Abstract
Artemisinin partial resistance may facilitate selection of Plasmodium falciparum resistant to combination therapy partner drugs. We evaluated 99 P. falciparum isolates collected in 2021 from northern Uganda, where resistance-associated PfK13 C469Y and A675V mutations have emerged, and eastern Uganda, where these mutations are uncommon. With the ex vivo ring survival assay, isolates with the 469Y mutation (median survival 7.3% for mutant, 2.5% mixed, and 1.4% wild type) and/or mutations in Pfcoronin or falcipain-2a, had significantly greater survival; all isolates with survival >5% had mutations in at least one of these proteins. With ex vivo growth inhibition assays, susceptibility to lumefantrine (median IC50 14.6 vs. 6.9 nM, p < 0.0001) and dihydroartemisinin (2.3 vs. 1.5 nM, p = 0.003) was decreased in northern vs. eastern Uganda; 14/49 northern vs. 0/38 eastern isolates had lumefantrine IC50 > 20 nM (p = 0.0002). Targeted sequencing of 819 isolates from 2015–21 identified multiple polymorphisms associated with altered drug susceptibility, notably PfK13 469Y with decreased susceptibility to lumefantrine (p = 6 × 10−8) and PfCRT mutations with chloroquine resistance (p = 1 × 10−20). Our results raise concern regarding activity of artemether-lumefantrine, the first-line antimalarial in Uganda.
Similar content being viewed by others
Introduction
Drug resistance has challenged the treatment and control of falciparum malaria for decades1. Partial resistance to artemisinins, the most important drugs now used to treat malaria, was identified in southeast Asia about 15 years ago2,3. The partial resistance phenotype entails delayed clearance of parasites after treatment of patients with artemisinins4, or enhanced survival of cultured parasites after exposure to dihydroartemisinin (DHA)5. Partial resistance in southeast Asia has been shown to be associated with any of about 20 candidate or validated mutations in the propeller domain of the P. falciparum kelch 13 (PfK13) protein6,7. Additional polymorphisms have accompanied PfK13 mutations in artemisinin resistant southeast Asian parasites,8,9 and in vitro selection of African parasites with DHA led to delayed clearance associated with mutations in P. falciparum coronin (Pfcoronin)10. PfK13 mutations validated as resistance mediators in southeast Asia have been reported in some other parts of the world11,12,13, but until recently evidence of sustained prevalence of these mutations or documented clinical or in vitro resistance has been lacking14. Of greatest concern has been potential emergence or spread of resistance to Africa, where the bulk of malaria morbidity and mortality is seen15. Recently, PfK13 mutations previously linked to artemisinin partial resistance in Asia have been described in East Africa, with emergence of the PfK13 R561H mutation in Rwanda16,17,18 and the C469Y and A675V mutations in northern Uganda19,20,21,22. In limited studies the C469Y, R561H, and A675V mutations have been shown to associate with artemisinin partial resistance measured clinically (delayed clearance) or in vitro (enhanced survival)17,22, but our understanding of the impacts of the recently emerged P. falciparum mutations on drug sensitivity and the treatment efficacies of leading artemisinin-based combination therapies (ACTs) in Africa is incomplete.
ACTs combine a rapid acting artemisinin plus a slower acting partner drug23. In southeast Asia, the emergence of artemisinin partial resistance was followed by evidence for decreased antimalarial activity of the ACT partner drugs mefloquine24 and piperaquine25. Notably, resistance to artemisinins, associated primarily with the PfK13 580Y mutation, and piperaquine, associated with novel mutations in PfCRT and plasmepsin 2/3 gene amplification, led to failure rates for DHA-piperaquine >50% in Cambodia26,27,28. The recent emergence of partial resistance to artemisinins in East Africa may similarly lead to selection of parasites with decreased sensitivity to ACT partner drugs. Considering the massive toll of malaria in Africa, this consequence could be devastating, as was seen with the emergence of chloroquine resistance in the 1980s, leading to millions of excess malaria deaths29.
The most commonly used ACT to treat malaria in Africa is artemether-lumefantrine. Unlike most antimalarials, lumefantrine is not available as a monotherapy, but rather is supplied only in combination with artemether. Perhaps for this reason, P. falciparum resistance to lumefantrine has not been definitively identified in parasites isolated in the field. However, an unstable lumefantrine resistance phenotype was selected by long-term incubation with the drug in vitro30, and variations in susceptibility to lumefantrine have been seen in studies of field isolates. Lumefantrine susceptibility has been associated with polymorphisms in PfMDR1, a putative drug transporter. The PfMDR1 86Y mutation was selected by use of amodiaquine, selected against by therapy with artemether-lumefantrine, and has decreased to very low prevalence in most of Africa15, including Uganda20, in recent years. The wild type PfMDR1 N86 genotype is associated with lower ex vivo lumefantrine susceptibility compared to that in 86Y mutant parasites31,32, and was associated with treatment failure in an analysis of data from 31 clinical trials33, but changes in susceptibility associated with this allele were modest. Lumefantrine sensitivity is also decreased with pfmdr1 gene amplification34,35, but this polymorphism has been very uncommon in studied African parasites15. In Uganda, lumefantrine susceptibility decreased modestly in conjunction with loss of the PfMDR1 86Y mutation over time31,32,36,37, the relative clinical efficacy of artemether-lumefantrine compared to that of artesunate-amodiaquine decreased over time38, and a recent trial showed corrected treatment efficacy of artemether-lumefantrine below 90% at one site39. Overall, although in vitro activity of lumefantrine and clinical efficacy of artemether-lumefantrine have generally remained good, there is evidence that activity may be decreasing.
The recent emergence of artemisinin resistant P. falciparum in northern Uganda raises concern that resistance to ACT partner drugs may follow, as seen in southeast Asia. To explore this possibility and better characterize artemisinin partial resistance in Uganda, we compared genotypes and phenotypes of parasites collected in northern Uganda, where the PfK13 469Y and 675V mutations have emerged in recent years, and eastern Uganda, where we have studied clinical isolates for over a decade, and markers of artemisinin resistance have been uncommon. In addition, we analyzed a larger bank of phenotyped isolates from eastern Uganda to better explore genetic correlates of drug susceptibility phenotypes.
Results
Collection of P. falciparum isolates from northern and eastern Uganda
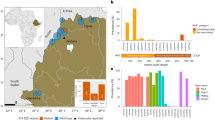
To compare isolates from different parts of the country, we assessed genotypes, growth inhibition, and ring survival for isolates collected from patients presenting with uncomplicated falciparum malaria at Patongo Health Center III, Agogo District, in northern Uganda (n = 57), and Tororo District Hospital, Tororo District and Busiu Health Center IV, Mbale District, two nearby sites in eastern Uganda (n = 42), from May 31 to August 16, 2021 (Fig. 1). Features of the participants providing these samples and characteristics of their infections are described in Table 1. In a broader survey, we assessed genotypes and growth inhibition for isolates from 819 patients presenting with uncomplicated falciparum malaria, including the sites noted above and Masafu Hospital, Busia District, from December 9, 2015 to August 20, 2021 (Table 1). Drug susceptibilities for the samples from eastern Uganda through 2019 were published previously32; in this report we focus on associations between in-depth sequencing of potential resistance mediators and drug susceptibility phenotypes.
