Abstract
Achromobacter xylosoxidans has attracted increasing attention as an emerging pathogen in patients with cystic fibrosis. Intrinsic resistance to several classes of antimicrobials and the ability to form robust biofilms in vivo contribute to the clinical manifestations of persistent A. xylosoxidans infection. Still, much of A. xylosoxidans biofilm formation remains uncharacterized due to the scarcity of existing genetic tools. Here we demonstrate a promising genetic system for use in A. xylosoxidans; generating a transposon mutant library which was then used to identify genes involved in biofilm development in vitro. We further described the effects of one of the genes found in the mutagenesis screen, encoding a putative enoyl-CoA hydratase, on biofilm structure and tolerance to antimicrobials. Through additional analysis, we find that a fatty acid signaling compound is essential to A. xylosoxidans biofilm ultrastructure and maintenance. This work describes methods for the genetic manipulation of A. xylosoxidans and demonstrated their use to improve our understanding of A. xylosoxidans pathophysiology.
Similar content being viewed by others
Introduction
Cystic fibrosis (CF) is caused by mutations in the gene encoding the cystic fibrosis transmembrane conductance regulator (CFTR) protein that resides at the apical surface of many epithelial cell types. CFTR defects result in abnormal chloride and bicarbonate transport, increasing mucus viscosity in the pancreas, paranasal sinuses, digestive tract, and most notably, the lower airways. Viscous mucus, due to its impaired clearance and abundant nutrient bioavailability, in turn becomes chronically colonized by pathogenic bacteria that are the leading cause of mortality among the CF population.1 For decades, Pseudomonas aeruginosa and Staphylococcus aureus have been extensively characterized and recognized as the primary airway pathogens. More recently, however, many other multidrug-resistant opportunistic bacterial species have received attention for their association with CF disease progression.2
Among them, Achromobacter xylosoxidans is notable given its association with poor pulmonary function scores and apparent patient-to-patient transmissibility.3,4,5 This aerobic, Gram-negative opportunistic pathogen has been found to colonize anywhere from 2 to 20 percent of CF subjects, though its prevalence has risen in recent years,4,6,7,8,9,10,11 sparking a renewed interest in its pathophysiology. Of particular concern is the intrinsic and acquired resistance of A. xlyosoxidans to multiple classes of antimicrobial agents, including aminoglycosides, beta-lactams, carbapenems, chloramphenicol and fluoroquinolones, which presents a significant burden for infection control.7,8,12,13,14,15
Also complicating treatment of A. xylosoxidans is its ability to form robust biofilms.16,17,18 Thought to be the predominant in vivo lifestyle among CF pathogens,19 biofilms confer a highly protective growth environment that shields pathogens against environmental stress, antimicrobials and the host immune response.20 In addition, nutrient and oxygen gradients throughout microcolonies (or aggregates)16 result in slowed metabolism among biofilm cells which can also potentiate drug tolerance. The recalcitrance of biofilm cells to antibiotic exposure likely enhances the persistence of A. xylosoxidans during chronic infection of the CF lung.
Relative to canonical CF pathogens, comparatively little is known about the molecular mechanisms of biofilm formation and maintenance in A. xylosoxidans. This is due, in part, to the paucity of genetic tools available for manipulation of its genome. Therefore, the objectives of this study were two-fold: First, we sought to develop a tractable system to genetically manipulate A. xylosoxidans. Using this system, our second objective was to take a transposon mutagenesis approach to study the molecular basis of A. xylosoxidans biofilm formation. In doing so, we identified several gene products essential for biofilm development. We chose to further characterize a gene identified most frequently in our screen (echA) encoding a putative enoyl-CoA hydratase that, when disrupted, leads to a decrease in biofilm accumulation and increased susceptibility to multiple classes of antibiotics.
Results
Identification of biofilm-defective mutants via transposon mutagenesis
To identify genetic determinants of biofilm formation in A. xylosoxidans, we generated a mutant library of strain MN001 using random transposon mutagenesis employing the mini-mariner transposable element.21 From this library, 15,000 mutants were screened for altered biofilm formation using an established crystal violet (CV)/microtiter dish assay.22 After an initial round of screening, 134 putative biofilm-defective mutants were identified that were then re-tested (n = 4) to verify mutant phenotypes. After secondary screening and eliminating mutants with general growth defects, 31 transposon mutants were confirmed to be defective in biofilm accumulation (Fig. 1, Table 1).
To identify DNA sequences (~200–400 bp) flanking transposon insertion junctions, mutants were screened by arbitrarily primed PCR. Insertions were mapped to loci predicted to encode various classes of gene products, including membrane proteins, glycosyltransferases, flagella, transcriptional regulators, in addition to several proteins with no assigned function (Table 1). Arbitrary PCR of three transposon insertion loci generated sequences with no homology to published gene sequences, and we were unable to obtain transposon-flanking sequences for five additional mutants. Of note, a putative enoyl-CoA hydratase, an exonuclease, and a propionate hydroxylase were each hit multiple times. We took interest in the gene encoding a putative enoyl-CoA hydratase (Axylo_0405) given the importance of homologous proteins in fatty acid signal biosynthesis and biofilm development among diverse bacterial species.23,24,25,26,27,28,29 We named this gene echA (for enoyl-CoA hydratase A) and sought to characterize its effects on A. xylosoxidans biofilm physiology in greater detail.
