, results from this meta-analysis suggest in PD, response inhibition deficits are least severe relative to controls when patients are in early-stages of PD and “on” dopaminergic medications. Deficits are more severe in later stages of PD “on” medications, and under medication withdrawal, regardless of disease duration. This pattern of findings provides indirect evidence that dopaminergic medications may support response inhibition in early-stage PD.
References
Schrag, A., Jahanshahi, M. & Quinn, N. What contributes to quality of life in patients with Parkinson’s disease? J. Neurol. Neurosurg. Psychiatry 69, 308–312 (2000).
Gauggel, S., Rieger, M. & Feghoff, T. Inhibition of ongoing responses in patients with Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 75, 539–544 (2004).
Muntean, M. L. & Perju-Dumbrava, L. The impact of non-motor symptoms on the quality of life of Parkinson’s disease patients. Eur. J. Neurol. 19, 685 (2012).
Lawson, R. A. et al. Cognitive decline and quality of life in incident Parkinson’s disease: The role of attention. Parkinsonism Relat. Disord. 27, 1–7 (2016).
Dujardin, K. et al. The spectrum of cognitive disorders in Parkinson’s disease: a data-driven approach. Mov. Disord. 28, 183–189 (2013).
Shine, J. M. et al. Freezing of gait in Parkinson’s disease is associated with functional decoupling between the cognitive control network and the basal ganglia. Brain 136, 3671–3681 (2013).
Walton, C. C. et al. Antisaccade errors reveal cognitive control deficits in Parkinson’s disease with freezing of gait. J. Neurol. 262, 2745–2754 (2015).
Lewis, S. J. G. & Barker, R. A. A pathophysiological model of freezing of gait in Parkinson’s disease. Parkinsonism Relat. Disord. 15, 333–338 (2009).
Vandenbossche, J. et al. Conflict and freezing of gait in Parkinson’s disease: support for a response control deficit. Neuroscience 206, 144–154 (2012).
Pedersen, K. F., Larsen, J. P., Tysnes, O.-B. & Alves, G. Prognosis of mild cognitive impairment in early Parkinson disease. JAMA Neurol. 70, 580–586 (2013).
MacDonald, H. J. & Byblow, W. D. Does response inhibition have pre-and postdiagnostic utility in Parkinson’s disease? J. Mot. Behav. 47, 29–45 (2015).
Cools, R., Stefanova, E., Barker, R. A., Robbins, T. W. & Owen, A. M. Dopaminergic modulation of high-level cognition in Parkinson’s disease: the role of the prefrontal cortex revealed by PET. Brain 125, 584–594 (2002).
Monchi, O., Petrides, M., Mejia-Constain, B. & Strafella, A. P. Cortical activity in Parkinson’s disease during executive processing depends on striatal involvement. Brain 130, 233–244 (2007).
Ekman, U. et al. Functional brain activity and presynaptic dopamine uptake in patients with Parkinson’s disease and mild cognitive impairment: a cross-sectional study. Lancet Neurol. 11, 679–687 (2012).
Alegre, M. et al. The subthalamic nucleus is involved in successful inhibition in the stop-signal task: a local field potential study in Parkinson’s disease. Exp. Neurol. 239, 1–12 (2013).
Obeso, I., Wilkinson, L. & Jahanshahi, M. Levodopa medication does not influence motor inhibition or conflict resolution in a conditional stop-signal task in Parkinson’s disease. Exp. Brain Res. 213, 435–445 (2011).
George, J. S. et al. Dopaminergic therapy in Parkinson’s disease decreases cortical beta band coherence in the resting state and increases cortical beta band power during executive control. Neuroimage Clin. 3, 261–270 (2013).
Campbell, M. C. et al. Neural correlates of STN DBS-induced cognitive variability in Parkinson disease. Neuropsychologia 46, 3162–3169 (2008).
Robbins, T. W. & Cools, R. Cognitive deficits in Parkinson’s disease: a cognitive neuroscience perspective. Mov. Disord. 29, 597–607 (2014).
Robbins, T. W. & Roberts, A. C. Differential regulation of fronto-executive function by the monoamines and acetylcholine. Cereb. Cortex 17, 151–160 (2007).