Study sites are labeled. The combined prevalence of the PfK13 469Y and 675V mutations in districts with available surveillance data from 201921 is shown with the color scale. Source data are provided as a Source Data file.
Genotypes of P. falciparum isolates from northern and eastern Uganda
For isolates collected concurrently in northern and eastern Uganda in 2021, we used molecular inversion probe (MIP) assays to characterize sequences of 80 genes potentially mediating drug resistance (Supplementary Table 1). Of particular interest were parasite polymorphisms recently associated with altered sensitivity to components of ACTs, namely PfK13 propeller domain mutations associated with partial resistance to artemisinins, and polymorphisms associated with altered sensitivity to lumefantrine (pfmdr1 amplification and mutations) and piperaquine (plasmepsin 2/3 amplification and novel PfCRT mutations). Consistent with recent data, prevalences of the PfK13 C469Y and A675V mutations were greater in northern, compared to eastern Uganda (C469Y 34% vs. 3%, p < 0.001; A675V 13% vs. 3%, p = 0.06, Table 2). Other PfK13 propeller domain mutations were uncommon; 15 mutations upstream of the propeller domain were identified. Neither amplification of the pfmdr1 or plasmepsin 2/3 genes nor PfCRT mutations associated with piperaquine resistance in Asia (T93S, H97Y, F145I, I218F, M343L, G353V)40,41 were seen. Considering other well-described polymorphisms previously associated with drug resistance, the prevalences of mutations in the transporters PfCRT (K76T) and PfMDR1 (N86Y, D1246Y) associated with altered sensitivity to aminoquinolines were very low, the prevalences of five mutations in PfDHFR (N51I, C59R, S108N) and PfDHPS (A437G, K540E) associated with resistance to the antifolates pyrimethamine and sulfadoxine were very high, and additional mutations in PfDHFR (I164L) and PfDHPS (A581G) associated with high level antifolate resistance were seen at low prevalences, all consistent with recent data from Uganda (Table 2)20,21.
Susceptibilities to lumefantrine (A growth inhibition assay) and DHA (B RSA) in parasites from northern and eastern Uganda. Each point represents the result for a single isolate (A n = 49 for northern and 38 for eastern Uganda; B n = 52 for northern and 29 for eastern Uganda). P-values were determined using the two-sided Mann–Whitney Wilcoxon test. Center bounds of boxes correspond to the median, and minimal and maximal bounds correspond to 25th and 75th percentiles, respectively. Whiskers extend to extreme values no further than 1.5x the IQR from the 25th or 75th percentiles. Source data are provided as a Source Data file.
Ex vivo drug susceptibilities of P. falciparum isolates from northern and eastern Uganda
For the isolates from 2021 studied with the ring survival assay (RSA), samples were stored at 4 °C and transported on the day of collection to our laboratory in Tororo. Time in storage before initiation of culture was slightly longer for samples collected in northern vs eastern Uganda (median 25.0 h in northern vs 24.0 h in eastern Uganda, p = 0.001). Susceptibilities to a panel of seven antimalarials were studied with a standard growth inhibition (IC50) assay and, for DHA, with the ex vivo RSA. Assays for parasites collected in the two regions of the country were run in parallel. Susceptibilities for chloroquine, desethylamodiaquine (the active metabolite of amodiaquine), piperaquine, mefloquine, and pyronaridine were similar between the two sites and, for each of these drugs, IC50s were at levels generally considered highly susceptible (Table 3). In contrast, for lumefantrine and DHA, isolates from northern Uganda were significantly less susceptible (after Bonferroni correction) than those from eastern Uganda (lumefantrine IC50 14.6 vs. 6.9 nM, p < 0.0001; dihydroartemisinin IC50 2.3 vs. 1.5 nM, p = 0.003; Table 3). For lumefantrine, 14 of 49 isolates from northern, but none of 38 from eastern Uganda had IC50 >20 nM (p = 0.0002; Fig. 2). RSAs, which entailed counting parasites 72 h after initiation of a 6 h DHA pulse, did not show significant differences in survival between isolates from northern (median 2.5% survival for 52 samples) and eastern (median 1.4% survival for 29 samples; p = 0.53) Uganda, but of note some parasites with PfK13 mutations associated with delayed parasite clearance were present at both sites (Fig. 2).
Associations between ring survival and P. falciparum genotypes
In the 81 samples from 2021 with available RSA data, we searched for associations between ring survival and PfK13 genotypes. Isolates with the PfK13 469Y mutation had significantly greater survival, with the survival highest for pure mutant (median 7.3%) compared to mixed (2.5%) and pure wild type (1.4%) parasites (Fig. 3). The PfK13 675 V mutation was not associated with increased survival, but this analysis was limited by sample size, with only 2 pure mutant 675 V isolates available for study. For broader consideration of potential resistance determinants, we used Mann–Whitney Wilcoxon tests to search for associations between polymorphisms in 23 genes for which variants have been associated with artemisinin partial resistance and our RSA results (Supplementary Table 1). Uncommon polymorphisms were assessed as aggregate variables, as described in Methods. Polymorphisms in five genes were associated with decreased or increased ring survival compared to wild type (Supplementary Table 2). Of these genes, considering the more prevalent allele (major allele) as wild type and the minor allele as mutant, any of 8 mutations in Pfcoronin (survival 6.5% in mutant vs. 2.3% in wild type, p = 0.04) or any of 17 mutations in falcipain 2a (survival 3.2% in mutant vs. 0.6% in wild type, p = 0.02) were most strongly associated with increased ring survival either alone or in association with PfK13 mutations (Fig. 4). Considering combined impacts, the presence of PfK13 469Y plus any mutation in Pfcoronin (median survival 12.6% in double mutant vs. 1.4% in double wild type, p = 0.009) or falcipain-2a (median survival 3.9% in double mutant vs. 0% in double wild type, p = 0.004) was also associated with increased survival. Of note, although some isolates with wild type PfK13 sequence had high levels of ring survival, these outliers appeared to be explained by mutations in falcipain-2a; all isolates with ring survival >5% had either the PfK13 469Y mutation, mutations in falcipain-2a, or both. Interestingly, mutations in PfK13 outside the propeller domain were associated with decreased RSA survival (the opposite of the effect of PfK13 469Y); considering any of 15 non-propeller mutations identified, survival was 1.5% in 42 mutant vs. 5.5% in 26 fully wild type isolates (p = 0.02; Supplementary Table 2). Two other polymorphisms with significant independent associations were deletion in a putative ubiquitin carboxyl-terminal hydrolase 1, associated with increased RSA survival, and a SNP in a gene encoding a protein of unknown function, associated with decreased survival.
