Abstract
Carriers of germline biallelic pathogenic variants in the MUTYH gene have a high risk of colorectal cancer. We test 5649 colorectal cancers to evaluate the discriminatory potential of a tumor mutational signature specific to MUTYH for identifying biallelic carriers and classifying variants of uncertain clinical significance (VUS). Using a tumor and matched germline targeted multi-gene panel approach, our classifier identifies all biallelic MUTYH carriers and all known non-carriers in an independent test set of 3019 colorectal cancers (accuracy = 100% (95% confidence interval 99.87–100%)). All monoallelic MUTYH carriers are classified with the non-MUTYH carriers. The classifier provides evidence for a pathogenic classification for two VUS and a benign classification for five VUS. Somatic hotspot mutations KRAS p.G12C and PIK3CA p.Q546K are associated with colorectal cancers from biallelic MUTYH carriers compared with non-carriers (p = 2 × 10−23 and p = 6 × 10−11, respectively). Here, we demonstrate the potential application of mutational signatures to tumor sequencing workflows to improve the identification of biallelic MUTYH carriers.
Similar content being viewed by others
Introduction
Genome-wide tumor profiling and associated computational approaches can provide a historical record of the mutational processes, both endogenous and exogenous, that were active during tumor initiation and progression, providing a tumor mutational signature (TMS) profile1,2. Several of these TMSs have been mechanistically shown to result from genetic defects related to homologous recombination repair deficiency3, DNA mismatch repair deficiency4, and base excision repair deficiency5,6, including in colorectal cancer (CRC)7,8. Therefore, TMSs can represent a functional manifestation of specific alterations in DNA repair pathways, with the potential application for not only identifying tumors caused by inherited defects in DNA repair genes but also providing functional evidence to support variant classification approaches in these DNA repair genes. The increasing application of tumor sequencing to identify targets for personalized therapy provides an opportunity to implement TMS analysis to gain additional clinically relevant knowledge on hereditary susceptibility earlier.
Identifying pathogenic variants in CRC and polyposis susceptibility genes has important implications for preventing subsequent primary cancers in the carrier6,9,10 and for the prevention of CRC in relatives through targeted screening approaches such as colonoscopy with polypectomy. The most common recessively inherited CRC and polyposis susceptibility genes include MUTYH11,12, and NTHL16,13. Germline carriers of biallelic pathogenic variants in the MUTYH gene are almost certain to develop CRC, although monoallelic carriers of a MUTYH pathogenic variant may have only a small increased risk of CRC14. Current indications for germline testing for MUTYH include >20 colonic adenomas, although the phenotype has been described as variable where some biallelic MUTYH carriers develop CRC without the associated polyposis, suggesting biallelic MUTYH carriers may be missed with this current approach15. Unlike Lynch syndrome, where DNA mismatch repair immunohistochemistry is used on tumor samples for triaging patients to identify pathogenic variant carriers, no tumor-based biomarkers or testing approaches are currently used in diagnostic pathology to triage people for identifying germline biallelic MUTYH carriers.
A TMS profile characteristic of biallelic inactivation of MUTYH has been described in CRC5,16 and in other cancer types17. In previous work we evaluated all the existing specific single base substitution (SBS) and indel (ID) TMS using whole-exome sequencing of CRCs, demonstrating that the SBS TMSs, SBS18, and SBS36, when combined were the dominant TMSs in CRCs from biallelic MUTYH pathogenic variant carriers7. To support the application of SBS18 and SBS36 in the clinical setting, further evidence related to the accuracy of this approach is needed, particularly when applied to targeted panel sequencing data. Furthermore, our previous work generated the hypothesis that a combined SBS18 and SBS36 TMS could be applied to support the classification of germline MUTYH variants of uncertain clinical significance (VUS).
In this study, we: (1) evaluate the performance of SBS18 and SBS36 TMSs to identify germline biallelic pathogenic variant carriers and classify variants in the MUTYH gene in a large series of CRCs from the Genetic Epidemiology of Colorectal cancer Consortium (GECCO) tested with custom-designed targeted tumor sequencing assays, and (2) identify somatic mutation associations with biallelic MUTYH carriers within the somatic mutation landscape of CRCs.
Results
Distribution and classifications of CRCs across the study
The germline and somatic variants identified in MUTYH from all 5649 CRCs assessed in this study are summarized in Supplementary Fig. 1. Each tumor was categorized into one of five groups based on carriership of MUTYH variants and their classification as pathogenic, benign, or VUS (further defined in Supplementary Table 1): (1) MUTYH positives: tumors in people found to be germline carriers of two pathogenic variants (compound heterozygotes) or a homozygous pathogenic variant in MUTYH; (2) MUTYH monoallelics: tumors with only one germline heterozygous pathogenic variant in MUTYH and no other germline potential pathogenic variants; (3) MUTYH negatives: tumors with no germline or somatic pathogenic or potential pathogenic variants identified in MUTYH; (4) potential MUTYH biallelics: tumors in people homozygous for a germline potentially pathogenic variant or with two variants classified as either pathogenic or potentially pathogenic, but not two pathogenic variants; and (5) MUTYH uncertain: tumors in people with only one heterozygous potentially pathogenic or heterozygous somatic pathogenic variant.
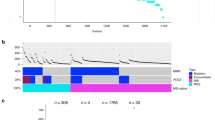
The tumors assessed were derived from 18 studies (Supplementary Table 2). The study design and distribution of tumors into training, validation, and test sets are summarized in Fig. 1. The demographic and clinic-pathological characteristics of the 5649 CRCs by training, validation, and test sets, by tumor MUTYH classification, and by recruiting study are shown in Supplementary Tables 2–5, respectively.