Mayse, J. D., Nelson, G. M., Avila, I., Gallagher, M. & Lin, S. Basal forebrain neuronal inhibition enables rapid behavioral stopping. Nat. Neurosci. 18, 1501–1508 (2015).
Bari, A., Eagle, D. M., Mar, A. C., Robinson, E. S. J. & Robbins, T. W. Dissociable effects of noradrenaline, dopamine, and serotonin uptake blockade on stop task performance in rats. Psychopharmacology (Berl). 205, 273–283 (2009).
Chamberlain, S. R. et al. Atomoxetine modulates right inferior frontal activation during inhibitory control: a pharmacological functional magnetic resonance imaging study. Biol. Psychiatry 65, 550–555 (2009).
Chamberlain, S. R. et al. Neurochemical modulation of response inhibition and probabilistic learning in humans. Science 311, 861–863 (2006).
Chamberlain, S. R. et al. Atomoxetine improved response inhibition in adults with attention deficit/hyperactivity disorder. Biol. Psychiatry 62, 977–984 (2007).
Kehagia, A. A. et al. Targeting impulsivity in Parkinson’s disease using atomoxetine. Brain 137, 1986–1997 (2014).
Ye, Z. et al. Selective serotonin reuptake inhibition modulates response inhibition in Parkinson’s disease. Brain 137, 1145–1155 (2014).
Rae, C. L. et al. Atomoxetine restores the response inhibition network in Parkinson’s disease. Brain 139, 2235–2248 (2016).
Borchert, R. J. et al. Atomoxetine enhances connectivity of prefrontal networks in Parkinson’s disease. Neuropsychopharmacology doi:10.1038/npp.2016.18 (2016).
Ye, Z. et al. Predicting beneficial effects of atomoxetine and citalopram on response inhibition in Parkinson’s disease with clinical and neuroimaging measures. Hum. Brain Mapp. 37, 1026–1037 (2016).
Aron, A. R., Dowson, J. H., Sahakian, B. J. & Robbins, T. W. Methylphenidate improves response inhibition in adults with attention-deficit/hyperactivity disorder. Biol. Psychiatry 54, 1465–1468 (2003).
Li, C.-S. R. et al. Biological markers of the effects of intravenous methylphenidate on improving inhibitory control in cocaine-dependent patients. Proc. Natl. Acad. Sci. USA 107, 14455–14459 (2010).
Nandam, L. S. et al. Methylphenidate but not atomoxetine or citalopram modulates inhibitory control and response time variability. Biol. Psychiatry 69, 902–904 (2011).
Ivanov, I. et al. Methylphenidate and brain activity in a reward/conflict paradigm: role of the insula in task performance. Eur. Neuropsychopharmacol. 24, 897–906 (2014).
Farr, O. M. et al. The effects of methylphenidate on cerebral activations to salient stimuli in healthy adults. Exp. Clin. Psychopharmacol. 22, 154–165 (2014).
Manza, P. et al. The effects of methylphenidate on cerebral responses to conflict anticipation and unsigned prediction error in a stop-signal task. J. Psychopharmacol. 3, 283–293 (2016).
Ghahremani, D. G. et al. Striatal dopamine D2/D3 receptors mediate response inhibition and related activity in frontostriatal neural circuitry in humans. J. Neurosci. 32, 7316–7324 (2012).
Robertson, C. L. et al. Striatal D1- and D2-type dopamine receptors are linked to motor response inhibition in human subjects. J. Neurosci. 35, 5990–5997 (2015).
Albrecht, D. S., Kareken, Da, Christian, B. T., Dzemidzic, M. & Yoder, K. K. Cortical dopamine release during a behavioral response inhibition task. Synapse 68, 266–274 (2014).
Bravi, D. et al. Wearing-off fluctuations in Parkinson’s disease: contribution of postsynaptic mechanisms. Ann. Neurol. 36, 27–31 (1994).
Costa, A. et al. Dopamine treatment and cognitive functioning in individuals with Parkinson’s disease: the ‘cognitive flexibility’ hypothesis seems to work. Behav. Neurol. 2014, 260896 (2014).
van Wouwe, N. C. et al. Dissociable effects of dopamine on the initial capture and the reactive inhibition of impulsive actions in Parkinson’s disease. J. Cogn. Neurosci. 28, 710–723 (2016).