Generation and complementation of an echA mutant
Genetic tractability has been challenging for A. xylosoxidans due its inherent resistance to multiple classes of antibiotics and inducible efflux system as a second line of defense.12,13,15 We therefore sought to develop a robust genetic system for the generation and complementation of marker-free deletion mutants that would facilitate further study of the genetic basis of biofilm formation. Given that tetracycline resistance was an effective marker to generate the transposon mutant library, the tetracycline resistance cassette from pEX18tc30 was PCR amplified and ligated into the mobilizable suicide vector pSMV831 generating pBMB1 (empty vector) and pBMB2 (echA deletion construct; Supplementary Fig. 1). Attempts to construct a complementation vector using broad host-range cloning plasmids were unsuccessful. We therefore introduced echA into pBMB3 (pBBR1MCS-5::alcA) forming pBMB4 (Supplementary Fig. 1), placing echA expression under the control of an alcohol-inducible promoter.32 Using these vectors, we generated a markerless deletion mutant and complement of A. xylosoxidans MN001 lacking echA.
A. xylosoxidans biofilm ultrastructure is mediated by echA
To confirm that the biofilm-deficient phenotypes of transposon mutants 21-A5, 21-F3, and 86-E10 (Table 1) were a result of mutations in echA, we re-assessed biofilm formation by the markerless ΔechA mutant using the CV assay described above. As before, ΔechA exhibited a significant decrease in biofilm biomass accumulation relative to the wildtype (p = 0.002) after 72 h (Fig. 2). Complementation with pBMB4 restored the wildtype phenotype (p = 0.023), confirming a role of echA and its gene product in A. xylosoxidans biofilm development.
A putative enoyl-CoA hydratase contributes to A. xylosoxidans biofilm formation via biosynthesis of a fatty acid signaling metabolite. A. xylosoxidans biofilms were grown for 72 h, quantified using crystal violet and normalized to cell density (biofilm index). Deletion of echA resulted in a significant decrease in biofilm biomass that was restored via complementation and addition of cis-DA. Error bars represent standard error of the mean (n = 6 for WT and ΔechA; n = 3 for ΔechA + pBMB4 and ΔechA + cis-DA)
Enoyl-CoA hydratases are central to the biosynthesis of a class of fatty acid signaling molecules, or diffusible signal factors (DSFs), that have been described in diverse bacterial species for their role in mediating virulence, motility and biofilm development.24,25,26,27,28,29,33,34 In P. aeruginosa, for example, the DSF cis-2-decenoic acid (cis-DA) is known to play a critical role in biofilm dispersion.24,35 Therefore, to test whether the observed biofilm impairment phenotype in A. xylosoxidans was also mediated by a DSF-like signaling mechanism, we exogenously added synthetic cis-DA (310 nM)35 to the ΔechA mutant during biofilm development. Despite having no effect on the WT strain, addition of cis-DA to ΔechA resulted in a significant restoration of biofilm biomass relative to the untreated control (p = 0.024) (Fig. 2). These data suggest that biofilm formation in MN001 is directly mediated by a DSF-like metabolite generated by an enoyl-CoA hydratase.
Since the CV staining approach used in the initial mutant screen relies on a dye that stains not only cells, but all biomass adhering to the microtiter plate, we elected to use additional biofilm assays to further characterize the biofilm phenotype of ΔechA, and whether disruption of the putative enoyl-CoA hydratase negatively impacts a specific stage of biofilm development (e.g. attachment, matrix production, maturation). We first used a modified adhesion assay36 to test for defects in attachment to the surface of a chamber slide. Under static conditions, ΔechA exhibited no difference in surface attachment relative to the wildtype, demonstrating that initial stages of biofilm formation are not affected (Fig. 3a). We then used a common colony morphology assay that relies on Congo red staining as a macroscopic means of identifying the capacity for extracellular matrix production.37,38 Over the course of 6 days of growth, biofilm colonies showed no apparent differences in morphology or color between strains, suggesting that the echA gene product has negligible effect on matrix production in A. xylosoxidans. Finally, we used scanning electron microscopy to visualize microcolony ultrastructure in mature biofilms grown for 72 hours under static conditions (Fig. 3c). Relative to WT, the ΔechA mutant exhibited notable phenotypic differences in biofilm architecture, corroborating observations made using the microtiter plate assay. First, the mutant strain demonstrated less robust biofilm growth and reduced surface coverage relative to WT. In addition, higher magnification images revealed a less-dense packing order to mutant biofilm cells, suggesting that cell-cell signaling mediated by enoyl-CoA hydratase-derived metabolite is central to biofilm ultrastructural development in A. xylosoxidans.