The SBS18/SBS36 TMS threshold was established using 102 CRCs down-sampled from whole-exome sequenced (WES) to intersect with the 1.34 Mb capture used to sequence the CRC tumors in the validation set. The 2528 CRCs sequenced with 1.34 Mb capture as part of the validation set were used to refine the SBS18/SBS36 classifier by including the somatic mutation count and TMS reconstruction error. The accuracy of the refined classifier was assessed using 3019 CRC tumors sequenced with a 1.96 Mb capture as part of the test set. The refined classifier was subsequently applied to 79 CRCs from monoallelic MUTYH pathogenic variant carriers, and CRCs defined as potential MUTYH biallelics and MUTYH uncertain status to determine its utility in variant classification. CI confidence interval, CIDR Center for Inherited Disease Research, CRC colorectal cancer, GECCO Genetic Epidemiology of Colorectal cancer Consortium, Mb megabase, OICR Ontario Institute of Cancer Research, PV pathogenic variant, SBS single bases substitution, TMS tumor mutational signature, VUS variant of uncertain clinical significance.
Pathogenic variants in MUTYH
The pathogenic variants and clinicopathological characteristics of each of the 19 CRCs from biallelic MUTYH carriers are detailed in Supplementary Table 6. No MUTYH positive tumor showed microsatellite instability (MSI) according to MSIseq predictions. There were 79 monoallelic MUTYH pathogenic variant carriers and 17 potential MUTYH biallelics identified (Supplementary Table 7). Figure 2 summarizes the overall TMS profiles of the 19 MUTYH positive CRCs and the 17 CRCs from potential MUTYH biallelics (expanded to include all CRCs from MUTYH monoallelic carriers in Supplementary Fig. 2). Supplementary Fig. 3 and Supplementary Table 8 summarize the aggregated contexts and mutational signatures observed for each tumor class, respectively.
SBS18/36 TMS threshold for identifying CRCs from MUTYH positives and its accuracy for discriminating MUTYH positives from MUTYH negatives
From the training set of 102 CRCs, including 8 MUTYH positive CRCs, we calculated the likelihood of biallelic MUTYH base excision repair deficiency TMS to be 95% when the sum of SBS18 and SBS36 exceeded 51% (range from 60.2 to 93.4%; Supplementary Table 9; Supplementary Fig. 4). We then assessed the accuracy of this baseline SBS18/36 classifier on the validation set of 2528 CRCs. All 6 MUTYH positives were correctly identified using the 51% SBS18/36 threshold, with no false negatives (Fig. 3a). Of the 2424 MUTYH negative CRCs, 45 were incorrectly classified as MUTYH positive and thus considered false positives. Therefore, the baseline classifier achieved 98.1% accuracy (95% confidence interval 97.5–98.6%), with 100% sensitivity (54.1–100%) and 98.1% specificity (97.5–98.6%) when applied to the validation set.
Distribution of a SBS18/SBS36 tumor mutational signature, b tumor mutational signature reconstruction error, and c adjusted somatic SNV count across 5649 CRCs in the training set, validation set, and test set, grouped by germline pathogenic variant status (tumor classifications). The red horizontal line in each figure indicates the cut-offs that were determined based on the training set and validation set tumors. All boxes correspond to the 25th and 75th percentiles and the whiskers represent 1.5× the inter-quartile range (IQR) extending from the boxes. Lines at the middle of each box show the median. Individual observations are shown beyond the whiskers. Source data are provided as a Source Data file.
The number of somatic mutations and degree of TMS reconstruction error are associated with false positive SBS18/36 TMS
We confirmed the absence of pathogenic variants in the 45 false positives by examining the sequencing data for any pathogenic variants that may have been overlooked by the variant calling pipeline. To determine features that could improve classification accuracy, we assessed each tumor’s somatic mutation count and TMS reconstruction error. The MUTYH positive CRCs from the training set (n = 8) and from the validation set (n = 6) exhibited a somatic mutation count ranging from 9 to 32 (mean ± SD 20.8 ± 7.8). In contrast, the 45 false positive CRCs from the validation set exhibited significantly lower somatic mutation counts, ranging from 1 to 12 (mean ± SD of 5.1 ± 2.6; p = 8 × 10−17, t-test). The 14 MUTYH positives from the training and validation sets exhibited reconstruction error ranging from 8.9 to 32.7% (mean ± SD 19.8 ± 8.3%), whereas the 45 false positive CRCs showed significantly higher reconstruction error ranging from 20.6 to 73.1% (mean ± SD 54.0 ± 11.5%; p = 1 × 10−14, t-test). By considering somatic mutation count and reconstruction error, the 45 false positives could be differentiated from the 14 MUTYH positives, evidenced by 43 of 45 CRCs (96%) having a reconstruction error >39%, and 40 of 45 (89%) having <9 somatic mutations (Figs. 3a–c, 4a, b). Combining these two constraints eliminated all false positives while still detecting all 14 MUTYH positives, providing an optimized MUTYH TMS classifier.
a The CRCs from the biallelic MUTYH pathogenic variant carriers cluster together based on high SBS18/SBS36 TMS and low TMS reconstruction error highlighting the need to include TMS reconstruction error in classifier, and b CRCs with greater than 95% likelihood of arising from biallelic MUTYH pathogenic variants based on TMS. The number of SNV mutations used in determining TMS (horizontal axis) and the TMS reconstruction error (vertical axis) demonstrates the importance of low reconstruction error (<39%) and sufficient somatic mutation count (≥9) for correctly classifying tumors from biallelic MUTYH pathogenic variant carriers (true positives). Source data are provided as a Source Data file.
Evaluating the optimized MUTYH TMS classifier on an independent test set of CRCs
We applied this optimized classifier, comprising SBS18 + SBS36 > 51%, reconstruction error <39%, and somatic mutation count ≥9, to the independent test set (n = 3019), with the somatic mutation counts adjusted for the differing panel sizes. All five MUTYH positives and all 2848 MUTYH negatives were correctly identified. This corresponds to 100% accuracy (95% CI 99.87–100%), sensitivity (47.8–100%), and specificity (99.87–100%) (Fig. 1), demonstrating the classifier’s likely generalizability to independent data.