Borenstein, M., Hedges, L., Higgins, J. & Rothstein, H. Comprehensive meta-analysis version 2. (Biostat, 2005).
Kudlicka, A., Clare, L. & Hindle, J. V. Executive functions in Parkinson’s disease: systematic review and meta-analysis. Mov. Disord. 26, 2305–2315 (2011).
Borenstein, M., Hedges, L. V., Higgins, J. P. T. & Rothstein, H. R. Identifying and quantifying heterogeneity. Introduction to Meta-Analysis. (John Wiley & Sons, 2009).
Houwelingen, H. C. Van, Arends, L. R. & Stijnen, T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat. Med. 21, 589–624 (2002).
Cohen, J., Cohen, P., West, S. G. & Aiken, L. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences 2nd edn (Hillsdale NJ Lawrence Erlbaum Associates, 2003).
Hu, S., Chao, H. H., Zhang, S., Ide, J. S. & Li, C.-S. R. Changes in cerebral morphometry and amplitude of low-frequency fluctuations of BOLD signals during healthy aging: correlation with inhibitory control. Brain Struct. Funct. 219, 983–994 (2014).
Manza, P. et al. The effects of age on resting state functional connectivity of the basal ganglia from young to middle adulthood. Neuroimage 107, 311–322 (2015).
Ioannidis, J. P. Contradicted and initially stronger effects in highly cited clinical research. JAMA. 294, 218–228 (2005).
Tomlinson, C. L. et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 25, 2649–2653 (2010).
Damier, P., Hirsch, E., Agid, Y. & Graybiel, A. The substantia nigra of the human brain II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain 122, 1437–1448 (1999).
Kish, S., Shannak, K. & Hornykiewicz, O. Uneven pattern of dopamine loss in the striatum of patients with idiopathic Parkinson’s disease. N. Engl. J. Med. 318, 876–880 (1988).
Weintraub, D., Siderowf, A. D. & Whetteckey, J. Impulse control disorders in Parkinson disease. Arch. Neurol. 67, 589–595 (2010).
Bari, A. & Robbins, T. W. Inhibition and impulsivity: behavioral and neural basis of response control. Prog. Neurobiol. 108, 44–79 (2013).
Claassen, D. O. et al. Proficient motor impulse control in Parkinson disease patients with impulsive and compulsive behaviors. Pharmacol. Biochem. Behav. 129, 19–25 (2015).
Djamshidian, A., O’Sullivan, S. S., Lees, A. & Averbeck, B. B. Stroop test performance in impulsive and non impulsive patients with Parkinson’s disease. Parkinsonism Relat. Disord. 17, 212–214 (2011).
Wylie, S. A. et al. Dopamine agonists and the suppression of impulsive motor actions in Parkinson disease. J. Cogn. Neurosci. 24, 1709–1724 (2012).
Hershey, T. et al. Dopaminergic modulation of response inhibition: an fMRI study. Brain Res. Cogn. Brain Res. 20, 438–448 (2004).
Costa, A. et al. Methylphenidate effects on neural activity during response inhibition in healthy humans. Cereb. Cortex 23, 1179–1189 (2013).
Eagle, D. M., Tufft, M. R. A., Goodchild, H. L. & Robbins, T. W. Differential effects of modafinil and methylphenidate on stop-signal reaction time task performance in the rat, and interactions with the dopamine receptor antagonist cis-flupenthixol. Psychopharmacology (Berl). 192, 193–206 (2007).
Tachibana, H., Aragane, K., Miyata, Y. & Sugita, M. Electrophysiological analysis of cognitive slowing in Parkinson’s disease. J. Neurol. Sci. 149, 47–56 (1997).
Swick, D., Ashley, V. & Turken, U. Are the neural correlates of stopping and not going identical? Quantitative meta-analysis of two response inhibition tasks. Neuroimage 56, 1655–1665 (2011).
Wager, T. D. et al. Common and unique components of response inhibition revealed by fMRI. Neuroimage 27, 323–340 (2005).
Cools, R. & D’Esposito, M. Inverted-u-shaped dopamine actions on human working memory and cognitive control. Biol. Psychiatry 69, e113–e125 (2011).
Colzato, L. S. et al. Effects of l-Tyrosine on working memory and inhibitory control are determined by DRD2 genotypes: a randomized controlled trial. Cortex 82, 217–224 (2016).