echA plays a central role in biofilm ultrastructure in A. xylosoxidans MN001. a Early attachment assay for WT and echA mutant. Error bars represent standard deviation of the mean for replicate experiments (n = 3). b Colony biofilms grown on Congo red plates for 6 days revealed no differences in matrix production. c Mature biofilms of the WT and mutant were visualized by SEM to examine biofilm architecture (scale bars, top = 30μm, bottom = 10 μm). All images shown are representative of experiments performed in biological triplicate (n = 3) with similar results
ΔechA exhibits increased susceptibility to antibiotic treatment
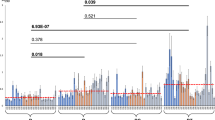
Biofilm-associated bacteria can be orders of magnitude more tolerant to antibacterial compounds than their planktonic counterparts.20 Given its defect in biofilm formation and more diffuse nature of mature microcolonies shown by SEM, we hypothesized that the ΔechA mutant would exhibit increased susceptibility to antimicrobial treatment. To test this, mature biofilms were grown statically in 8-chamber coverslip slides for 72 h and treated with various concentrations of two commonly used therapeutics to which A. xylosoxidans is tolerant, levofloxacin and tobramycin (Fig. 4). Despite not showing any difference in minimum inhibitory concentrations for planktonic cells of the WT and mutant strains (100 μg/mL for tobramycin; 4 μg/mL for levofloxacin), Live/Dead staining of treated biofilms, visualization by microscopy (Fig. 4a), and quantification of dead biomass (Fig. 4b) revealed a statistically significant increase (p < 0.001) in susceptibility of the ΔechA biofilm to both antibiotics relative to WT. These data demonstrate a central role of echA in biofilm antibiotic tolerance.
Disruption of enoyl-CoA hydratase activity leads to increased antibiotic susceptibility. a Mature A. xylosoxidans biofilms were visualized by fluorescence microscopy after 6 h exposure to levofloxacin (100 μg/mL) and tobramycin (1000 μg/mL). Deletion of echA resulted in increased susceptibility to both compounds. b Integrative densities of green (live) and red (dead) cells were used to calculate % dead biomass for each biofilm treated with various concentrations of antibiotic (bars represent standard deviation, n = 4 for each treatment)
Discussion
A. xylosoxidans is recognized as an emerging nosocomial pathogen and is associated with a range of infections, including bacteremia,39 endocarditis,40 meningitis,41 and pneumonia in immunocompromised individuals.42 In addition, the prevalence of A. xylosoxidans is now estimated to be as high as 20% among individuals with CF,6,7,8,9,10,11 which is of increasing concern given its reported correlation to lung function decline,3 patient-to-patient transmissibility,5 and multi-drug resistance phenotypes.12,13,14,15 Unfortunately, little is known about the physiology and molecular biology of this pathogen, and a greater understanding is critically needed to inform new treatment strategies. This study is an important step in that direction as it identifies several molecular determinants of biofilm growth, thought to play a critical role in the persistence and pathogenesis of A. xylosoxidans in the CF airways.16
The inherent and acquired drug resistance of Achromobacter spp. not only limits therapeutic approaches but has also led to a paucity of tools (i.e. selection markers) available for molecular biology studies of A. xylosoxidans and manipulation of its genome. Here, we systematically screened numerous vectors and determined that among antibiotics tested, only tetracycline and gentamicin resistance markers were compatible with both E. coli and A. xylosoxidans. TetR and GentR cassettes were then used to generate (to our knowledge) the first transposon mutant library and a null deletion strain in A. xylosoxidans, facilitating a detailed study at the molecular level. These tools pave the way for addressing critical questions about the physiology of this bacterium and its role in pathogenesis.
Screening of our transposon library revealed several genetic determinants of biofilm formation. Statistically, genome coverage in our library was unsaturated (~92%), though 31 hits in genes in diverse functional categories suggests that the regulation of biofilm development in A. xylosoxidans integrates a complex network of cellular processes and environmental stimuli. Several homologs of genes identified in this screen have been linked to biofilm formation in other bacteria. For example, flgB, encoding a flagellar basal body rod protein, has been implicated in biofilm development in both Bordetella bronchiseptica43 and P. aeruginosa.44 It is noteworthy that other flagellar-associated genes are downregulated in A. xylosoxidans biofilms relative to planktonically grown cells.45 In addition, LysR family regulators, such as Axylo_0951 that was identified in our screen, have been implicated in biofilm morphology and mucosal colonization in other respiratory pathogens such as P. aeruginosa, Burkholderia cenocepacia, and Klebsiella pneumoniae.46,47,48 Further characterization of these and other genes identified in our screen (see Table 1) will undoubtedly generate new insights into the many aspects of Achromobacter biofilm physiology that remain uncharacterized.
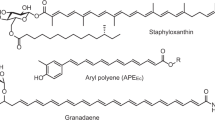
We took most interest in Axylo_0405 (echA), encoding a putative enoyl-CoA hydratase (one of eight in strain MN001) with homology to DspI in P. aeruginosa.24 DspI and other bacterial homologs (e.g. RpfF in X. campestris)27 are key enzymes used in the synthesis of diffusible signaling factors (DSFs) that are monounsaturated fatty acids of medium chain length containing a cis-2 double bond thought to be central in their mechanism of action. These metabolites broadly regulate bacterial behaviors such as motility, iron uptake and virulence,29,49,50 and data presented here adds to the growing appreciation of their widespread role in biofilm development across diverse Gram-negative bacteria. While synthetic cis-DA was able to partially rescue the biofilm defect in ΔechA, the specific identity of the fatty acid signal produced by A. xylosoxidans remains to be determined. It is also possible that A. xylosoxidans may respond to multiple DSF-like signals produced endogenously or exogenously, as interspecies signaling mediated by cis-2 fatty acids has also been reported.28 Ongoing work is now aimed at characterizing the signal structure, its biosynthetic pathway, sensing mechanism(s) and downstream phenotypic effects in addition to biofilm development.