Each point represents the result for a single isolate (A n = 50 WT, 18 C469Y, 6 A675V; B n = 50 WT, 8 C469Y, 10 469Y, 4 A675V, 2 675V). Results are shown with mixed and pure mutant isolates combined (A) or shown separately (B). P-values were determined using the two-sided Mann–Whitney Wilcoxon test. Center bounds of boxes correspond to the median, and minimal and maximal bounds correspond to 25th and 75th percentiles, respectively. Whiskers extend to extreme values no further than 1.5x the IQR from the 25th or 75th percentiles. WT, wild type. Source data are provided as a Source Data file.
Susceptibilities to DHA by RSA in parasites with different PfK13, Pfcoronin (CRN; A, B), and falcipain-2a (FP2a; C, D) genotypes are shown. Each point represents the result for a single isolate (A n = 38 WT, 18 Mut; B n = 26 C469 + CRN-WT, 9 C469 + CRN-Mut, 12 469Y + CRN-WT, 5 469Y + CRN-Mut; C n = 17 WT, 47 Mut; D n = 11 C469 + FP2a-WT, 30 C469 + FP2a-Mut, 3 469Y + FP2a -WT, 15 469Y + FP2a-Mut). PfK13 genotypes at codon 469 are indicated; mutant 469Y includes mixed isolates. P-values were determined using the two-sided Mann–Whitney Wilcoxon test. Center bounds of boxes correspond to the median, and minimal and maximal bounds correspond to the 25th and 75th percentiles, respectively. Whiskers extend to extreme values no further than 1.5x the IQR from the 25th or 75th percentiles. WT, wild type, Mut, any Pfcoronin or falcipain 2a polymorphism. Source data are provided as a Source Data file.
Associations between growth inhibition and P. falciparum genotypes
Comparing results for samples collected from northern and eastern Uganda in 2021, isolates with the PfK13 469Y or 675 V mutation were significantly less susceptible to lumefantrine (IC50 14.1 nM for mixed or mutant 469Y, 14.7 nM for mixed or mutant 675 V, and 8.7 nM for wild type; Fig. 5). Susceptibilities to the other tested drugs, including mefloquine, which appears to share some determinants of decreased activity with lumefantrine15, did not differ between wild type and PfK13 mutant parasites.
Each point represents the result for a single isolate (A n = 61 WT, 17 C469Y, 6 A675V; B n = 61 WT, 7 C469Y, 10 469Y, 5 A675V, 1 675V). Results are shown with mixed and pure mutant isolates combined (A) or shown separately (B). P-values were determined using the two sided Mann–Whitney Wilcoxon test. Center bounds of boxes correspond to the median, and minimal and maximal bounds correspond to the 25th and 75th percentiles, respectively. Whiskers extend to extreme values no further than 1.5x the IQR from the 25th or 75th percentiles. WT, wild type. Source data are provided as a Source Data file.
To more broadly consider associations between phenotypes and genotypes, we utilized a large set of 819 isolates with growth inhibition data, collected mostly from eastern Uganda from 2015-2021, and also including 49 samples collected in northern Uganda in 2021, as described above. Parasite DNA was genotyped using the MIP platform targeting 80 genes encoding proteins potentially associated with drug susceptibility, including proteins known or predicted to be drug transporters and proteins for which polymorphisms are known or suspected of contributing to resistance to established antimalarials and compounds under development (Supplementary Table 1). We identified a total of 4337 polymorphisms and used Mann–Whitney Wilcoxon tests to explore relationships between variation in ex vivo IC50s and the presence of these polymorphisms.
We first focused on lumefantrine, due to identification of significant differences in susceptibility in samples from northern and eastern Uganda, as described above. In evaluation of 713 isolates, we identified 33 non-synonymous polymorphisms associated with lumefantrine IC50, with significance at p ≤ 0.01. We then filtered to include only loci where median IC50s for mixed and mutant alleles trended in the same direction (both had increased or decreased drug sensitivity relative to parasites with pure wild type genotypes) and for which the pure minority allele was present in at least one sample. This resulted in identification of polymorphisms in 9 genes associated with altered susceptibility to lumefantrine (Table 4). Most notably, the PfK13 mutations that have emerged in northern Uganda were strongly associated with decreased susceptibility to lumefantrine (469Y, p = 6 × 10−8; 675 V p = 0.001). Other associations, with either increased or decreased susceptibility to lumefantrine, included SNPs in PfMDR1, including the 86Y mutation which is now very uncommon, but was previously associated with increased lumefantrine susceptibility; and polymorphisms in a putative phospholipase; the ApiAP2 transcription factor; the multidrug-resistance proteins PfMRP1 and PfMRP2; and the hemoglobinases falcipain-2a, falcipain-3, and plasmepsin I (Table 4).
Considering the other six tested drugs, applying the same filtering criteria as for lumefantrine, associations between a variety of polymorphisms and drug susceptibility were identified, mostly at relatively low levels of significance (Supplementary Tables 3–8). Most striking, there was strong association between well characterized mutations in PfCRT, including the K76T mutation known to mediate chloroquine resistance, and susceptibility to chloroquine (p = 10−7−10−20 for 6 PfCRT mutations) and the related drug monodesethylamodiaquine (p = 0.01–0.0003 for 4 PfCRT mutations). These results were expected15, and they support the overall validity of our analyses.
Stability of ex vivo lumefantrine susceptibility phenotypes
Anecdotally, some remarkable ex vivo drug susceptibility phenotypes have proven to be unstable, with IC50s for antimalarial drugs lower after culture adaptation compared to values seen immediately after sample collection, potentially explained by more successful growth of drug sensitive compared to drug resistant strains in mixed cultures. To explore the stability of observed phenotypes we culture adapted northern Uganda strains with remarkable lumefantrine IC50 results. Lumefantrine susceptibility was generally greater in culture adapted parasites compared to initial ex vivo values. For eight isolates with original ex vivo lumefantrine IC50 values >30 nM (median IC50 39.5 nM), subsequent IC50 values measured after culture for 4 or more weeks and then after freezing, thawing, growth in culture, and repeat assays, were generally lower than the initial ex vivo values (Table 5). However, after culture adaptation IC50 values for these eight northern Uganda isolates measured before (median IC50 13.2 nM) or after (median IC50 16.9 nM assessed in Uganda and 7.4 nM assessed in the USA) freeze-thaw-reculture were above values for parasites collected from eastern Uganda for direct comparison with the northern Uganda isolates (median IC50 6.9 nM for 38 isolates) or for a larger set of isolates published earlier (median IC50 5.1 nM for 365 isolates32).
