Abstract
The importance of integrating biomarkers into the TNM staging has been emphasized in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging system. In a pooled analysis of 2148 TNBC-patients in the adjuvant setting, TILs are found to strongly up and downstage traditional pathological-staging in the Pathological and Clinical Prognostic Stage Groups from the AJJC 8th edition Cancer Staging System. This suggest that clinical and research studies on TNBC should take TILs into account in addition to stage, as for example patients with stage II TNBC and high TILs have a better outcome than patients with stage I and low TILs.
Similar content being viewed by others
Introduction
The importance of integrating biomarkers into the TNM staging has been emphasized in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging System (www.cancerstaging.org). Prognostic biomarkers are becoming increasingly important given that many low early-stage breast cancer patients have excellent outcomes with standard of care treatments. The clinical guidelines for systemic treatment in early-stage TNBC are not consistent. The evidence for the integration of biomarkers into the TNM staging system is mostly retrospective and with limited prospective data available1. In the case of multigene panels, their clinical validity for defining prognosis of particular subgroups of patients had been shown in several retrospective analyses and these were routinely used and incorporated into national (NCCN and ASCO) and international (ESMO, St Gallen) treatment guidelines far before prospective data became available. In the 8th edition of the AJCC, histologic grading, molecular subtype (luminal, HER2-positive, and triple negative [TN]) and multigene panels/genomic signatures were included into staging assessments. Whilst pathological and clinical stage remain a valuable aspect of the staging process and are strongly prognostic, we highlight here the evidence that supports Tumor Infiltrating Lymphocytes (TILs) as a biologic biomarker which improves discrimination over prognostic pathological and clinical staging for early stage TNBC.
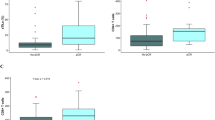
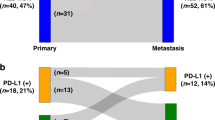
A recent pooled analysis provides the relevant work for integrating TIL quantity into clinical staging for early-stage TNBC (JCO 2019)2. These data were from 2148 patients enrolled onto eight prospective clinical trials as well as one large institutional cohort. All patients had received anthracyclines with or without taxanes based regimens in the adjuvant setting. The median follow-up was 6.6 years. In the current study, using the Pathological and Clinical Prognostic Stage Groups from the AJJC 8th edition Cancer Staging Manual (for definitions hereof, see footnote*), three endpoints were calculated for each Stage group: invasive disease-free survival (iDFS), distant disease-free survival (D-DFS) as well as overall survival (OS). At a cut-point of 30% or more, TIL scores are found to strongly up and downstage traditional pathological-staging in this large data set (Fig. 1, Supp Table 1). This suggest that clinical and research studies on TNBC should take TILs into account in addition to stage, as patients with stage II TNBC and high TILs have a better outcome than patients with stage I and low TILs. Importantly, histological grade is not prognostic in this pooled analysis. At the established prognostic cut-off of 30%, trained pathologists have a high pairwise concordance rate up to 0.93 using both core-biopsies as well as full sections, indicating that TILs are a reliable biomarker that can be used in daily practice and in research and clinical trial settings3. This compares favorably to the reproducibility of other commonly used morphological features in breast cancer practice4. Similarly, adding TILs to clinical staging is shown to up- and downstage prognostic groups which also take subtype into consideration (Fig. 2; Supp Table 2) though we note the small numbers in some of the subgroups (ie Stage IIA).
Pathological Prognostic Stage is assigned stage for patients who have surgical resection as the initial treatment of their cancer before receipt of any systemic or radiation therapy. It is based on clinical information, biomarker data, and findings from surgery and resected tissue. The 5-year estimated overall survival values (5-Yr OS) are provided together with bootstrap confidence intervals.
Clinical prognostic stage assigned stage for all patients based on history, physical examination, imaging studies performed (but not required) and relevant biopsies. Clinical prognostic stage is determined by T, N, M, tumor grade, as well as subtype information using human epidermal growth factor receptor (HER2), estrogen receptor (ER), and progesterone receptor (PR)- status. Supplementary Tables 1 and 2.
Risk assessment models meeting the AJCC criteria and included in the 8th Edition were Adjuvant Online and PREDICT-Plus. We have developed a prognostic model for early-stage disease that includes age, number of positive lymph nodes, tumor size, grade, and stromal TIL percentage. This prognostic model is available on the website of the International Immuno-Oncology Biomarker Working Group (www.tilsinbreastcancer.org). This prognostic model could be used in routine patient care as well as future trial designs.