Respiratory pathogens that adopt a biofilm lifestyle in vivo exist in a protective environment against antimicrobials and host defense mechanisms. Furthermore, biofilm cells generally reduce their metabolic activity relative to planktonic cells, further enhancing their intrinsic resistance to therapy. A. xylosoxidans has been shown to form robust biofilms both in vivo and in vitro,16,18 which is corroborated by microscopy data presented here. However, our data demonstrating a heightened susceptibility of ΔechA to antibiotic treatment suggest that interfering with fatty acid-mediated cell-cell signaling may represent a viable approach to managing A. xylosoxidans biofilms in the lower airways, particularly when used in combination with conventional CF antibiotics. Here we elected to test two compounds to which A.xylosoxidans has high resistance, levofloxacin and tobramycin,51 though it will be interesting to test whether this effect holds true for other antibiotics with different mechanisms of action.
In summary, we developed a robust genetic system for use in A. xylosoxidans that we leveraged to generate a transposon mutant library. Further study of this library revealed a suite of genes essential for biofilm development in vitro and invoked an essential role for a putative enoyl-CoA hydratase in biofilm ultrastructure and tolerance to antimicrobials, likely mediated by a cis-2 fatty acid signaling compound. While a clear picture of the clinical impact of A. xylosoxidans in CF airway disease is only beginning to emerge, the continued study of the molecular basis of its biofilm formation and physiology will undoubtedly lead to improved treatment strategies for this important respiratory pathogen.
Methods
Bacterial strains, plasmids, and growth conditions
Bacterial strains used are listed in Supplementary Table 1. A. xylosoxidans MN00152 and Escherichia coli were grown in lysogeny broth (LB) at 37 °C unless otherwise specified. When necessary, growth media were supplemented with gentamicin at 20 μg/ml (E. coli) or 100 μg/ml (A. xlyosoxidans), ampicillin at 100 μg/ml (E. coli) or 300 μg/ml (A. xylosoxidans), carbenicillin (300 μg/ml), tetracycline (300 μg/ml), or chloramphenicol (30 μg/ml). E. coli strain β2155 was supplemented with 360 μM diaminopimelic acid (DAP).
Transposon mutagenesis
The transposon delivery vector pTnTet containing the hyperactive mariner transposon21 was introduced by transformation into the E. coli donor bacterial strain β2155.53 A. xylosoxidans MN001 and E. coli β2155 (carrying pTnTet) were grown overnight in LB and LB containing chloramphenicol (30 mg/ml) and 360 μM DAP, respectively, at 37 °C. Cells were combined in a donor-to-recipient ratio of 5:1, centrifuged at 4000 × g for 5 min, resuspended in 200 μL fresh LB-DAP and spot-plated (10 μL) onto LB agar. Mating proceeded for 8 h at 37 °C, at which point cells were harvested and resuspended in 1 mL of LB. Cell suspensions were diluted 1:5, and 100 μL aliquots were plated on LB-tetracycline agar and allowed to grow for 48 h at 37 °C. Colonies were randomly selected for downstream biofilm assays.
Biofilm microtiter plate assay
To identify determinants of biofilm development, transposon mutants were screened using a modified crystal violet (CV) assay approach.22 Briefly, individual mutants were transferred to single wells of a 96-well microtiter plate containing 200 μL LB per well, and incubated while shaking at 37 °C. Following 24 h of growth, 2 μL was transferred to 198 μL ABT medium [15 mM (NH4)2SO4, 40 mM Na2HPO4, 20 mM KH2PO4, 50 mM NaCl, 1 mM MgCl2, 0.1 mM CaCl2 and 0.01 mM FeCl3 supplemented with 0.5% casamino acids and 0.5% glucose]25 in a new microtiter plate, and grown for an additional 24 h at 37 °C in a humidified chamber. Plates were first measured spectrophotometrically (OD600) to determine culture cell density. Supernatants were discarded, and plates were washed 3X with ultrapure water. Plates were dried in a biosafety hood for 2.5 h and stained with 200 μL of 0.1% CV for 20 minutes. Plates were then washed 5X to remove excess stain, air-dried for 4 h, and 200 μL 30% acetic acid was added to each well. Following a 15 min incubation, CV absorbance was measured spectrophotometrically (OD560) and normalized to culture density. Wells exhibiting less than 50% absorbance than the wildtype (MN001) were considered putative hits (134 total) and were subjected to a secondary screen using the same protocol (n = 4 for each mutant). Transposon mutants showing a significant reduction in biofilm growth (31 total, as determined by a Mann-Whitney U test) were stored for further characterization.
Biofilm growth of MN001, its ΔechA derivative and complemented strain (see below) were also tested using the same microtiter assay. In these experiments, growth medium was supplemented with 2% ethanol to drive expression of the alcA promoter in pBMB4 (below). When indicated, cis-2-decenoic acid (F13807D, Carbosynth) was also added at a concentration of 310 nM.35
Arbitrary PCR and mutant sequencing
An arbitrary-PCR-based approach22 was used to identify sequences flanking transposon insertion sites. The PCR method involved two rounds of reactions, with the first using a primer unique for the mariner transposon and one degenerate primer (pair 1, Table S2).54 The second round included nested primers (pair 2) unique to the transposon and 5’ end of the arbitrary primer for amplification of PCR products obtained in the first round. PCR products were sequenced at the University of Minnesota Genomics Center (UMGC) and were mapped to the A. xylosoxidans MN001 genome (Accession#PRJNA288995).