Classifying CRCs from MUTYH monoallelics and potential MUTYH biallelics
The SBS18/36 TMS was significantly higher in biallelic MUTYH carrier CRCs compared with both non-MUTYH carrier CRCs (p = 3 × 10−112, t-test) and monoallelic MUTYH pathogenic variant carrier CRCs (p = 5 × 10−29, t-test). When applying our optimized classifier, none of the 79 MUTYH monoallelics were classified as positive (Fig. 4a, b), demonstrating that monoallelic inactivation of MUTYH is insufficient to observe the SBS18/36 TMS in CRCs. To investigate somatic inactivation of the wildtype allele in the MUTYH monoallelics, we assessed loss of heterozygosity (LOH) as a potential second somatic event. Evidence of LOH across MUTYH was observed in 4% (224/5649) of CRCs in this study, but these tumors did not show significantly elevated SBS18/36. The 224 tumors with LOH spanning MUTYH were supported by 8.2 ± 7.2 mutations (mean ± sd) across the entire LOH region, with 1.8 ± 0.9 mutations within 100,000 bases of MUTYH. Public data suggests LOH does not commonly affect MUTYH: 0/60 Pan-Cancer Analysis of Whole Genomes (PCAWG) CRCs and 69/583 (12%) of The Cancer Genome Atlas (TCGA) CRCs showed evidence of copy number loss across MUTYH. Structural variants are similarly rare18. Four of the 79 (5%) MUTYH monoallelics exhibited LOH but none were classified as positive based on the classifier. Additionally, 61 tumors harbored pathogenic or potentially pathogenic somatic mutations in MUTYH across the entire cohort (1.1%), but no pathogenic somatic mutation in MUTYH was observed in any of the monoallelic CRCs, suggesting a second somatic event is a rare event in MUTYH monoallelic carriers. We did not observe any statistically significant association between SBS18/36 and tumor stage in the monoallelic or biallelic carriers (Supplementary Table 10 and Supplementary Fig. 5).
Given this differential in biallelic and monoallelic MUTYH carriers, we applied the optimized classifier to 17 potential MUTYH biallelic CRCs carrying more than one variant (germline or somatic) classified as either pathogenic or VUS to determine if the SBS18/36 TMS could provide functional evidence for biallelic inactivation and, therefore, support variant classification (Table 1). For two VUSs, p.G381W and c.577-5A>G, the TMSs provide support for pathogenicity (Table 1). Neither variant has been seen in gnomAD and have inconclusive computational predictions by REVEL and CADD, but the high observed TMS, in conjunction with acceptable reconstruction error, somatic mutation count, and no evidence for LOH, adds support for pathogenicity. Similarly, the high TMS observed in tumor C5024 suggests that one of these VUSs c.933+3A>C or p.A489T is likely to be pathogenic. For five VUSs, p.R426C, p.S304R, p.R274Q, p.R309C, and p.T477T, our classifier adds evidence suggesting that these variants are likely benign. In particular, p.R309C was homozygous in two independent tumors that the classifier predicted to be MUTYH negative. Participant O1569 carried the germline monoallelic pathogenic variant c.1187G>A p.G396D and a second germline variant c.821G>A p.R274Q classified as a VUS by ClinVar (REVEL 0.826; CADD 33). Previous studies suggest that c.R274Q mutant MUTYH has partial activity compared to wild-type protein19,20. In this tumor, ten somatic mutations were detected with high reconstruction error (45.8%) and SBS18/36 TMS of 24.9%—which suggests <1% likelihood of the tumor being related to biallelic MUTYH inactivation (Supplementary Table 9). This adds evidence that c.821G>A p.R274Q is likely benign.
Of the 170 tumors in MUTYH uncertain group (Supplementary Table 7), 169 were classified as MUTYH negative by the classifier. The single positive tumor exhibited high mutational burden (93.7 mutations/megabase (Mb)) and was found to harbor a germline potentially pathogenic variant in POLD1 (c.1225C>T p.R409W).
Somatic mutation landscape of CRCs from biallelic MUTYH pathogenic variant carriers
To evaluate the impact of biallelic inactivation of MUTYH on the somatic mutational landscape, we combined all 19 MUTYH positive tumors across the three datasets. We previously observed that SBS18 and SBS36 are associated with specific pathogenic variants in MUTYH7. Specifically, homozygous pathogenic variants at the 5′ end of the gene (exons 1–10) tend to give rise to SBS36, while SBS18 is more prevalent in homozygous pathogenic variants at the 3′ end of the gene. Comparing homozygous p.Y179C tumors to p.G396D homozygous tumors, SBS18 and SBS36 were both significantly different between these two groups of tumors (p = 0.015 and 0.024, respectively, t-test; Supplementary Fig. 6). Three additional carriers with homozygotes near p.G396D (c.1214C>T p.P405L, c.1227_1228dupGG p.E410Gfs*43 and c.1147del p.A385PfsTer23) support the possibility of domain-specific TMSs. When aggregated with the p.G396D tumors, we see similarly significant differences between the TMSs (p = 0.011 and 0.012 respectively, t-test; Supplementary Table 6).
Under the definition that hypermutated tumors have >10 mutations/Mb21, 12/19 (63.1%) MUTYH positives were considered hypermutated (mean ± SD 22.0 ± 8.8 somatic mutations). None showed evidence of MSI or somatic POLE exonuclease domain mutations. In comparison, 469 (10.4%) of the 4510 microsatellite stable MUTYH negative tumors were considered either hypermutated (n = 415) or ultra-hypermutated (n = 54) (>100 mutations/Mb21), representing a significant difference (p = 4 × 10−8, binomial test) (Fig. 3c).