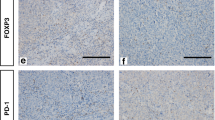
The inclusion of immune biomarkers is timely given reporting of phase III registration trials of PD-1/PD-L1 targeting agents in early-stage TNBC. In the recently reported KEYNOTE-522 study (NCT03036488)5, pembrolizumab, a PD-1 inhibitor, was found to significantly but moderately increase the rates of pathological complete response (pCR) and significantly improve event-free survival (EFS) when added to a neoadjuvant regimen of anthracycline, taxanes and carboplatin in patients with stage II and III TNBC. Similar magnitude of EFS improvements have been reported in smaller studies6,7. PD-L1 protein is known to be highly expressed on the breast cancer TIL and correlations between both markers have been observed8. In the KEYNOTE-522 study, patients designated as PD-L1 positive by the PD-L1 IHC 22C3 pharmdDx assay (Agilent Technologies, Carpinteria, CA, USA) were reported to have higher rates of pCR in both pembrolizumab and control arms across all TNM stages. An important treatment by PD-L1 interaction was not observed, in contrast to late-stage disease9,10. In any case, the increasing incorporation of PD-1 inhibition into the treatment of both early- and late stage TNBC further reinforces the need for routine evaluation of TIL in all TNBC patients, particularly given discordances in PD-L1 IHC assays. One could also speculate that patients with high expression of both immune biomarkers, i.e. those “immune enriched” could be strong candidates for future treatment optimization (for example, reduced cytotoxic chemotherapy)11.
Methods
This is a follow-up analysis of the Loi et al 2019 study2. The study protocol of this project was approved by the local institutional review committee at Gustave Roussy in November 2014 and authorized by the French National Committee on Computing and Liberty. Identified studies were prospective randomized clinical trials or large retrospective hospital series that evaluated the prognostic associations of TILs in patients who were diagnosed with early-stage TNBC treated with anthracycline-based chemotherapy with or without taxane in the adjuvant setting using the same prespecified method for reading TILS (according to International Immuno-Oncology Biomarker Working Group guidelines). TNBC was defined by estrogen receptor (ER), progesterone receptor (PR), and HER2 negativity as outlined in Loi et al. (ref).
The prespecified primary end point was invasive disease-free survival (iDFS), defined as the date of first invasive recurrence, or second primary or death from any cause. Patients still alive without an event of interest were censored at the date of the last visit. Distant disease-free survival (D-DFS) is defined as the date of first distant recurrence or death from any cause. Patients still alive without an event of interest were censored at the date of the last visit. Overall survival (OS) was defined as the date of death from any cause. Patients still alive were censored at the date of the last visit. We used the Kaplan-Meier method to establish survival curves according to AJCC staging categories. The Kaplan–Meier estimates are provided together with bootstrap confidence intervals (1000 samples).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Trial data can be made available by contacting the individual trial investigators of the trials included in this project, pending individual sponsors approval. The corresponding author of the paper can redirect requests. A specific data transfer agreement between the individual sponsors of the trials and the researcher may be requested. This data transfer agreement details both parts responsibilities to ensure the required level of data integrity and legal and ethical obligations.
References
Murthy, R. K. et al. Incorporation of clinical and biological factors improves prognostication and reflects contemporary clinical practice. NPJ Breast Cancer 6, 1–9 (2020).
Loi, S. et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J. Clin. Oncol. 37, 559 (2019).
Kos, Z. et al. Pitfalls in assessing stromal tumor infiltrating lymphocytes (sTILs) in breast cancer. NPJ Breast Cancer 6, 1–6 (2020).
Gilchrist, K. W. et al. Interobserver reproducibility of histopathological features in stage II breast cancer. Breast Cancer Res. Treat. 5, 3–10 (1985).
Schmid, P. et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 382, 810–821 (2020).
Mittendorf, E. et al. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. Lancet Oncol. 396, 1090–1100 (2020).
Loibl, S. et al. Durvalumab improves long-term outcome in TNBC: results from the phase II randomized GeparNUEVO study investigating neodjuvant durvalumab in addition to an anthracycline/taxane based neoadjuvant chemotherapy in early triple-negative breast cancer (TNBC). J. Clin. Oncol. 39, 506–506 (2021).
Loi, S. et al. Relationship between tumor infiltrating lymphocyte (TIL) levels and response to pembrolizumab (pembro) in metastatic triple-negative breast cancer (mTNBC): Results from KEYNOTE-086. Ann. Oncol. 28, p.v608 (2017).
Loi, S. et al. Abstract PD5-03: relationship between tumor-infiltrating lymphocytes (TILs) and outcomes in the KEYNOTE-119 study of pembrolizumab vs chemotherapy for previously treated metastatic triple-negative breast cancer (mTNBC). Cancer Res. 80, PD5–PD03 (2020).
Schmid, P. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N. Engl. J. Med. 379, 2108–2121 (2018).
Gonzalez‐Ericsson, P. I. et al. The path to a better biomarker: application of a risk management framework for the implementation of PD‐L1 and TILs as immuno‐oncology biomarkers in breast cancer clinical trials and daily practice. J. Pathol. 250, 667–684 (2020).
Acknowledgements
S.L. is supported by National Breast Cancer Foundation of Australia (NBCF) and the Breast Cancer Research Foundation (BCRF), NY, USA. RS is supported by the Breast Cancer Research Foundation (BCRF), NY, US. M.L.-T., J.L., F.A. and S.M. are supported by ANR and CGI (RHU MyPROBE and ANR-17-RHUS-0008).
Author information
Authors and Affiliations
Contributions
Conception and design: S.L., S.M. and R.S. Provision of study materials or patients: all. Collection and assembly of data: all. Data analysis and interpretation: all. Manuscript writing and final approval: all.