Construction and complementation of an echA deletion mutant
To generate a deletion vector compatible with A. xylosoxidans, pSMV855 was first digested using ApaI. A tetracycline resistance cassette was then amplified from pEX18tc31 using primer pair 3 (Supplementary Table 2) and digested with ApaI. Vector and insert (1:3 ratio) were then ligated using T4 ligase, transformed into E. coli UQ950 and selected for on LB agar containing tetracycline (15 μg/mL). Colonies were screened using primers M13F and TetR (pair 4) to confirm insertion orientation. One plasmid, pBMB1, was selected for further use.
To generate an in-frame, unmarked deletion of Axylo1_0405 (echA), ~1 kb sequences flanking echA were PCR amplified using primer pairs 5 and 6 (Supplementary Table 2). These flanking regions were combined and cloned into pBMB1 digested with SpeI and XhoI using Gibson assembly, resulting in pBMB2 (Supplementary Fig. 1). This plasmid was then chemically transformed into UQ950, and positive ligations were screened by PCR. pBMB2 was then transformed into E. coli strain WM3064 and mobilized into A. xylosoxidans MN001 by conjugation. Recombinants were selected for on LB-tetracycline agar and double recombinants were selected for on LB agar containing 6% sucrose.
Complementation was achieved via exogenous expression of echA (Ax_0405) from pBBR1MCS-5.55 To do so, an alcohol-inducible promoter, alcA32 was first amplified from pGGA008 using primers alcA_F and alcA_R (Supplementary Table 2) before digestion with restriction enzymes HindIII and BamHI. Ligation into similarly digested pBBR1MCS-5 yielded pBMB3 (pBBR1MCS-5::alcA). echA was then amplified from A. xylosoxidans MN001 genomic DNA using primers echA_F and echA_R, and digested with BamHI and SacI before ligation into pBMB3 using T4 ligase. The resulting vector, pBMB4 (pBBR1MCS-5::alcAechA; Supplementary Fig. 1), was transformed into E. coli UQ950. This vector was then introduced into A. xylosoxidans MN001 via conjugation with an E. coli donor strain WM3064, and transconjugants were selected on LB agar containing 300 μg/mL gentamicin sulfate. All constructs and positive transformants were verified by Sanger sequencing.
Attachment assay
A modified attachment assay36 was used to assess early attachment of A. xylosoxidans to a polystyrene substratum. Briefly, MN001 and its ΔechA derivative were grown for 18 h at 37 °C in ABT followed by dilution 1:100 into fresh medium. Cells were then grown to mid-log phase (OD600 = 0.6) before dilution in ABT to an OD600 of 0.1. 200 μl of each culture was added to an 8-chamber coverslip slide (Ibidi, #80824) and incubated at 37 °C for 1 h. Following incubation, slides were rinsed twice with 200 μl of PBS to remove unattached biomass, and attached cells were stained using SYTO 9 (Invitrogen) in PBS according the manufacturer’s protocol. Substrata were imaged using an Olympus IX83 inverted fluorescence microscope with a transmitted Koehler illuminator and a 40X objective lens (Olympus). Four images per strain per biological replicate (n = 4) were captured on a Hamamatsu ORCA camera, and post-acquisition analysis was performed using FIJI software56 by calculating the integrated density of SYTO 9.
Colony biofilm assay
MN001 and ΔechA were grown overnight in LB medium, diluted 1:1000, and 10 μL was spotted on nutrient agar containing 1% tryptone, 1% agar, 20 μg/mL Coomassie Brilliant Blue, and 40 μg/mL Congo red.36 Plates were incubated at 37 °C for 6 days and monitored daily for colony morphology.
Scanning electron microscopy
Overnight cultures were diluted 1:10 in fresh LB medium and were added to 48-well microtiter plates containing autoclaved Aclar fluoropolymer film (Electron Microscopy Sciences, Hatfield, PA). Biofilms were grown for 48 h at 37 °C, shaking at 50 rpm, and prepared for SEM using cationic dye stabilization methods.57,58 Briefly, Aclar membranes containing biofilm growth were washed three times in 0.2 M sodium cacodylate buffer, and submerged in primary fixative (0.15 M sodium cacodylate buffer, pH 7.4, 2% paraformaldehyde, 2% glutaraldehyde, 4% sucrose, 0.15% alcian blue 8 GX) for 22 h. Samples were washed three more times prior to a 90 minute treatment with secondary fixative (1% osmium tetroxide, 1.5% potassium ferrocyanide, 0.135M sodium cacodylate, pH 7.4). After three final washes, biofilms were chemically dehydrated in a graded ethanol series (25, 50, 70, 85, 95 [2×] and 100% [2×]) before CO2-based critical point drying. Aclar membranes were attached to SEM specimen mounts using carbon conductive adhesive tape and sputter coated with ~ 5 nm iridium using the Leica ACE 600 magnetron-based system. Biofilms were imaged using a Hitachi S-4700 field emission SEM with an operating voltage of 2 kV.