Somatic mutations were compared between the 19 MUTYH positives and 5,352 MUTYH negatives (Fig. 5; expanded to include MUTYH monoallelic tumors in Supplementary Fig. 7). Several genes were found to have a significant enrichment of non-synonymous mutations in the MUTYH positives, including KRAS, PIK3CA, and AMER1 (Table 2), consistent with previous findings16. In KRAS and PIK3CA, a substantial proportion of all mutations could be attributed to specific individual mutations: p.G12C (KRAS) and p.Q546K (PIK3CA). We demonstrated the utility of these hotspot mutations on smaller panels, showing that they identify most biallelic carriers, though with lower sensitivity and specificity than can be achieved using a larger panel that incorporates SBS18/36 TMS (Supplementary Table 11). Both mutations were found to be mutation types highly specific to the SBS18 and SBS36 mutational trinucleotide contexts, supporting a link to the DNA damage profile associated with biallelic MUTYH inactivation. Similarly, the proportion of somatic mutations attributable to SBS18/36, measured as relative likelihood22, was higher in all enriched genes (Table 2), adding evidence that the association between MUTYH positives and these genes has a mechanistic basis.
The 40 most commonly mutated CRC genes48 are included, as well as known CRC genes ALK, CSMD1, POLE, and POLD1. KRAS was found to be significantly more commonly mutated in our biallelic MUTYH carrier CRCs. Source data are provided as a Source Data file. AgeDx age of diagnosis, TMB tumor mutational burden (mutations/Mb), TMS tumor mutational signature.
Discussion
We previously demonstrated that combining MUTYH-related base excision repair deficiency mutational signatures SBS18 and SBS36 was more effective than each signature alone for identifying germline biallelic MUTYH carriers using whole exome sequencing of CRC tumors7. In this study, we trained, validated, and then tested the effectiveness of our MUTYH SBS18/36 TMS classifier for identifying CRCs from biallelic MUTYH pathogenic variant carriers in a large cohort of 5649 tumors that underwent targeted multi-gene panel sequencing from formalin-fixed paraffin-embedded (FFPE) tissue DNA. The addition of somatic mutation count and TMS reconstruction error to the SBS18/36 threshold enabled the determination and validation of classifier parameters, namely SBS18/36 TMS proportion >51%, TMS reconstruction error <39%, and somatic mutation count ≥9, that yielded 100% accuracy for distinguishing MUTYH positives from MUTYH negatives when applied to an independent dataset. Furthermore, when the MUTYH TMS classifier was applied to a group of potential MUTYH biallelics as a functional approach to evaluate the pathogenicity of VUSs, we found support for two VUSs, p.G381W and c.577-5A>G, being likely pathogenic, while for five VUSs, p.S304R, p.R274Q, p.R426C, p.R309C, and p.T477T, our classifier provided evidence they were likely benign. Finally, we provided a detailed view of the somatic mutation landscape of CRCs from biallelic MUTYH pathogenic variant carriers based on a consensus set of 205 cancer genes, identifying specific mutations in KRAS and PIK3CA genes that were associated with CRC tumorigenesis in biallelic MUTYH carriers.
Effectiveness of TMSs to identify biallelic MUTYH carriers from targeted panel sequencing data
We demonstrated that the SBS18/36 TMS was robust when scaling down from a whole exome capture (67 Mb)7 to a 1.34 Mb capture in the training set. Furthermore, SBS18/36 remained highly correlated between the different capture sizes of the validation (1.34 Mb, ρ = 0.904) and test (1.96 Mb, ρ = 0.911) sets when compared with the whole exome capture (Supplementary Table 12). This is important for the generalizability and implementation of this MUTYH TMS classifier approach where tumor sequencing for clinical diagnostics is still largely embedded with targeted multi-gene panel testing rather than whole exome or whole genome sequencing. Developing and applying the classifier parameters on different capture sizes and assays (validation set = 1.34 Mb and test set = 1.96 Mb) while still achieving 100% accuracy supports the potential for a broad application of this approach to different clinical panels in use globally.
Resolving false positives in the TMS data
Despite demonstrating that the combined SBS18/36 TMS was effective at identifying CRCs from biallelic MUTYH carriers, the reduction in capture size from exome to the 1.34 Mb targeted panel required the inclusion of justifiable constraints in our classifier to eliminate false positives. By considering the number of observed somatic variants and the TMS reconstruction error, all 24 false positives observed in the independent dataset of 3022 CRCs were eliminated. Although the number of somatic mutations is a critical factor influencing the accuracy of reported TMSs, the literature lacks consensus recommending minimum mutation counts, with estimates ranging from 20023, 10024, 5025, down to 526. We showed that the presence of either of the two hotspot mutations KRAS p.G12C or PIK3CA p.Q546K resulted in 89.5% sensitivity (area under the curve 0.932) for detecting MUTYH positive CRCs, representing the lower limit of detection. For the 1.34 Mb capture, we found that tumors with reconstruction error >39% or carrying <9 somatic mutations were unlikely to generate a SBS18/36 TMS profile that was caused by biallelic inactivation of MUTYH. These measures are negatively correlated (ρ = −0.41) and exclude tumors for different reasons: the constraint on minimum somatic mutations reflects our previous finding that MUTYH positive CRCs exhibit significantly higher tumor mutational burden (TMB) than MUTYH negative mismatch repair (MMR)-proficient tumors7, confirmed by this larger study. The constraint on reconstruction error eliminates tumors with TMSs that are not strongly supported by the observed mutations. Increasing capture size tends to increase both mutation count and reduce TMS reconstruction error (Supplementary Tables 12 and 13) which will aid in reducing false positives and the resolution of cases that fall close to the current classifier thresholds. Calibration of the MUTYH TMS classifier for custom captures that are unique to individual diagnostic laboratories may be required for effective implementation.
Application to variant classification
We identified several key findings that support the incorporation of our MUTYH TMS classifier in variant classification approaches, mirroring the multifactorial approach adopted when classifying MMR variants:27,28 (1) Biallelic inactivation of MUTYH is necessary for generation of the SBS18/36 TMS, providing functional evidence of defective base excision repair, (2) the presence of the SBS18/36 TMS is a very strong predictor with 100% accuracy, (3) low false positive rate when TMS reconstruction error and somatic mutation count is added to the classifier for targeted panel sequencing data, and (4) somatic inactivation of MUTYH rarely occurs as evidenced by the rarity of second somatic hits in MUTYH monoallelics and no biallelic somatic inactivation was observed in 5649 CRCs.