Corresponding author
Ethics declarations
Competing interests
S.L. receives research funding to her institution from Novartis, Bristol Meyers Squibb, Merck, Puma Biotechnology, Eli Lilly, Nektar Therapeutics Astra Zeneca, Roche-Genentech and Seattle Genetics. S.L. has acted as consultant (not compensated) to Seattle Genetics, Novartis, Bristol Meyers Squibb, Merck, AstraZeneca and Roche-Genentech. S.L. has acted as consultant (paid to her institution) to Aduro Biotech, Novartis, GlaxoSmithKline, Roche-Genentech, Astra Zeneca, Silverback Therapeutics, G1 Therapeutics, Daiichi Sankyo, PUMA Biotechnologies, Seattle Genetics and Bristol Meyers Squibb. RS reports non-financial support from Merck and Bristol Myers Squibb; research support from Merck, Puma Biotechnology, and Roche; and personal fees from Roche for an advisory board related to a trial-research project. S.D. has received honorarium as a member of the scientific advisory board of Lytix Biopharma, and ad hoc consulting for Ono Pharmaceuticals. M.P. is a Scientific Board Member of Oncolytics. M.P. has acted as a consultant (compensated) to AstraZeneca, Camel-IDS/Precirix, Gilead, Immunomedics, Lilly, Menarini, MSD, Novartis, Odonate, Pfizer, Roche-Genentech, Seattle Genetics, Immutep, Seagen, NBE Therapeutics, Frame Therapeutics. M.P. receives research funding to her institution from AstraZeneca, Immunomedics, Lilly, Menarini, MSD, Novartis, Pfizer, Radius, Roche-Genentech, Servier, Synthon. E.M. has acted as a consultant (compensated) to Pierre Fabre, Genomic Health and Eisai. E.M. has received funding for travel expenses and/or accommodation from Celgene, Roche, Eisai, Mylan and Pfizer. C.D. reports stock and other ownership interests from Sividon Diagnostics (unitl 2016), honoraria from Novartis and Roche. C.D. has acted as a consultant (compensated) to MSD Oncology, Daiichi Sankyo, Molecular Health, Astra Zeneca, merck. C.D. receives research funding (to institution) from Myriad Genetics and Roche. C.D. reports patents, royalties and/or other intellectual property from VMScope digital pathology software, patent applications WO2015114146A1 and WO2010076322A1(therapy response) and WO2020109570A1 (cancer immunotherapy). C.D. has received funding for travel expenses and/or accommodation from Roche. H.J. is the Chair of the Scientific Advisory Board at Orion Pharma and at Neutron Therapeutics Ltd. S.M. reports fees outside the submitted work from statistical advice (IDDI, Janssen Cilag, Amaris, Roche) and from data and safety monitoring membership of clinical trials (Hexal, Steba, IQVIA, Sensorion, Biophytis, Servier, Yuhan. F.A. received research funding and served as speaker / advisor (compensated to the hospital) for Roche, AstraZeneca, Daiichi Sankyo, Pfizer, Novartis, Lilly. S.A. has uncompensated consulting or advisory roles with Bristol Meyers Squibb, Genentech, and Merck as well as research funding to her institution from Amgen, Bristol Meyers Squibb, Celgene, Genentech, Merck and Novartis. M.V.D. reports personal fees for consultancy/advisory from Eli Lilly, Pfizer, Novartis, Genomic Health. MLT reports honorarium/expertise from Roche, Roche Diagnostics, MSD, AstraZeneca, Daiichi Sankyo. P.L.K.L. has received honorarium as member of advisory board of Bristol Myers Squibb and has received compensation for traveling from Sanofi. PAF reports honoraria from AstraZeneca and Novartis and travel support from Pfizer and Ipsen. The remaining authors declare competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Loi, S., Salgado, R., Adams, S. et al. Tumor infiltrating lymphocyte stratification of prognostic staging of early-stage triple negative breast cancer. npj Breast Cancer 8, 3 (2022). https://doi.org/10.1038/s41523-021-00362-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-021-00362-1
This article is cited by
-
High tumor infiltrating lymphocytes are significantly associated with pathological complete response in triple negative breast cancer treated with neoadjuvant KEYNOTE-522 chemoimmunotherapy
Breast Cancer Research and Treatment (2024)
-
The prognostic value of tumour-infiltrating lymphocytes, programmed cell death protein-1 and programmed cell death ligand-1 in Stage I–III triple-negative breast cancer
British Journal of Cancer (2023)
-
Single-cell profile of tumor and immune cells in primary breast cancer, sentinel lymph node, and metastatic lymph node
Breast Cancer (2023)
-
Immunotherapy in Early-Stage Triple-Negative Breast Cancer: Where Are We Now and Where Are We Headed?
Current Treatment Options in Oncology (2023)
-
Integrative prognostic analysis of tumor–infiltrating lymphocytes, CD8, CD20, programmed cell death-ligand 1, and tertiary lymphoid structures in patients with early-stage triple-negative breast cancer who did not receive adjuvant chemotherapy
Breast Cancer Research and Treatment (2023)