Discussion
The emergence in northern Uganda of P. falciparum harboring the PfK13 C469Y or A675V mutations raises concern regarding selection of parasites resistant to both artemisinins and ACT partner drugs, potentially leading to the inability of first-line ACTs to effectively treat malaria. To better appreciate the current situation, we directly compared the drug susceptibilities of isolates collected in 2021 from malaria patients in northern Uganda, where the PfK13 mutations have been common in recent years, and eastern Uganda, where they have been uncommon. We found, as expected, high prevalence of the C469Y and A675V mutations in isolates from northern Uganda, although prevalence was also higher than previously seen in isolates from eastern Uganda21. Using the DHA RSA, the standard measure of in vitro susceptibility to artemisinins, we saw an association between the C469Y mutation, but not the A675V mutation (for which few samples were available for study), and decreased parasite survival. Using standard growth inhibition assays, susceptibility to lumefantrine and DHA, but not other tested drugs, was significantly lower in isolates from northern, compared to eastern Uganda. Considering a much larger number of isolates collected from 2015–21, but for which only growth inhibition assays were available, decreased susceptibility to lumefantrine was strongly associated with the PfK13 469Y mutation. These results suggest that emergence of partial resistance to artemisinins has been accompanied by decreased activity of lumefantrine, potentially foretelling loss of efficacy of artemether-lumefantrine, the first-line antimalarial in Uganda and most of Africa.
It is important to determine if the PfK13 mutations recently identified in northern Uganda19,20,21,22 are associated with increased parasite survival after exposure to artemisinins. Previous work identified association between the 675V mutation and clinical delayed clearance after treatment with artemisinins in southeast Asia7. In a recent study from northern Uganda both mutations were associated with clinical delayed clearance and only the 675V mutation with ex vivo increased survival after DHA exposure, but analyses were limited by relatively few mutant isolates for study22. A study from Rwanda showed that single isolates collected in 2019 with the 469 F, 561H, and 675 V mutations had in vitro increased survival compared to a wild type parasite18, but to our knowledge the 469Y mutation had not previously been associated with increased survival in an RSA. In our studies, the 469Y mutation was significantly associated with enhanced survival by RSA. Therefore, our results solidify the conclusion that both PfK13 mutations that emerged recently in northern Uganda are associated with artemisinin partial resistance.
Polymorphisms in a number of P. falciparum proteins have been shown to be associated with artemisinin partial resistance, either in conjunction with PfK13 mutations or independently8,10, but consistent mediators other than PfK13 have not been identified, and mediation of resistance appears to be highly dependent on parasite genetic background42. Our evaluation of associations between polymorphisms in 23 candidate genes and enhanced survival in the RSA identified a number of polymorphisms with modest association with enhanced survival (Supplementary Table 2), and the strongest association with polymorphisms in two genes, encoding falcipain-2a and Pfcoronin.
Strikingly, all isolates with RSA survival >5% despite lack of the PfK13 469Y mutation had mutations in falcipain-2a. Of the 17 mutations identified in falcipain-2a, 11 were also identified in isolates from southeast Asia in which falcipain-2a haplotypes were associated with enhanced RSA survival9. Falcipain-2a is a hemoglobinase that plays a key role, in concert with other proteases, in hydrolyzing hemoglobin to supply amino acids for parasite metabolism43. Loss of falcipain activity due to treatment with specific inhibitors or gene knockout markedly blunted the antimalarial activity of DHA, indicating that falcipain-mediated proteolysis of hemoglobin is needed for efficient activation of artemisinins44. These results are consistent with our understanding that the conversion of artemisinins by heme, after liberation from hemoglobin, into toxic free radicals, is a prerequisite to efficient action of artemisinins45. Interestingly, a mutation encoding a falcipain-2a stop codon was identified in parasites selected in vitro for resistance to artemisinin, but this selection occurred after emergence of a PfK13 mutation6. Taken together, available data suggest that certain mutations in falcipain-2a can mediate artemisinin partial resistance independent of or in concert with mutations in PfK13.
In studies of parasites from Senegal, in vitro selection of P. falciparum with increasing concentrations of DHA selected for parasites with enhanced survival associated with mutations in Pfcoronin, but not PfK1310; impacts of Pfcoronin mutations on survival after DHA exposure varied based on parasite genetic background46. Pfcoronin is a member of the WD40-propeller domain protein family that is known to associate with actin filaments and intracellular membranes47,48. The biological basis of contributions of Pfcoronin mutations to artemisinin partial resistance is unknown, but it was noted that impacts of Pfcoronin mutations are masked by PfK13 mutations, suggesting that mutations in the two proteins may impact on the same parasite mechanisms46.
Additional polymorphisms were associated with altered RSA survival. A deletion in pfubp1, which encodes a putative deubiquitinating enzyme, was associated with increased ring survival. Two mutations in the P. chabaudi homolog of this protein were associated with artemisinin resistance in a murine genetic cross49; mutations were linked to artemisinin partial resistance in P. falciparum in vitro50 and P. berghei in mice51, but not to clinical partial resistance52; and the protein was shown by affinity labeling to associate with PfK1353. Our results support these limited data identifying PfUBP1 mutations as potential secondary mediators of artemisinin partial resistance. Interestingly, the presence of any of 15 pre-propeller domain PfK13 mutations was associated with decreased survival. These results suggest that, perhaps paradoxically, these mutations enhance artemisinin activity, the opposite effect of propeller domain mutations. A polymorphism in a protein of unknown function (Pf3D7_1433800) was also associated with increased survival. A different polymorphism in this protein was selected in the same experiments that identified Pfcoronin as a potential resistance determinant10, but this did not appear to contribute to increased ring survival46.
We also compared susceptibility of P. falciparum isolates to a panel of seven antimalarials using a standard growth inhibition assay. Considering only isolates collected and studied over the same time frame in 2021, susceptibilities to two drugs, lumefantrine and DHA, were lower in isolates from northern Uganda than those from eastern Uganda. Considering a much larger set of isolates collected in 2015–21, polymorphisms in nine genes were associated with altered lumefantrine susceptibility compared to that of wild type parasites. These results highlight potential mediators of, or factors associated with, altered lumefantrine susceptibility. First, the PfK13 469Y and 675 V mutations were strongly associated with decreased susceptibility, highlighting the potential for partial resistance to artemisinins to be associated with decreased susceptibility to partner drugs. However, these results do not indicate a causal role for PfK13 mutations in altered lumefantrine susceptibility. Second, three mutations in the putative drug transporter PfMDR1 were associated with altered lumefantrine susceptibility; one of these, 86Y, was previously at high prevalence in Africa, was selected against by exposure to lumefantrine15, and was associated with increased drug susceptibility in prior studies31,32 and our current analysis. Third, mutations in a putative phospholipase were associated with altered lumefantrine susceptibility. Mutations in this protein were previously selected by in vitro exposure to primaquine and associated with decreased susceptibility to that drug54. Interestingly, loss-of-function mutations in another predicted P. falciparum phospholipase, PfPARE, were associated with decreased susceptibility to MMV011438, a series of pepstatin esters55, and the antimalarial candidate oxoborole AN1376256, presumably due to loss of intracellular drug activation. Fourth, different polymorphisms in a predicted P. falciparum transcription factor, ApiAP257, were associated with both increased and decreased lumefantrine susceptibility. Different mutations in this protein were associated with decreased susceptibility to three different compounds under development as antimalarials in a chemogenetic screen54 and to quinine in a genome-wide association study58. Fifth, mutations in the putative drug transporters PfMRP1 and PfMRP2 were associated with alterations in lumefantrine susceptibility. Other mutations in PfMRP1 have been described in African parasites and associated with prior therapy with artemether-lumefantrine59 and with decreased susceptibility to chloroquine, artemisinin, mefloquine, lumefantrine, piperaquine, and/or DHA in different studies60,61,62,63. A deletion in the PfMRP2 upstream promoter64 and a number of polymorphisms in the coding sequence65 were associated with decreased susceptibility to aminoquinolines. Sixth, SNPs in genes encoding hemoglobinases, the cysteine proteases falcipain-2a and falcipain-343 and the aspartic protease plasmepsin-I66, were associated with altered lumefantrine activity. As noted above, decreased activity of falcipain-2a through enzyme inhibition or gene knockout caused decreased susceptibility to artemisinins44, and altered function of other hemoglobinases might also impact on artemisinin action.