Based on these key observations, the MUTYH TMS classifier supported pathogenicity for two VUSs and an absence of support for pathogenicity for five VUS. The MUTYH TMS classifier supported pathogenicity for at least one of c.933+3A>C and c.1465G>A p.A489T variants, although further work is needed to determine which one is or if they occur on a haplotype. Although the presence of the SBS18/36 TMS provides strong evidence for pathogenicity, the absence of the SBS18/36 TMS in supporting a likely benign classification should be considered with other factors, namely, the possibility the VUS is on the same allele as the pathogenic variant (in cis) and that we currently do not know if there is variability in deleterious effects of different pathogenic variants within MUTYH that result in a less dominant SBS18/36 TMS phenotype. Our findings support the application of the MUTYH TMS classifier as a tool to aid in variant classification approaches for MUTYH, and may help resolve some of the 58% (689 of 1190) of variants in MUTYH in ClinVar that are classified as either uncertain or with a conflicting classification.
Somatic landscape and segregation of SBS18 and SBS36
Evidence is accumulating that the two signatures, SBS18 and SBS36, segregate based on the MUTYH domain affected by the variant7: the presence of the c.1187G>A p.G396D pathogenic variant contributes predominantly to the SBS18 signature, while c.536A>G p.Y179C contributes predominantly to SBS36. Although SBS18 and SBS36 are similar signatures (cosine similarity 0.91) characterized by C>A transversions, they differ substantially in specific contexts: GCA>A, CCA>A, and ACA>A. This suggests that the affected domain alters tumor etiology, which could help us better understand the biology of tumors that arise and potentially inform clinical decision making. For example, both significantly enriched somatic mutations in KRAS c.34G>T p.G12C (CCA>A) and PIK3CA c.1636C>A p.Q546K (GCA>A) found in the MUTYH positives (Table 2) are in variant contexts that differ significantly between signatures, suggesting domain-specific hotspots that may inform treatment decision making.
The finding of commonly occurring specific somatic mutations and mutated genes has treatment implications. Cross-referencing the significant biomarkers found in this study with existing clinical actionability databases29 identified relevant drug associations, including FDA guidelines suggesting likely resistance to Cetuximab and Panitumumab (KRAS p.G12C), and pre-clinical trials suggesting responsiveness to MEK, ERK, BCL-XL, IGF-1R, PI3K pathway inhibitors, and BH3 mimetics. Further, clinical trials with direct inhibitors of the KRAS p.G12C allele30 are ongoing in CRC and represent a promising potential therapy for MUTYH positives. The FDA approval of the PD-1 inhibitor, pembrolizumab, as a therapy for tumors with TMB greater than 1031 is also clinically relevant, with our results indicating that most MUTYH positives are hypermutated (despite being MMR-proficient/microsatellite stable).
Limitations
We cannot exclude the possibility that other mechanisms may cause SBS18/36 TMS that are more difficult to detect using panel sequenced data, such as LOH or structural variants. We could not determine the impact tumor heterogeneity might have on TMS. This might be more impactful for MUTYH monoallelic carriers, where somatic inactivation of the wildtype allele may occur later in tumorigenesis, however, overall we found no significant increase in the SBS18/36 TMS for MUTYH monoallelic carrier CRCs compared with MUTYH negative CRCs (10.8 ± 15.4% v. 7.1 ± 12.4%, p = 0.45, t-test) supporting previous findings that monoallelic MUTYH pathogenic variants alone do not result in loss of base excision repair7. Doublet and indel signatures were not considered for this study due to low numbers in panel-sequenced data. The majority of our MUTYH positives carry the most common MUTYH pathogenic variants—by expanding the analysis to different ethnic groups and a broader diversity of MUTYH variants we can improve the generalizability of the MUTYH TMS classifier and potentially classify a greater number of MUTYH variants. Similarly, the application to non-CRCs needs to be investigated with the aim of developing a tumor agnostic MUTYH TMS classifier.
In conclusion, identifying germline biallelic MUTYH carriers is important for personalized surveillance and cancer prevention in carriers and cancer risk prediction in relatives. The variable clinical phenotype, lack of tumor-based screening to triage CRC-affected patients for MUTYH gene testing (akin to MMR immunohistochemistry for Lynch syndrome), conflicting reports regarding CRC risks in monoallelic MUTYH carriers, and the absence of validated functional assays for variant classification present important clinical challenges that limit effective identification and clinical management of MUTYH carriers. Key findings from this study address these current limitations, namely, the high accuracy of the tumor-based MUTYH TMS classifier for identifying biallelic MUTYH pathogenic variants and the absence of SBS18/36 TMS in MUTYH monoallelics enabled its application to variant classification; we re-classified seven germline VUSs, including supporting a likely pathogenic classification for two variants, c.1141G>T p.G381W and c.577-5A>G. The significantly enriched somatic mutations in KRAS c.34G>T p.G12C and PIK3CA c.1636C>A p.Q546K in MUTYH positive CRCs, where both mutations correspond to dominant contexts in SBS18/36, support a direct connection to MUTYH-related base excision repair deficiency and provide potential biomarkers for targeted therapy. With the increasing use of tumor sequencing for precision oncology and clinical diagnostics, our findings support the incorporation of our MUTYH TMS classifier into clinical tumor sequencing workflows as an accurate method to identify biallelic MUTYH pathogenic variant carriers, particularly when biallelic MUTYH status is not suspected, or when germline testing fails to yield a high-confidence resolution due to VUSs or conflicting results. Finally, the incorporation of analyses directed towards TMS for identifying hereditary subtypes could improve the detection of carriers and efforts to provide precision prevention of CRC.