Antibiotic challenge
Biofilm antimicrobial susceptibility testing was performed using a chamber slide assay.59 Briefly, MN001 and ΔechA were grown in LB overnight, diluted 1:1000 and grown to an OD600 of 0.6 before dilution to an OD600 of 0.5. In total 200 μL of each culture was then added to each well of an Ibidi 8-chamber coverslip slide and incubated at 37 °C in a humidified chamber. After 24 h, medium was replaced with fresh LB and incubated for an additional 24 h. Media was gently aspirated from each well, replaced with LB containing either tobramycin or levofloxacin (0, 10, 100, and 1000 μg/mL), and incubated at 37 °C for 6 h. Cells were washed in sterile PBS to remove unattached biomass, stained for 15 minutes using the BacLight Live/Dead viability assay (Life Technologies, #L7012) and visualized by fluorescent imaging as described above. Integrated density for SYTO 9 and propidium iodide (PI) for each image was determined using FIJI,56 and percentage of dead biomass was determined by (average integrative density of PI)/(average integrated density of PI+ integrated density of SYTO 9).59 Data were generated using four biological replicates (n = 4).
Prior publication
This work was previously published as a preprint.60
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data generated during and/or analyzed during the current study are included in this article, its Supplementary information files, or are available from the corresponding author on reasonable request.
References
Gibson, R. L., Burns, J. L. & Ramsey, B. W. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am. J. Respir. Crit. Care. Med. 168, 918–951 (2003).
Salsgiver, E. L. et al. Changing epidemiology of the respiratory bacteriology of patients with cystic fibrosis. Chest 149, 390–400 (2016).
Ridderberg, W., Bendstrup, K. E., Olesen, H. V., Jensen-Fangel, S. & Nørskov-Lauritsen, N. Marked increase in incidence of Achromobacter xylosoxidans infections caused by sporadic acquisition from the environment. J. Cyst. Fibros. 10, 466–469 (2011).
Rønne Hansen, C., Pressler, T., Høiby, N. & Gormsen, M. Chronic infection with Achromobacter xylosoxidans in cystic fibrosis patients; a retrospective case control study. J. Cyst. Fibros. 5, 245–251 (2006).
Van Daele, S. et al. Shared genotypes of Achromobacter xylosoxidans strains isolated from patients at a cystic fibrosis rehabilitation center. J. Clin. Microbiol. 43, 2998–3002 (2005).
Burns, J. L. et al. Microbiology of sputum from patients at cystic fibrosis centers in the United States. Clin. Infect. Dis. 27, 158–163 (1998).
Tan, K., Conway, S. P., Brownlee, K. G., Etherington, C. & Peckham, D. G. Alcaligenes infection in cystic fibrosis. Pediatr. Pulmonol. 34, 101–104 (2002).
Raso, T., Bianco, O., Grosso, B., Zucca, M. & Savoia, D. Achromobacter xylosoxidans respiratory tract infections in cystic fibrosis patients. APMIS 116, 837–841 (2008).
Pereira, R. H. et al. Patterns of virulence factor expression and antimicrobial resistance in Achromobacter xylosoxidans and Achromobacter ruhlandii isolates from patients with cystic fibrosis. Epidemiol. Infect. 145, 600–606 (2017).
De Baets, F., Schelstraete, P., Van Daele, S., Haerynck, F. & Vaneechoutte, M. Achromobacter xylosoxidans in cystic fibrosis: Prevalence and clinical relevance. J. Cyst. Fibros. 6, 75–78 (2007).
Amoureux, L. et al. Detection of Achromobacter xylosoxidans in hospital, domestic, and outdoor environmental samples and comparison with human clinical isolates. Appl. Environ. Microbiol. 79, 7142–7149 (2013).
Bador, J., Amoureux, L., Blanc, E. & Neuwirth, C. Innate aminoglycoside resistance of Achromobacter xylosoxidans is due to axyXY-oprZ, an RND-type multidrug efflux pump. Antimicrob. Agents Chemother. 57, 603–605 (2013).
Bador, J. et al. First description of an RND-type multidrug efflux pump in Achromobacter xylosoxidans, AxyABM. Antimicrob. Agents Chemother. 55, 4912–4914 (2011).
Amoureux, L. et al. Epidemiology and resistance of Achromobacter xylosoxidans from cystic fibrosis patients in Dijon, Burgundy: First French data. J. Cyst. Fibros. 12, 170–176 (2013).
Rolston, K. V. & Messer, M. The in-vitro susceptibility of Alcaligenes denitrificans subsp. xylosoxidans to 40 antimicrobial agents. J. Antimicrob. Chemother. 26, 857–860 (1990).
Nielsen, S. M., Nørskov-Lauritsen, N., Bjarnsholt, T. & Meyer, R. L. Achromobacter species isolated from cystic fibrosis patients reveal distinctly different biofilm morphotypes. Microorganisms 4, pii: E33 (2016).
Hansen, C. R. et al. Inflammation in Achromobacter xylosoxidans infected cystic fibrosis patients. J. Cyst. Fibros. 9, 51–58 (2010).