The identification of parasites with unusually high lumefantrine IC50s from northern Uganda led to interest in characterizing this phenotype. However, the phenotype proved to be unstable. Growth of parasites in culture for 4 or more weeks to establish culture adapted parasites was accompanied by an increase in susceptibility to lumefantrine. Thus, it appears that some parasites with decreased lumefantrine sensitivity are circulating in northern Uganda, but that, in the mixed isolates typically present in this region, the less susceptible strains are routinely out-competed by more drug sensitive strains during culture, and/or decreased susceptibility phenotypes are lost in vitro due to unexplained environmental differences between in vivo and in vitro growth of parasites.
Our study had some important limitations. First, due to the logistical challenges of studying isolates from Agago District in our laboratory in Tororo District (~400 km distant), we collected parasites for RSAs only over a 2-month period, limiting our analysis to 57 isolates from northern Uganda. Second, due to our interest in studying isolates collected during the same time interval, we were limited to analysis of RSAs for 42 isolates from eastern Uganda. The limited sample size limited the power of our RSA analyses. Third, participants who provided samples from northern and eastern Uganda differed in some respects, notably lower age and higher parasitemia in those from eastern Uganda; however, it is not expected that these differences would impact on ex vivo measures of drug susceptibility. Fourth, isolates were usually polyclonal, as typical for infections in high transmission regions of Africa. Ex vivo IC50s necessarily represented averages of activities of clones in a sample, and genomic analyses may have missed some sequences of minority clones. Fifth, our multiplex deep sequencing approach limited analysis of portions of some genes due to incomplete tiling or inadequately balanced PCR conditions. Sixth, our studies were limited to the target genes and not able to characterize the full complement of variation across the genome in relation to drug susceptibility; additional studies, including genome-wide association studies and genetic crosses, will be helpful in this regard. Despite these limitations, we feel that the robust associations identified are valid, but additional study of larger numbers of isolates collected across a wide geographic range are certainly a high priority.
The clinical ramifications of decreased activity of both artemisinins and lumefantrine against P. falciparum circulating in northern Uganda are unknown. Clearance of parasites with PfK13 469Y and 675 V mutations was delayed, compared to that of wild type parasites, after treatment with intravenous artesunate22. This result suggests that responses to treatment of severe malaria caused by mutant parasites may be slow, leading to increased severe morbidity and mortality. In Rwanda, clearance of parasites with a different PfK13 mutation, 561H, was delayed compared to that of wild type parasites, after treatment with artemether-lumefantrine, but treatment efficacy assessed by standard measures did not differ between patients infected with mutant and wild type parasites17. Impacts of the Ugandan 469Y and 675 V mutations on the treatment efficacies of ACTs are unknown. However, altered responses to both artemisinins and lumefantrine, as suggested by our data, appear likely to affect responses to therapy with artemether-lumefantrine, the first-line antimalarial in Uganda and most malaria-endemic countries in Africa. Studies in regions with PfK13 mutant parasites of the antimalarial efficacies of intravenous artesunate to treat severe malaria and of artemether-lumefantrine to treat uncomplicated malaria are thus of the highest priority.
Methods
Collection of P. falciparum isolates
For assessments that included RSAs and growth inhibition assays, samples were obtained from May 31–August 17, 2021 from 3 sites: Patongo Health Center III, Agogo District, in northern Uganda; Tororo District Hospital, Tororo District, in eastern Uganda; and Busiu Health Center IV, Mbale District, also in eastern Uganda (Fig. 1). For assessments that included only growth inhibition assays, samples were obtained from December, 2015-August, 2021 from the sites in eastern Uganda noted above, as well as Masafu Hospital, Busia District, also in eastern Uganda, as described previously32. For Patongo Health Center, samples were collected twice weekly and transported on the day of collection to our laboratory in Tororo. Samples from eastern Uganda sites were collected as available on a daily basis. Isolates were collected from patients aged 6 months or older presenting at the sites with clinical symptoms of malaria, a positive Giemsa-stained blood film for P. falciparum, and no signs of severe disease. Patients reporting use of antimalarial treatment within the previous 30 days or with evidence of an infection with other Plasmodium species were excluded. Written informed consent was obtained from all participants. Parents or guardians of children younger than 18 years provided written consent on their behalf; children aged 8–17 years provided assent. 2–5 mL of venous blood was collected in a heparin tube before the start of therapy. Participants were administered artemether-lumefantrine, following national guidelines, after sample collection. The studies were approved by the Makerere University Research and Ethics Committee, the Uganda National Council for Science and Technology, and the University of California, San Francisco Committee on Human Research.
Parasite culture and collection of samples for DNA analysis
Parasitemia was identified with Giemsa-stained thin films using a light microscope with a 100× objective lens and counting 1000 or more erythrocytes. Due to logistical considerations (samples collected at different times of the day and from different locations) samples were stored at 4 °C, with culture generally initiated on the morning after sample collection. Parasites were placed in culture as previously described32. Blood was centrifuged for 10 min at room temperature, plasma and buffy coat were removed, and the erythrocyte pellet was washed three times with RPMI 1640 media (Thermo Fisher Scientific, Waltham, MA, USA) at 37 °C. The pellet was resuspended in complete medium consisting of RPMI 1640 with 25 mM HEPES, 24 mM NaHCO3, 0.1 mM hypoxanthine, 10 μg/mL gentamicin, and 0.5% AlbuMAX II (Thermo Fisher Scientific, Waltham, MA, USA) to produce a hematocrit of 50%. In addition, 4 aliquots of the washed pellets of approximately 10 μL were spotted onto Whatman 3MM filter paper (Cytivia, Marlborough, MA, USA) for subsequent molecular analysis.