Methods
Study participants
All participants provided written informed consent, and each study was approved by the relevant research ethics committee or institutional review board. The University of Melbourne Human Research Ethics Committee approved this research (study IDs 1750748, 1954921). Three independent sets of CRC-affected individuals (Fig. 1) were included in the study: (1) a training set of 102 CRCs with whole-exome sequencing from the Australasian Colon Cancer Family Registry (ACCFR; n = 47)32,33 and the ANGELS study (n = 55)7; (2) a validation set of 2906 CRCs from GECCO sequenced at the Ontario Institute for Cancer Research with a 1.34 Mb targeted panel covering 205 genes;34 and (3) a test set of 3093 CRCs and advanced adenomas from GECCO and sequenced at the Center for Inherited Disease Research with a 1.96 Mb targeted panel covering 350 genes. DNA was extracted from FFPE CRCs and matched with germline tissue (either blood-derived or normal mucosa). A description of each of the studies and the breakdown of the CRCs are provided in Supplementary Tables 2–5.
Tumor sequencing analysis
The mean coverage of MUTYH across the capture regions for the training, validation, and test tumor datasets was 581.2 ± 156.9, 753.9 ± 578.0, and 1542.5 ± 1176.8, respectively (mean ± SD) (Supplementary Fig. 8). For the training data, somatic variant calls were generated from the intersection of Strelka v2.9.235 and Mutect236, with minimum tumor sequencing depth of 25 reads and variant allele fraction of 10%. Variant calls were then limited to the same 1.34 Mb capture region as the validation set. For the panel-sequenced validation and test sets, somatic variants were generated from the intersection of Strelka v1.0.1547 and Mutect, as per34 (see Supplementary Methods for more detail). Tumors with at least one somatic single nucleotide variant (SNV) were included for analysis, which comprised 102, 2528, and 3019 tumors in the training, test, and validation sets, respectively, for a total of 5649 tumors assessed in this study (Fig. 1).
LOH in the tumor across MUTYH was determined by identifying germline heterozygous variants with homozygous somatic equivalents (see Supplementary Methods)4. Copy number loss was assessed in PCAWG and TCGA CRC cohorts with available consensus data37 and copy number segment data38, respectively (see Supplementary Methods). TMB was calculated as the combined number of SNVs, insertions, and deletions (indels) per megabase of capture sequence. MSI status was determined using the method described by MSIseq39. Reported transcript and protein changes in MUTYH refer to NM_001128425.1 and NP_001121897.1 respectively.
Germline MUTYH variant calling
The mean coverage of MUTYH across the capture regions for the training, test, and validation germline datasets was 372.0 ± 118.1, 280.4 ± 352.6, and 425.7 ± 321.5 respectively (mean ± SD) (Supplementary Fig. 8). Germline variants in the test and validation datasets were called using Strelka35 and limited to PASS calls with a minimum depth of 50 reads and a minimum variant allele fraction of 10%.
Variant Classifications
Variants classified by ClinVar40 as likely pathogenic or pathogenic were grouped and considered “pathogenic” for the purposes of this study (n = 18 unique variants). Variants of uncertain significance or with conflicting interpretations in ClinVar and/or variants that were predicted by computational metrics as pathogenic were retained and defined as “potentially pathogenic” variants (n = 105 unique variants) (Supplementary Fig. 1). The variant classification methods are detailed in the Supplementary Methods. The classified variants were then used to classify all tumors into five categories (Fig. 1 and Supplementary Table 1).
Tumor mutational signature (TMS) generation
TMSs were calculated for each of the 5649 CRCs using the simulated annealing method described by SignatureEstimation41, an approach previously applied successfully to panel-sequenced data42. The pre-defined set of Catalog of Somatic Mutations in Cancer (COSMIC) mutational signatures v3.143 was reduced to a set of 14 signatures previously observed in 59 whole-genome sequenced CRCs as determined in PCAWG1, including the known base excision repair signatures SBS18 and SBS36 associated with defective MUTYH16 and SBS30 associated with defective NTHL16,44. The TMS reconstruction error measures how accurately a reported signature profile reflects the observed mutations and was calculated as the cosine distance between the observed mutational context counts and the predicted mutational context counts computed from the mutational signatures45. We used the Python (v3.7.4) SciPy (v1.4.1)46 implementation of simulated annealing (“basinhopping”) to calculate the linear combination of TMSs that minimized reconstruction error.
Determining SBS18/36 TMS thresholds for identifying MUTYH positive CRCs
From the training set, 8 CRCs from known MUTYH positives and 92 confirmed MUTYH negatives were used to establish a combined SBS18 and SBS36 TMS threshold for identifying CRCs from biallelic MUTYH carriers that were specific to the targeted 1.34 Mb/205 gene panel (as previously applied to whole exome sequencing data7).
Predicting biallelic MUTYH carriers from the validation and test sets of CRCs and evaluating the accuracy of TMSs
Based on the combined SBS18/36 TMS threshold calculated from the training set of 100 CRCs, we predicted the MUTYH status of the validation set of CRCs and assessed its accuracy against the tumor classifications based on variant calling. The TMS-based classifier was then optimized using the validation set, by considering the number of somatic mutations and the TMS reconstruction error in addition to the SBS18/36 TMS threshold. The test set was then utilized as an independent dataset to assess the accuracy of the optimized classifier. The test set somatic mutation count was compared to the classifier threshold after adjusting by the proportional difference in panel sizes (1.34/1.96). To further assess the classifier’s utility for MUTYH variant classification, we applied it to CRCs defined as MUTYH monoallelics, potential MUTYH biallelics, and MUTYH uncertain (Fig. 1).