Jakobsen, T. H. et al. Complete genome sequence of the cystic fibrosis pathogen Achromobacter xylosoxidans NH44784-1996 complies with important pathogenic phenotypes. PLoS ONE 8, e68484 (2013).
Bjarnsholt, T. et al. The in vivo biofilm. Trends Microbiol. 21, 466–474 (2013).
Stewart, P. S. & Costerton, J. W. Antibiotic resistance of bacteria in biofilms. Lancet 358, 135–138 (2001).
Chiang, S. L. & Rubin, E. J. Construction of a mariner-based transposon for epitope-tagging and genomic targeting. Gene 296, 179–185 (2002).
O’Toole, G. A. et al. Genetic approaches to study of biofilms. Methods Enzym. 310, 91–109 (1999).
Wang, L. H. et al. A bacterial cell-cell communication signal with cross-kingdom structural analogues. Mol. Microbiol. 51, 903–912 (2004).
Amari, D. T., Marques, C. N. H. & Davies, D. G. The putative enoyl-coenzyme A hydratase DspI is required for production of the Pseudomonas aeruginosa biofilm dispersion autoinducer cis-2-decenoic acid. J. Bacteriol. 195, 4600–4610 (2013).
Ionescu, M. et al. Promiscuous diffusible signal factor production and responsiveness of the Xylella fastidiosa Rpf system. mBio 7, e01054–16 (2016).
Newman, K. L., Almeida, R. P. P., Purcell, A. H. & Lindow, S. E. Cell-cell signaling controls Xylella fastidiosa interactions with both insects and plants. Proc. Natl Acad. Sci. USA 101, 1737–1742 (2004).
Dow, J. M. et al. Biofilm dispersal in Xanthomonas campestris is controlled by cell-cell signaling and is required for full virulence to plants. Proc. Natl Acad. Sci. USA 100, 10995–11000 (2003).
Boon, C. et al. A novel DSF-like signal from Burkholderia cenocepecia interferes with Candida albicans morphological transition. ISME J. 2, 27–36 (2003).
Huang, T. P. & Lee Won, A. C. Extracellular fatty acids facilitate flagella-independent translocation by Stenotrophomonas maltophila. Res. Microbiol. 158, 702–711 (2007).
Kovach, M. E. et al. Four new derivatives of the broad-host-range cloning vector pBBR1MCS, carrying different antibiotic-resistance cassettes. Gene 166, 175–176 (1995).
Hoang, T. T., Karkhoff-Schweizer, R. R., Kutchma, A. J. & Schweizer, H. P. A broad-host-range Flp-FRT recombination system for site-specific excision of chromosomally-located DNA sequences: Application for isolation of unmarked Pseudomonas aeruginosa mutants. Gene 212, 77–86 (1998).
Lampropoulos, A. et al. Greengate—a novel, versatile, and efficient cloning system for plant transgenesis. PLoS ONE 8, e83043 (2013).
Deng, Y. et al. Cis-2-dodecenoic acid receptor RpfR links quorum-sensing signal perception with regulation of virulence through cyclic dimeric guanosine monophosphate turnover. Proc. Natl Acad. Sci. USA 109, 15479–15484 (2012).
Barber, C. E. et al. A novel regulatory system required for pathogenicity of Xanthomonas campestris is mediated by a small diffusible signal molecule. Mol. Microbiol. 24, 555–566 (1997).
Davies, D. G. & Marques, C. N. H. A fatty acid messenger is responsible for inducing dispersion in microbial biofilms. J. Bacteriol. 191, 1393–1403 (2009).
Ramsey, M. M. & Whiteley, M. Pseudomonas aeruginosa attachment and biofilm development in dynamic environments. Mol. Microbiol. 53, 1075–1087 (2004).
Dietrich, L. E. et al. Bacterial community morphogenesis is intimately linked to the intracellular redox state. J. Bacteriol. 195, 1371–1380 (2013).
Jones, C. J. & Wozniak, D. J. Congo red stain identifies matrix overproduction and is an indirect measurement for c-di-GMP in many species of bacteria In Sauer K. (ed) c-di-GMP signaling. Meth. Mol. Biol. Humana Press, New York, NY (2017).
Aisenberg, G., Rolston, K. V. & Safdar, A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer. Cancer 101, 2134–2140 (2004).
Ahmed, M. S. et al. Achromobacter xylosoxidans, an emerging pathogen in catheter-related infection in dialysis population causing prosthetic valve endocarditis: a case report and review of literature. Clin. Nephrol. 71, 350–354 (2009).
Namnyak, S. S., Holmes, B. & Fathalla, S. E. Neonatal meningitis caused by Achromobacter xylosoxidans. J. Clin. Microbiol. 22, 470–471 (1985).
Wood, G. C. et al. Treatment of Achromobacter ventilator-associated pneumonia in critically ill trauma patients. Ann. Pharmacother. 52, 120–125 (2018).
Nicholson, T. L., Conover, M. S. & Deora, R. Transcriptome profiling reveals stage-specific production and requirement of flagella durting biofilm development in Bordetella bronchiseptica. PLoS ONE 7, e49166 (2012).
De La Fuente-Nunez, C. et al. Inhibition of bacterial biofilm formation and swarming motility by a small synthetic cationic peptide. Antimicrob Agents Chemother 56, 2696–2704 (2012).