Ex vivo growth inhibition assays
Drug susceptibilities were evaluated in samples with a minimum of 0.3% parasitemia using a 72 h microplate growth inhibition assay with SYBR Green detection, as previously described32. Study compounds (chloroquine, monodesethylamodiaquine, piperaquine, lumefantrine, mefloquine, dihydroartemisinin, and pyronaridine), supplied by Medicines for Malaria Venture, were dissolved in dimethyl sulfoxide (except distilled water for chloroquine) as 10 mM stocks and stored at −20 °C. Drugs were serially diluted by a factor of 3 in complete medium in 96-well microplates (50 μL per well), including drug-free and parasite-free control wells, with concentrations optimized to capture full dose-response curves. Cultures were diluted with uninfected erythrocytes from local blood banks for total volumes of 200 μL per well at 0.2% parasitemia and 2% hematocrit. Plates were maintained at 5% CO2, 5% O2, and 90% N2 for 72 h at 37 °C in a humidified modular incubator (Billups Rothenberg, San Diego, CA, USA). After 72 h, well contents were resuspended and 100 μL culture per well was transferred to black 96-well plates containing 100 μL per well SYBR Green lysis buffer (20 mM Tris, 5 mM EDTA, 0.008% saponin, 0.08% Triton X-100, and 0.2 μL/mL SYBR Green I (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA)), and mixed. Plates were incubated for 1 h in the dark at room temperature, and fluorescence was then measured with a FLUOstar Omega plate reader (BMG LabTech, Cary, NC, USA; 485 nm excitation and 530 nm emission). To monitor stability of drug stocks, laboratory control P. falciparum Dd2 (MRA-156) and 3D7 (MRA-102) strains (BEI Resources, Manassas, VA, USA) were maintained in culture and assayed (beginning at the ring stage) approximately monthly, following synchronization with a magnetic column (Miltenyi Biotec, Auburn, CA, USA). For adaptation of parasites for long-term culture, freshly collected isolates were diluted to 1% parasitemia, if needed, using donor erythrocytes and cultured at 2% hematocrit in RPMI complete medium under the conditions described above. Cultures were diluted with uninfected erythrocytes as needed. After ~4 weeks, ring-stage parasites were cryopreserved in Glycerolyte-57 solution (Frensenius Kabi AG, Hamburg, Germany) and stored in gas-phase liquid nitrogen.
Ex vivo ring survival assays
Standard growth inhibition assays do not predict clinical delayed clearance associated with artemisinin-resistant parasites. Therefore, DHA susceptibility was measured using the ex vivo RSA, as previously described67. In brief, freshly cultured parasites with a minimum of 0.2% parasitemia, prepared as described above for growth inhibition assays, were incubated with 700 nM DHA or, for controls, 0.1% DMSO, for 6 h. Isolates with >1% parasitemia were diluted to 1%; isolates with ≤1% parasitemia were cultured at starting parasitemias. The cells were washed to remove drug after 6 h, and culture was continued for an additional 66 h. At 72 h after culture initiation, Giemsa-stained thin smears were prepared. Cultures were considered viable and appropriate for assessment if control parasitemia was ≥0.2% and also ≥25% of the starting parasitemia. Parasitemias were counted in control and treated cultures, and RSA survival was expressed as the proportion of viable parasites in the DHA treated cultures relative to controls.
Genomic characterization of isolates
Gene sequences and copy number were analyzed by MIP capture and deep sequencing, as previously described21,32,68. For MIP capture, we targeted a total of 80 genes, selected because of known or potential roles in altered susceptibility to standard antimalarials or compounds under development (Supplementary Table 1), using previously published and newly designed probes (Supplementary Table 9). Novel probes were designed using MIPTools software (version 0.19.12.13). DNA was isolated with Chelex-100 extraction buffer as previously reported, using 0.01% Tween 20 instead of saponin21. MIP capture, library preparation, and sequencing were done as previously described68. Sequencing reads are available in the National Center for Biotechnology Information (NCBI) Sequence Read Archive (accession number PRJNA850445). MIPTools was used to organize raw sequencing data and to perform variant calling. Individual genotypes were assigned for polymorphic sites that were covered by a minimum of 10 unique molecular identifiers (UMIs) and variants were required to have a within sample allele count ≥3 UMIs for alternate alleles and ≥2 UMIs for reference alleles. Copy numbers were estimated on the basis of sample and probe normalized depth of sequence coverage from 31 unique probes for pfmdr1 and 21 probes for plasmepsin 2/3. The Dd2 strain, which contains amplified pfmdr1 and is single copy for plasmepsin 2/3, and the G8 subclone of KH001_053 (kindly provided by Selina Bopp and the TRAC collaboration), which has multiple copies of plasmepsin 269, were used as controls. Complexity of infection (COI) was estimated from genotyping data generated by MIP sequencing using THE REAL McCOIL, a Markov chain Monte Carlo model that estimates the allele frequency and COI of samples70.
Statistical analysis
IC50 values were derived by plotting fluorescence intensity against log drug concentration and fit to a non-linear curve using a four-parameter Hill equation in Prism (version 9.0), as previously described32. All additional analyses were done in R (version 4.1.2). Categorical data were evaluated using two-sided Fisher’s Exact tests and continuous data, including growth inhibition assays and RSAs, with two-sided Mann–Whitney Wilcoxon tests. For evaluation of IC50 data, genotypes were considered as binary variables, determined by the presence or absence of the minor allele (mixed and pure minor allele genotypes were combined). P ≤ 0.01 were considered significant. For RSA survival, loci with high (>15%) prevalence of minor alleles were evaluated independently, as described above, and loci with low (≤15%) minor allele prevalence were analyzed as aggregate variables, in which the presence of any minor allele was compared with the major allele. For both high and low prevalence loci, p ≤ 0.05 were considered significant. For loci that were statistically significant, RSA survival was also evaluated in the context of K13 C469Y and A675V mutations. Candidate loci and K13 genotypes were treated as binary variables as described above.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All relevant data are available from the corresponding authors upon request. Sequence data are available in the National Center for Biotechnology Information (NCBI) Sequence Read Archive (accession number PRJNA850445). Data and code are available at https://github.com/PJRosenthalLab/2022_Tumwebaze_NatCom. Source data are provided with this paper.
References
Cui, L., Mharakurwa, S., Ndiaye, D., Rathod, P. K. & Rosenthal, P. J. Antimalarial drug resistance: literature review and activities and findings of the ICEMR network. Am. J. Trop. Med. Hyg. 93, 57–68 (2015).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361, 455–467 (2009).
Dhorda, M., Amaratunga, C. & Dondorp, A. M. Artemisinin and multidrug-resistant Plasmodium falciparum - a threat for malaria control and elimination. Curr. Opin. Infect. Dis. 34, 432–439 (2021).
Phyo, A. P. et al. Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet 379, 1960–1966 (2012).
Witkowski, B. et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in-vitro and ex-vivo drug-response studies. Lancet Infect. Dis. 13, 1043–1049 (2013).
Ariey, F. et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature 505, 50–55 (2014).
WWARN K13 Genotype-Phenotype Study Group. Association of mutations in the Plasmodium falciparum Kelch13 gene (Pf3D7_1343700) with parasite clearance rates after artemisinin-based treatments-a WWARN individual patient data meta-analysis. BMC Med. 17, 1 (2019).
Miotto, O. et al. Genetic architecture of artemisinin-resistant Plasmodium falciparum. Nat. Genet. 47, 226–234 (2015).
Siddiqui, F. A. et al. Plasmodium falciparum falcipain-2a polymorphisms in southeast Asia and their association with artemisinin resistance. J. Infect. Dis. 218, 434–442 (2018).