Statistical analyses
All statistical analyses were performed using Python 3.7.4. NumPy 1.17.347 was used for numerical calculations. Statistical calculations were performed using SciPy 1.4.146. All t-tests were performed as two-sided and assuming equal variance with all p-values reported unadjusted unless otherwise specified.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data generated in this study are included in this published article (and its supplementary information files/Source Data file). The original panel-sequenced data used in this study are available at the database of Genotypes and Phenotypes (dbGaP). The Ontario Institute of Cancer Research (OICR) data is available under accession code phs002050.v1.p1. The Center for Inherited Disease Research (CIDR) data is available under accession code phs001905.v1.p1. The whole exome sequencing data used in this study has been previously published7. This data is available from the Colon Cancer Family Registry via a “request to collaborate with the CCFR” application process (www.coloncfr.org/collaboration). Colorectal Adenocarcinoma TCGA copy number data was downloaded from cBioPortal (https://www.cbioportal.org/) using the data sequenced in the Colorectal Adenocarcinoma (TCGA, PanCancer Atlas) study. Copy number loss was assessed in the PCAWG with the consensus copy number data downloaded from https://dcc.icgc.org/releases/PCAWG/consensus_cnv. Mutational signature definitions were downloaded from the COSMIC website at https://cancer.sanger.ac.uk/signatures/downloads/. Source data are provided with this paper.
References
Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. Nature 578, 94–101 (2020).
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013).
Davies, H. et al. HRDetect is a predictor of BRCA1 and BRCA2 deficiency based on mutational signatures. Nat. Med. 23, 517–525 (2017).
Georgeson, P. et al. Tumor mutational signatures in sebaceous skin lesions from individuals with Lynch syndrome. Mol. Genet. Genom. Med. 7, e00781 (2019).
Pilati, C. et al. Mutational signature analysis identifies MUTYH deficiency in colorectal cancers and adrenocortical carcinomas. J. Pathol. 242, 10–15 (2017).
Grolleman, J. E. et al. Mutational signature analysis reveals NTHL1 deficiency to cause a multi-tumor phenotype. Cancer Cell 35, 256–266.e5 (2019).
Georgeson, P. et al. Evaluating the utility of tumour mutational signatures for identifying hereditary colorectal cancer and polyposis syndrome carriers. Gut https://doi.org/10.1136/gutjnl-2019-320462 (2021).
Pope, B. J. et al. Germline and tumor whole genome sequencing as a diagnostic tool to resolve suspected lynch syndrome. medRxiv. https://doi.org/10.1101/2020.03.12.20034991 (2020).
Win, A. K. et al. Risk of metachronous colon cancer following surgery for rectal cancer in mismatch repair gene mutation carriers. Ann. Surg. Oncol. 20, 1829–1836 (2013).
Win, A. K. et al. Risks of primary extracolonic cancers following colorectal cancer in lynch syndrome. J. Natl Cancer Inst. 104, 1363–1372 (2012).
Sieber, O. M. et al. Multiple colorectal adenomas, classic adenomatous polyposis, and germ-line mutations in MYH. N. Engl. J. Med. 348, 791–799 (2003).
Al-Tassan, N. et al. Inherited variants of MYH associated with somatic G:C–>T:A mutations in colorectal tumors. Nat. Genet. 30, 227–232 (2002).
Weren, R. D. A. et al. A germline homozygous mutation in the base-excision repair gene NTHL1 causes adenomatous polyposis and colorectal cancer. Nat. Genet. 47, 668–671 (2015).
Win, A. K. et al. Risk of colorectal cancer for carriers of mutations in MUTYH, with and without a family history of cancer. Gastroenterology 146, 1208–11.e1 (2014).
Balaguer, F. et al. Identification of MYH mutation carriers in colorectal cancer: A multicenter, case-control, population-based study. Clin. Gastroenterol. Hepatol. 5, 379–387 (2007).
Viel, A. et al. A specific mutational signature associated with DNA 8-oxoguanine persistence in MUTYH-defective colorectal cancer. EBioMedicine 20, 39–49 (2017).
Scarpa, A. et al. Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 543, 65–71 (2017).
ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium. Pan-cancer analysis of whole genomes. Nature 578, 82–93 (2020).
Komine, K. et al. Functional complementation assay for 47 MUTYH variants in a MutY-disrupted Escherichia coli strain. Hum. Mutat. 36, 704–711 (2015).
Ali, M. et al. Characterization of mutant MUTYH proteins associated with familial colorectal cancer. Gastroenterology 135, 499–507 (2008).
Campbell, B. B. et al. Comprehensive analysis of hypermutation in human cancer. Cell 171, 1042–1056.e10 (2017).
Gurjao, C. et al. Discovery and features of an alkylating signature in colorectal cancer. Cancer Discov. 11, 2446–2455 (2021).
Blokzijl, F., Janssen, R., van Boxtel, R. & Cuppen, E. MutationalPatterns: Comprehensive genome-wide analysis of mutational processes. Genome Med. 10, 33 (2018).
Rubanova, Y. et al. Reconstructing evolutionary trajectories of mutation signature activities in cancer using TrackSig. Nat. Commun. 11, 731 (2020).
Rosenthal, R., McGranahan, N., Herrero, J., Taylor, B. S. & Swanton, C. DeconstructSigs: Delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 17, 31 (2016).
Gulhan, D. C., Lee, J. J.-K., Melloni, G. E. M., Cortés-Ciriano, I. & Park, P. J. Detecting the mutational signature of homologous recombination deficiency in clinical samples. Nat. Genet. 51, 912–919 (2019).
Thompson, B. A. et al. A multifactorial likelihood model for MMR gene variant classification incorporating probabilities based on sequence bioinformatics and tumor characteristics: A report from the Colon Cancer Family Registry. Hum. Mutat. 34, 200–209 (2013).
Shirts, B. H. et al. Using somatic mutations from tumors to classify variants in mismatch repair genes. Am. J. Hum. Genet. 103, 19–29 (2018).
Tamborero, D. et al. Cancer Genome Interpreter annotates the biological and clinical relevance of tumor alterations. Genome Med. 10, 25 (2018).
McCormick, F. Sticking it to KRAS: Covalent inhibitors enter the clinic. Cancer Cell 37, 3–4 (2020).
Strickler, J. H., Hanks, B. A. & Khasraw, M. Tumor mutational burden as a predictor of immunotherapy response: is more always better? Clin. Cancer Res. 27, 1236–1241 (2021).
Newcomb, P. A. et al. Colon Cancer Family Registry: An international resource for studies of the genetic epidemiology of colon cancer. Cancer Epidemiol. Biomark. Prev. 16, 2331–2343 (2007).