Nielsen, S. M., Penstoft, L. N. & Norskov-Lauritsen, N. Motility, biofilm formation and antimicrobial efflux of sessile and planktonic cells of Achromobacter xylosoxidans. Pathogens 8, 14 (2019).
Hennequin, C. & Forestier, C. oxyR, a LysR-type regulator involved in Klebsiella pneumoniae mucosal and abiotic colonization. Infect. Immun. 77, 5449–5457 (2009).
Cao, H. et al. A quorum sensing-associated virulence gene of Pseudomonas aeruginosa encodes a LysR-like transcription regulator with a unique self-regulatory mechanism. Proc. Natl Acad. Sci. USA 98, 14613–14618 (2001).
Bernier, S. P., Nguyen, D. T. & Sokol, P. A. A LysR-type transcriptional regulator in Burkholderia cenocepacia influences colony morphology and virulence. Infect. Immun. 76, 38–47 (2008).
Huedo, P. et al. Two different rpf clusters distributed among a population of Stenotrophomonas maltophila clinical strains display differential diffusible signal factor production and virulence regulation. J. Bacteriol. 196, 2431 (2014).
Chatterjee, S. & Sonti, R. V. rpfF mutants of Xanthomonas oryzae sp. oryzae are deficient for virulence and growth under low iron conditions. Mol. Plant Microbe Interact. 15, 463–471 (2002).
Abbott, I. J. & Peleg, A. Y. Stenotrophomonas, Achromobacter, and nonmelioid Burkholderia species: antimicrobial resistance and therapeutic strategies. Sem. Resp. Crit. Care Med. 36, 99–110 (2015).
Badalamenti, J. P. & Hunter, R. C. Complete genome sequence of Achromobacter xylosoxidans MN001, a cystic fibrosis airway isolate. Genome Announc 3, pii: e00947-15 (2015).
Dehio, C. & Meyer, M. Maintenance of broad-host-range incompatibility group p and group q plasmids and transposition of tn5 in bartonella henselae following conjugal plasmid transfer from Escherichia coli. J. Bacteriol. 179, 538–540 (1997).
Larsen, R. A., Wilson, M. M., Guss, A. M. & Metcalf, W. W. Genetic analysis of pigment biosynthesis in xanthobacter autotrophicus py2 using a new, highly efficient transposon mutagenesis system that is functional in a wide variety of bacteria. Arch. Microbiol. 178, 193–201 (2002).
Saltikov, C. W., Cifuentes, A., Venkateswaran, K. & Newman, D. K. The ars detoxification system is advantageous but not required for As(v) respiration by the genetically tractable Shewanella species strain ANA-3. Appl. Environ. Microbiol. 69, 2800–2809 (2003).
Schindelin, J. et al. FIJI: An open-source platform for biological-image analysis. Nat. Methods 9, 676–682 (2012).
Erlandsen, S. L., Kristich, C. J., Dunny, G. M. & Wells, C. L. High-resolution visualization of the microbial glycocalyx with low-voltage scanning electron microscopy: dependence on cationic dyes. J. Histochem. Cytochem. 52, 1427–1435 (2004).
Barnes, A. M., Ballering, K. S., Leibman, R. S., Wells, C. L. & Dunny, G. M. Enterococcus faecalis produces abundant extracellular structures containing DNA in the absence of cell lysis during early biofilm formation. mBio 3, e00193–00112 (2012).
Tom, S. K., Yau, Y. C., Beaudoin, T., LiPuma, J. J. & Waters, V. Effect of high-dose antimicrobials on biofilm growth of Achromobacter species isolated from cystic fibrosis patients. Antimicrob. Agents Chemother. 60, 650–652 (2016).
Cameron, L. C., et al. A putative enoyl-CoA hydratase contributes to biofilm formaton and the antibiotic tolerance of Achromobacter xylosoxidans. Preprint at http://www.biorxiv.org/content/10.1101/620559v1 (2019).
Acknowledgements
pGGA008 (Addgene plasmid #48817) was a gift from Dr. Jan Lohmann (Heidelberg). We thank Clayton Summitt for assistance with data analysis and other members of the Hunter lab for critical review of the manuscript. Parts of this work were carried out in the Characterization Facility, University of Minnesota, which receives partial support from NSF through the Materials Research Science and Engineering Centers (MRSEC) program. This study was supported by the University of Minnesota, a NHLBI Pathway to Independence award to RCH, American Society for Microbiology Undergraduate Research Fellowships to AKL and LAK.
Author information
Authors and Affiliations
Contributions
L.C. performed experiments, created figures, and helped write and edit the manuscript. B.B. performed experiments, created figures, and helped edit the manuscript. C.P. and A.L. performed experiments. L.K. performed SEM experiments and created figures. R.H. contributed to the conception, experimental design, data interpretation, statistical analyses, and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cameron, L.C., Bonis, B., Phan, C.Q. et al. A putative enoyl-CoA hydratase contributes to biofilm formation and the antibiotic tolerance of Achromobacter xylosoxidans. npj Biofilms Microbiomes 5, 20 (2019). https://doi.org/10.1038/s41522-019-0093-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41522-019-0093-6
This article is cited by
-
Cyclohexanecarboxylic acid degradation with simultaneous nitrate removal by Marinobacter sp. SJ18
Environmental Science and Pollution Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.