Demas, A. R. et al. Mutations in Plasmodium falciparum actin-binding protein coronin confer reduced artemisinin susceptibility. Proc. Natl. Acad. Sci. USA 115, 12799–12804 (2018).
Chenet, S. M. et al. Independent emergence of the Plasmodium falciparum kelch propeller domain mutant allele C580Y in Guyana. J. Infect. Dis. 213, 1472–1475 (2016).
Das, S., Manna, S., Saha, B., Hati, A. K. & Roy, S. Novel pfkelch13 gene polymorphism associates with artemisinin resistance in eastern India. Clin. Infect. Dis. 69, 1144–1152 (2019).
Miotto, O. et al. Emergence of artemisinin-resistant Plasmodium falciparum with kelch13 C580Y mutations on the island of New Guinea. PLoS Pathog. 16, e1009133 (2020).
Rosenthal, P. J. Artemisinin resistance outside of southeast Asia. Am. J. Trop. Med. Hyg. 99, 1357–1359 (2018).
Conrad, M. D. & Rosenthal, P. J. Antimalarial drug resistance in Africa: the calm before the storm? Lancet Infect. Dis. 19, e338–e351 (2019).
Uwimana, A. et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 26, 1602–1608 (2020).
Uwimana, A. et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect. Dis. 21, 1120–1128 (2021).
van Loon, W. et al. In vitro confirmation of artemisinin resistance in Plasmodium falciparum from patient isolates, southern Rwanda, 2019. Emerg. Infect. Dis. 28, 852–855 (2022).
Ikeda, M. et al. Artemisinin-resistant Plasmodium falciparum with high survival rates, Uganda, 2014-2016. Emerg. Infect. Dis. 24, 718–726 (2018).
Asua, V. et al. Changing molecular markers of antimalarial drug sensitivity across Uganda. Antimicrob. Agents Chemother. 63, e01818–e01818 (2019).
Asua, V. et al. Changing prevalence of potential mediators of aminoquinoline, antifolate, and artemisinin resistance across Uganda. J. Infect. Dis. 223, 985–994 (2021).
Balikagala, B. et al. Evidence of artemisinin-resistant malaria in Africa. N. Engl. J. Med. 385, 1163–1171 (2021).
Nosten, F. & White, N. J. Artemisinin-based combination treatment of falciparum malaria. Am. J. Trop. Med. Hyg. 77, 181–192 (2007).
Phyo, A. P. et al. Declining efficacy of artemisinin combination therapy against P. falciparum malaria on the Thai-Myanmar border (2003–2013): the role of parasite genetic factors. Clin. Infect. Dis. 63, 784–791 (2016).
Amaratunga, C. et al. Dihydroartemisinin-piperaquine resistance in Plasmodium falciparum malaria in Cambodia: a multisite prospective cohort study. Lancet Infect. Dis. 16, 357–365 (2016).
Amato, R. et al. Genetic markers associated with dihydroartemisinin-piperaquine failure in Plasmodium falciparum malaria in Cambodia: a genotype-phenotype association study. Lancet Infect. Dis. 17, 164–173 (2017).
Witkowski, B. et al. A surrogate marker of piperaquine-resistant Plasmodium falciparum malaria: a phenotype-genotype association study. Lancet Infect. Dis. 17, 174–183 (2017).
van der Pluijm, R. W. et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect. Dis. 19, 952–961 (2019).
Trape, J. F. The public health impact of chloroquine resistance in Africa. Am. J. Trop. Med. Hyg. 64, 12–17 (2001).
Mwai, L. et al. Genome wide adaptations of Plasmodium falciparum in response to lumefantrine selective drug pressure. PLoS One 7, e31623 (2012).
Rasmussen, S. A. et al. Changing antimalarial drug sensitivities in Uganda. Antimicrob. Agents Chemother. 61, e01516–e01517 (2017).
Tumwebaze, P. K. et al. Drug susceptibility of Plasmodium falciparum in eastern Uganda: a longitudinal phenotypic and genotypic study. Lancet Microbe 2, e441–e449 (2021).
Venkatesan, M. et al. Polymorphisms in Plasmodium falciparum chloroquine resistance transporter and multidrug resistance 1 genes: parasite risk factors that affect treatment outcomes for P. falciparum malaria after artemether-lumefantrine and artesunate-amodiaquine. Am. J. Trop. Med. Hyg. 91, 833–843 (2014).
Mungthin, M. et al. Association between the pfmdr1 gene and in vitro artemether and lumefantrine sensitivity in Thai isolates of Plasmodium falciparum. Am. J. Trop. Med. Hyg. 83, 1005–1009 (2010).
Kubota, R., Ishino, T., Iwanaga, S. & Shinzawa, N. Evaluation of the effect of gene duplication by genome editing on drug resistance in Plasmodium falciparum. Front. Cell Infect. Microbiol 12, 915656 (2022).
Balikagala, B. et al. Recovery and stable persistence of chloroquine sensitivity in Plasmodium falciparum parasites after its discontinued use in Northern Uganda. Malar. J. 19, 76 (2020).
Fukuda, N. et al. Ex vivo susceptibility of Plasmodium falciparum to antimalarial drugs in Northern Uganda. Parasitol. Int. 81, 102277 (2021).
Yeka, A. et al. Artesunate/amodiaquine versus artemether/lumefantrine for the treatment of uncomplicated malaria in Uganda: a randomized trial. J. Infect. Dis. 213, 1134–1142 (2016).
Ebong, C. et al. Efficacy and safety of artemether-lumefantrine and dihydroartemisinin-piperaquine for the treatment of uncomplicated Plasmodium falciparum malaria and prevalence of molecular markers associated with artemisinin and partner drug resistance in Uganda. Malar. J. 20, 484 (2021).
Ross, L. S. et al. Emerging Southeast Asian PfCRT mutations confer Plasmodium falciparum resistance to the first-line antimalarial piperaquine. Nat. Commun. 9, 3314 (2018).
Dhingra, S. K., Small-Saunders, J. L., Menard, D. & Fidock, D. A. Plasmodium falciparum resistance to piperaquine driven by PfCRT. Lancet Infect. Dis. 19, 1168–1169 (2019).
Stokes, B. H. et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. Elife 10, e66277 (2021).
Rosenthal, P. J. Falcipain cysteine proteases of malaria parasites: An update. Biochim Biophys. Acta. Proteins Proteom. 1868, 140362 (2020).
Klonis, N. et al. Artemisinin activity against Plasmodium falciparum requires hemoglobin uptake and digestion. Proc. Natl. Acad. Sci. USA 108, 11405–11410 (2011).
Wang, J., Xu, C., Lun, Z. R. & Meshnick, S. R. Unpacking ‘artemisinin resistance’. Trends Pharm. Sci. 38, 506–511 (2017).
Sharma, A. I. et al. Genetic background and PfKelch13 affect artemisinin susceptibility of PfCoronin mutants in Plasmodium falciparum. PLoS Genet. 16, e1009266 (2020).