Eagle, D. M. & Baunez, C. Is there an inhibitory-response-control system in the rat? Evidence from anatomical and pharmacological studies of behavioral inhibition. Neurosci. Biobehav. Rev. 34, 50–72 (2010).
Ye, Z. et al. Improving response inhibition in Parkinson’s disease with atomoxetine. Biol. Psychiatry 77, 740–748 (2014).
Li, W. et al. Extensive graft-derived dopaminergic innervation is maintained 24 years after transplantation in the degenerating parkinsonian brain. Proc. Natl. Acad. Sci. doi:10.1073/pnas.1605245113 (2016).
Goetz, C. G. et al. Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): process, format, and clinimetric testing plan. Mov. Disord. 22, 41–47 (2007).
Nasreddine, Z. & Phillips, N. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005).
Hauser, R. A. & Holford, N. H. G. Quantitative description of loss of clinical benefit following withdrawal of levodopa-carbidopa and bromocriptine in early Parkinson’s disease. Mov. Disord. 17, 961–968 (2002).
Amador, S. C., Hood, A. J., Schiess, M. C., Izor, R. & Sereno, A. B. Dissociating cognitive deficits involved in voluntary eye movement dysfunctions in Parkinson’s disease patients. Neuropsychologia 44, 1475–1482 (2006).
Briand, K. A., Strallow, D., Hening, W., Poizner, H. & Sereno, A. B. Control of voluntary and reflexive saccades in Parkinson’s disease. Exp. Brain Res. 129, 38–48 (1999).
Hood, A. J. et al. Levodopa slows prosaccades and improves antisaccades: an eye movement study in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 78, 565–570 (2007).
Lemos, J. et al. Distinct functional properties of the vertical and horizontal saccadic network in Health and Parkinson’s disease: an eye-tracking and fMRI study. Brain Res. 1648, 469–484 (2016).
Nemanich, S. T. & Earhart, G. M. Freezing of gait is associated with increased saccade latency and variability in Parkinson’s disease. Clin. Neurophysiol. 127, 2394–2401 (2016).
Cohen, R. G. et al. Inhibition, executive function, and freezing of gait. J. Parkinson’s Dis. 4, 111–122 (2014).
Farid, K. et al. Brain dopaminergic modulation associated with executive function in Parkinson’s disease. Mov. Disord. 24, 1962–1969 (2009).
Bohnen, N. I. et al. Cognitive correlates of cortical cholinergic denervation in Parkinson’s disease and parkinsonian dementia. J. Neurol. 253, 242–247 (2006).
Fera, F. et al. Dopaminergic modulation of cognitive interference after pharmacological washout in Parkinson’s disease. Brain Res. Bull. 74, 75–83 (2007).
Bonnet, C. et al. Eye movements in ephedrone-induced parkinsonism. PLoS One 9, e104784 (2014).
Cameron, I. G. M., Watanabe, M., Pari, G. & Munoz, D. P. Executive impairment in Parkinson’s disease: response automaticity and task switching. Neuropsychologia 48, 1948–1957 (2010).
Harsay, H. A., Buitenweg, J. I. V., Wijnen, J. G., Guerreiro, M. J. S. & Ridderinkhof, K. R. Remedial effects of motivational incentive on declining cognitive control in healthy aging and Parkinson’s disease. Front. Aging Neurosci. 2, 1–12 (2010).
Rivaud-Péchoux, S., Vidailhet, M., Brandel, J. P. & Gaymard, B. Mixing pro- and antisaccades in patients with parkinsonian syndromes. Brain 130, 256–264 (2007).
van Koningsbruggen, M. G., Pender, T., Machado, L. & Rafal, R. D. Impaired control of the oculomotor reflexes in Parkinson’s disease. Neuropsychologia 47, 2909–2915 (2009).
van Stockum, S., MacAskill, M., Anderson, T. & Dalrymple-Alford, J. Don’t look now or look away: two sources of saccadic disinhibition in Parkinson’s disease? Neuropsychologia 46, 3108–3115 (2008).
O’Callaghan, C., Naismith, S. L., Hodges, J. R., Lewis, S. J. G. & Hornberger, M. Fronto-striatal atrophy correlates of inhibitory dysfunction in parkinson’s disease versus behavioural variant frontotemporal dementia. Cortex 49, 1833–1843 (2013).