Jenkins, M. A. et al. Cohort profile: The colon cancer family registry cohort (CCFRC). Int. J. Epidemiol. 47, 387–388i (2018).
Zaidi, S. H. et al. Landscape of somatic single nucleotide variants and indels in colorectal cancer and impact on survival. Nat. Commun. 11, 3644 (2020).
Kim, S. et al. Strelka2: Fast and accurate calling of germline and somatic variants. Nat. Methods 15, 591–594 (2018).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Dentro, S. C. et al. Characterizing genetic intra-tumor heterogeneity across 2658 human cancer genomes. Cell 184, 2239–2254.e39 (2021).
Cancer Genome Atlas Research Network. et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 45, 1113–1120 (2013).
Huang, M. N. et al. MSIseq: Software for assessing microsatellite instability from catalogs of somatic mutations. Sci. Rep. 5, 13321 (2015).
Landrum, M. J. et al. ClinVar: Improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 46, D1062–D1067 (2018).
Huang, X., Wojtowicz, D. & Przytycka, T. M. Detecting presence of mutational signatures in cancer with confidence. Bioinformatics 34, 330–337 (2018).
Zehir, A. et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat. Med. 23, 703–713 (2017).
Wellcome Sanger Institute. COSMIC signatures of mutational processes in human cancer. Signatures of Mutational Processes in Human Cancer https://cancer.sanger.ac.uk/cosmic/signatures (2019).
Grolleman, J. E., Díaz-Gay, M., Franch-Expósito, S., Castellví-Bel, S. & de Voer, R. M. Somatic mutational signatures in polyposis and colorectal cancer. Mol. Asp. Med. 69, 62–72 (2019).
Maura, F. et al. A practical guide for mutational signature analysis in hematological malignancies. Nat. Commun. 10, 2969 (2019).
Virtanen, P. et al. SciPy 1.0: Fundamental algorithms for scientific computing in Python. Nat. Methods 17, 261–272 (2020).
Harris, C. R. et al. Array programming with NumPy. Nature 585, 357–362 (2020).
Martínez-Jiménez, F. et al. A compendium of mutational cancer driver genes. Nat. Rev. Cancer 20, 555–572 (2020).
Acknowledgements
Funding from a National Health and Medical Research Council of Australia (NHMRC) project grant GNT1125269 (PI- Daniel Buchanan), and from NIH/NCI grants (U01CA137088, R01CA223498, and X01-HG009781; PI-Ulrike Peters) supported the design, analysis, and interpretation of data. Additional acknowledgements relating to co-authors and contributing studies are described in the Supplementary Methods as Supplementary Note 1.
Author information
Authors and Affiliations
Contributions
B.J.P., C.R., D.D.B., F.A.M., I.M.W., P.G., S.N.T,., and U.P. contributed to the conception and design of the research. A.G., A.T.C., D.D.B., E.L.A., F.A.M., G.G.G., H.B., I.M.W., J.C.C., J.D.P., J.E.M., M.A.J., M.H., M.J.G., M.O.S., P.L., P.T.C., R.E.S., S.G., S.I.B., S.N.T., S.O., U.P., V.M., and W.Y.H. contributed to the recruitment of study participants. A.G., A.J.F., A.T.C., C.Q., D.D.B., K.F.D., L.H., M.C., M.G., M.J.G., M.O.S., P.T.C., Q.M.T., R.S., R.W., S.H.Z., S.I.B., S.N.T., S.O., T.J.H., T.U., U.P., V.M., W.S., W.Y.H., and Y.L. contributed to sample preparation and quality control. A.J.F., B.J.P., C.Q., D.D.B., J.E.J., K.F.D., K.M., L.H., M.C., M.G., P.G., Q.M.T., R.N., R.S., S.H.Z., S.O., T.A.H., U.P., and Y.L. contributed to the data analysis. A.E.T., A.I.P., A.T.C., B.J.P., C.R., D.A.D., D.D.B., J.E.J., F.A.M., H.B., I.M.W., J.A.N., J.C.C., J.C.F., J.D.P., J.E.M., K.M., M.A.J., M.C., M.H., P.G., P.L., P.T.C., S.I.B., S.O., T.A.H., T.U., U.P., W.Y.H., and Y.C. contributed to the interpretation of findings. A.I.P., B.J.P., C.R., D.D.B., F.A.M., I.M.W., M.A.J., P.G., R.N., S.O., and U.P. drafted or substantively revised the manuscript. A.T.C., B.J.P., D.D.B., F.A.M., P.G., and U.P. contributed to the overall supervision of the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Andrew T. Chan performed consulting for Bayer Pharma AG, Pfizer Inc., Boehringer Ingelheim for work unrelated to this manuscript. Dr. Marios Giannakis received research funding from Bristol-Myers Squibb, Merck, Servier, and Janssen not related to this study. Dr. Paul Limburg serves as Chief Medical Officer for Screening at Exact Sciences through a contracted services agreement with Mayo Clinic. Dr. Limburg and Mayo Clinic have contractual rights to receive royalties through this agreement. Jonathan A. Nowak received research funding from Illumina and NanoString. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Ville Mustonen, Kasmintan Schrader, and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Georgeson, P., Harrison, T.A., Pope, B.J. et al. Identifying colorectal cancer caused by biallelic MUTYH pathogenic variants using tumor mutational signatures. Nat Commun 13, 3254 (2022). https://doi.org/10.1038/s41467-022-30916-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-30916-1
This article is cited by
-
Evaluation of an eight marker-panel including long mononucleotide repeat markers to detect microsatellite instability in colorectal, gastric, and endometrial cancers
BMC Cancer (2023)
-
DNA damage and somatic mutations in mammalian cells after irradiation with a nail polish dryer
Nature Communications (2023)
-
A tumor focused approach to resolving the etiology of DNA mismatch repair deficient tumors classified as suspected Lynch syndrome
Journal of Translational Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.