Tardieux, I. et al. Plasmodium falciparum novel gene encoding a coronin-like protein which associates with actin filaments. FEBS Lett. 441, 251–256 (1998).
Olshina, M. A. et al. Plasmodium falciparum coronin organizes arrays of parallel actin filaments potentially guiding directional motility in invasive malaria parasites. Malar. J. 14, 280 (2015).
Hunt, P. et al. Gene encoding a deubiquitinating enzyme is mutated in artesunate- and chloroquine-resistant rodent malaria parasites. Mol. Microbiol. 65, 27–40 (2007).
Henrici, R. C., van Schalkwyk, D. A., Sutherland, C. J. Modification of pfap2mu and pfubp1 markedly reduces ring-stage susceptibility of Plasmodium falciparum to artemisinin in vitro. Antimicrob Agents Chemother 64, e01542–19 (2019).
Simwela, N. V. et al Experimentally engineered mutations in a ubiquitin hydrolase, UBP-1, modulate in vivo susceptibility to artemisinin and chloroquine in Plasmodium berghei. Antimicrob Agents Chemother 64, e02484–19 (2020).
Imwong, M. et al. Exploring the contribution of candidate genes to artemisinin resistance in Plasmodium falciparum. Antimicrob. Agents Chemother. 54, 2886–2892 (2010).
Birnbaum, J. et al. A Kelch13-defined endocytosis pathway mediates artemisinin resistance in malaria parasites. Science 367, 51–59 (2020).
Cowell, A. N. et al. Mapping the malaria parasite druggable genome by using in vitro evolution and chemogenomics. Science 359, 191–199 (2018).
Istvan, E. S. et al. Esterase mutation is a mechanism of resistance to antimalarial compounds. Nat. Commun. 8, 14240 (2017).
Sindhe, K. M. V. et al. Plasmodium falciparum resistance to a lead benzoxaborole due to blocked compound activation and altered ubiquitination or sumoylation. mBio 11, e02640–19 (2020).
Jeninga, M. D., Quinn, J. E., Petter, M. ApiAP2 transcription factors in apicomplexan parasites. Pathogens 8, 47 (2019).
Wendler, J. P. et al. A genome wide association study of Plasmodium falciparum susceptibility to 22 antimalarial drugs in Kenya. PLoS One 9, e96486 (2014).
Dahlstrom, S. et al. Plasmodium falciparum multidrug resistance protein 1 and artemisinin-based combination therapy in Africa. J. Infect. Dis. 200, 1456–1464 (2009).
Veiga, M. I. et al. Novel polymorphisms in Plasmodium falciparum ABC transporter genes are associated with major ACT antimalarial drug resistance. PLoS One 6, e20212 (2011).
Hao, M. et al. In vitro sensitivities of Plasmodium falciparum isolates from the China-Myanmar border to piperaquine and association with polymorphisms in candidate genes. Antimicrob. Agents Chemother. 57, 1723–1729 (2013).
Phompradit, P., Muhamad, P., Chaijaroenkul, W. & Na-Bangchang, K. Genetic polymorphisms of candidate markers and in vitro susceptibility of Plasmodium falciparum isolates from Thai-Myanmar border in relation to clinical response to artesunate-mefloquine combination. Acta. Trop. 139, 77–83 (2014).
Bai, Y. et al. Longitudinal surveillance of drug resistance in Plasmodium falciparum isolates from the China-Myanmar border reveals persistent circulation of multidrug resistant parasites. Int J. Parasitol. Drugs Drug Resist 8, 320–328 (2018).
Mok, S. et al. Structural polymorphism in the promoter of pfmrp2 confers Plasmodium falciparum tolerance to quinoline drugs. Mol. Microbiol 91, 918–934 (2014).
Veiga, M. I. et al. Complex polymorphisms in the Plasmodium falciparum multidrug resistance protein 2 gene and its contribution to antimalarial response. Antimicrob. Agents Chemother. 58, 7390–7397 (2014).
Nasamu, A. S., Polino, A. J., Istvan, E. S. & Goldberg, D. E. Malaria parasite plasmepsins: More than just plain old degradative pepsins. J. Biol. Chem. 295, 8425–8441 (2020).
Cooper, R. A. et al. Lack of artemisinin resistance in Plasmodium falciparum in Uganda vased on parasitological and molecular assays. Antimicrob. Agents Chemother. 59, 5061–5064 (2015).
Verity, R. et al. The impact of antimalarial resistance on the genetic structure of Plasmodium falciparum in the DRC. Nat. Commun. 11, 2107 (2020).
Bopp, S. et al. Plasmepsin II-III copy number accounts for bimodal piperaquine resistance among Cambodian Plasmodium falciparum. Nat. Commun. 9, 1769 (2018).
Chang, H. H. et al. THE REAL McCOIL: A method for the concurrent estimation of the complexity of infection and SNP allele frequency for malaria parasites. PLoS Comput. Biol. 13, e1005348 (2017).
Acknowledgements
The study was funded by the National Institutes of Health (AI075045 (P.J.R.), AI089674 (P.J.R.), TW007375 (P.J.R.), and AI139520 (J.A.B.)) and the Medicines for Malaria Venture (RD/15/0001 (P.J.R.)). We thank study participants and staff members of the clinics where samples were collected. We thank Selina Bopp, Sarah Volkman and the members of the TRAC collaboration for kindly providing a KH001_053 clone as a copy number control.
Author information
Authors and Affiliations
Contributions
All authors conceived and designed the experiments; P.K.T., M.D.C., M.O., S.O., O.B., T.K., J.L, S.G., D.G., S.R.S., F.G.C., and R.A.C. acquired the data; P.K.T., M.D.C., M.O., S.O., T.K., S.G., D.G., J.A.B., R.A.C., and P.J.R. analysed and interpreted the data; P.K.T., M.D.C., S.L.N., J.A.B, R.A.C., and P.J.R. played primary roles in writing the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Colin Sutherland, Didier Menard, Dulcie Lautu-Gumal and the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tumwebaze, P.K., Conrad, M.D., Okitwi, M. et al. Decreased susceptibility of Plasmodium falciparum to both dihydroartemisinin and lumefantrine in northern Uganda. Nat Commun 13, 6353 (2022). https://doi.org/10.1038/s41467-022-33873-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-33873-x
This article is cited by
-
Limited threat of Plasmodium falciparum pfhrp2 and pfhrp3 gene deletion to the utility of HRP2-based malaria RDTs in Northern Uganda
Malaria Journal (2024)
-
Emergence, transmission dynamics and mechanisms of artemisinin partial resistance in malaria parasites in Africa
Nature Reviews Microbiology (2024)
-
Clinical isolates of uncomplicated falciparum malaria from high and low malaria transmission areas show distinct pfcrt and pfmdr1 polymorphisms in western Ethiopia
Malaria Journal (2023)
-
A review of efficacy and safety of Ugandan anti-malarial plants with application of RITAM score
Malaria Journal (2023)
-
Antimalarial drug discovery: progress and approaches
Nature Reviews Drug Discovery (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.