Stefanova, E. et al. Attentional set-shifting in Parkinson’s disease patients with freezing of gait-acquisition and discrimination set learning deficits at the background? J. Int. Neuropsychol. Soc. 20, 929–936 (2014).
A’Campo, L. E. I., Wekking, E. M., Spliethoff-Kamminga, N. G. A., Stijnen, T. & Roos, R. A. C. Treatment effect modifiers for the patient education programme for Parkinson’s disease. Int. J. Clin. Pract. 66, 77–83 (2012).
Bohlhalter, S., Abela, E., Weniger, D. & Weder, B. Impaired verbal memory in Parkinson disease: relationship to prefrontal dysfunction and somatosensory discrimination. Behav. Brain Funct. 5, 49 (2009).
Brown, R. G. & Marsden, C. D. Internal versus external cues and the control of attention in Parkinson’s disease. Brain 111, 323–345 (1988).
Hanes, K. R., Andrewes, D. G., Smith, D. J. & Pantelis, C. A brief assessment of executive control dysfunction: discriminant validity and homogeneity of planning, set shift, and fluency measures. Arch. Clin. Neuropsychol. 11, 185–191 (1996).
Hsieh, Y.-H., Chen, K.-J., Wang, C.-C. & Lai, C.-L. Cognitive and motor components of response speed in the stroop test in Parkinson’s disease patients. Kaohsiung. J. Med. Sci. 24, 197–203 (2008).
Kierzynka, A., Kaźmierski, R. & Kozubski, W. Educational level and cognitive impairment in patients with Parkinson disease. Neurol. Neurochir. Pol. 45, 24–31 (2011).
McNamara, P., Durso, R., Brown, A. & Lynch, A. Counterfactual cognitive deficit in persons with Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 74, 1065–1070 (2003).
Müller-Oehring, E. M. et al. Task-rest modulation of basal ganglia connectivity in mild to moderate Parkinson’s disease. Brain Imaging Behav. 9, 619–638 (2015).
Ranchet, M., Paire-Ficout, L., Marin-Lamellet, C., Laurent, B. & Broussolle, E. Impaired updating ability in drivers with Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 82, 218–223 (2011).
Ranchet, M. et al. Impact of specific executive functions on driving performance in people with Parkinson’s disease. Mov. Disord. 28, 1941–1948 (2013).
Relja, M. & Klepac, N. A dopamine agonist, pramipexole, and cognitive functions in Parkinson’s disease. J. Neurol. Sci. 248, 251–254 (2006).
Wild, L. B. et al. Characterization of cognitive and motor performance during dual-tasking in healthy older adults and patients with Parkinson’s disease. J. Neurol. 260, 580–589 (2013).
Witt, K. et al. Patients with Parkinson’s disease learn to control complex systems-an indication for intact implicit cognitive skill learning. Neuropsychologia 44, 2445–2451 (2006).
Woodward, T. S., Bub, D. N. & Hunter, M. A. Task switching deficits associated with Parkinson’s disease reflect depleted attentional resources. Neuropsychologia 40, 1948–1955 (2002).
Acknowledgements
The authors thank Drs. Anne Moyer, Turhan Canli, and Christian Luhmann for their helpful comments and suggestions. This study was funded by the Stony Brook Research Foundation.
Author information
Authors and Affiliations
Contributions
P.M. and H.-C.L. conceived and designed the study. P.M. conducted statistical analysis and wrote the first draft of the manuscript. M.A. and V.T. compiled and organized the data to conduct the meta-analysis. C.-S.R.Li. and H.-C.L. co-wrote and critiqued the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manza, P., Amandola, M., Tatineni, V. et al. Response inhibition in Parkinson’s disease: a meta-analysis of dopaminergic medication and disease duration effects. npj Parkinson's Disease 3, 23 (2017). https://doi.org/10.1038/s41531-017-0024-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-017-0024-2
This article is cited by
-
Impulsivity traits and awareness of motor intention in Parkinson’s disease: a proof-of-concept study
Neurological Sciences (2022)
-
Essential tremor impairs the ability to suppress involuntary action impulses
Experimental Brain Research (2022)