Abstract
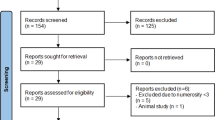
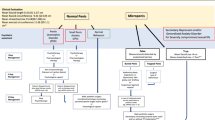
Male infertility currently contributes to nearly half of the reported infertility cases. Scrotal wall layers play a cardinal role in regulating testicular physiology. However, few studies have focused on the functional histology of these layers and their relations with infertility in humans. The objective of the present narrative review is to collate novel insights into the functional histology of the human scrotal wall layers and their relation with infertility. The data was extracted from articles published between 1946 and 2021. The study was performed between January and December 2021. 71 original studies have been included in this review. Despite the fact that few studies have presented detailed functional histology of the human scrotal wall layers, this narrative review elucidates the possible influence of scrotal histology on infertility. Scrotal wall layers-associated pathologies may induce infertility by various mechanisms. They can impose mechanical forces that may affect the testicular histology and stimulate testicular inflammation. Moreover, they may induce testicular hyperthermia. Various unanswered clinical questions have been identified in this narrative review. More clinical studies are needed to assess the effect of alterations in the components of the scrotal wall layers on fertility (e.g., due to the exposure to metabolic and/or psychological stressors). In addition, testing the effectiveness of various pharmacological/surgical interventions to treat scrotal wall layers-associated pathologies will provide more insights into infertility treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
No new datasets were generated or analyzed for this narrative review.
References
Fietz D, Bergmann M. Functional Anatomy and Histology of the Testis. In: Simoni M, Huhtaniemi I. editors. Endocrinology of the Testis and Male Reproduction. Endocrinology. Springer, Cham. 2017. https://doi.org/10.1007/978-3-319-44441-3_9.
Durairajanayagam D, Agarwal A, Ong C. Causes, effects and molecular mechanisms of testicular heat stress. Reprod Biomed Online. 2015;30:14–27. https://doi.org/10.1016/j.rbmo.2014.09.018.
Erkkilä K, Henriksén K, Hirvonen V, Rannikko S, Salo J, Parvinen M, et al. Testosterone regulates apoptosis in adult human seminiferous tubules in vitro. J Clin Endocrinol Metab. 1997;82:2314–21.
Schmid N, Flenkenthaler F, Stöckl JB, Dietrich KG, Köhn FM, Schwarzer JU, et al. Insights into replicative senescence of human testicular peritubular cells. Sci Rep. 2019;9:1–14.
Holmes SD, Lipshultz LI, Smith RG. Regulation of transferrin secretion by human sertoli cells cultured in the presence or absence of human peritubular cells. J Clin Endocrinol Metab. 1984;59:1058–62.
Middendorff R, Müller D, Mewe M, Mukhopadhyay AK, Holstein AF, Davidoff MS. The tunica albuginea of the human testis is characterized by complex contraction and relaxation activities regulated by cyclic GMP. J Clin Endocrinol Metab. 2002;87:3486–99.
Patel AP. Anatomy and physiology of chronic scrotal pain. Transl Androl Urol. 2017;6:S51–6.
Ivell R. Lifestyle impact and the biology of the human scrotum. Reprod Biol Endocrinol. 2007;5:1–8.
Carlsen E, Andersson AM, Petersen JH, Skakkebæk NE. History of febrile illness and variation in semen quality. Hum Reprod. 2003;18:2089–92.
Garolla A, Torino M, Sartini B, Cosci I, Patassini C, Carraro U, et al. Seminal and molecular evidence that sauna exposure affects human spermatogenesis. Hum Reprod. 2013;28:877–85.
Tanaka T, Kobori Y, Terai K, Inoue Y, Osaka A, Yoshikawa N, et al. Seminal oxidation–reduction potential and sperm DNA fragmentation index increase among infertile men with varicocele. Hum Fertil. 2022;25:142–6. https://doi.org/10.1080/14647273.2020.1712747
Légaré C, Thabet M, Sullivan R. Expression of heat shock protein 70 in normal and cryptorchid human excurrent duct. Mol Hum Reprod. 2004;10:197–202.
Abdelhamid MHM, Walschaerts M, Ahmad G, Mieusset R, Bujan L, Hamdi S. Mild experimental increase in testis and epididymis temperature in men: Effects on sperm morphology according to spermatogenesis stages. Transl Androl Urol. 2019;8:651–65.
Zhang MH, Zhai LP, Fang ZY, Li AN, Xiao W, Qiu Y. Effect of scrotal heating on sperm quality, seminal biochemical substances, and reproductive hormones in human fertile men. J Cell Biochem. 2018;119:10228–38.
Zumstein V, Vetterlein MW, Hoffer AP, Schmid HP, Engeler D, Betschart P. Stay cool! Special underwear for cyclic cooling significantly decreases scrotal skin temperature. Cent Eur J Urol. 2021;74:468–70.
Benidir T, Remondini T, Lau S, Jarvi KA. Evaluation of patient compliance with the use of scrotal cooling devices. F S Reports. 2021;2:289–95. https://doi.org/10.1016/j.xfre.2021.06.007
Sengul G, Ertekin C. Human cremaster muscle and cremasteric reflex: A comprehensive review. Clin Neurophysiol. 2020;131:1354–64. https://doi.org/10.1016/j.clinph.2020.03.011.
Smith JG, Fischer RW, Blank H. The epidermal barrier: a comparison between scrotal and abdominal skin. J Invest Dermatol. 1960;36:337–43. https://doi.org/10.1038/jid.1961.55.
Jurkiewicz NH, Jurkiewicz A, da Silva Júnior ED. Physiopharmacological properties of the testicular capsule: A concise review. Eur J Pharmacol. 2020;883:173345. https://doi.org/10.1016/j.ejphar.2020.173345.
Arenas MI, Bethencourt FR, Fraile B, Paniagua R. Immunocytochemical and quantitative study of the tunica albuginea testis in young and ageing men. Histochem Cell Biol. 1997;107:469–77. https://doi.org/10.1007/s004180050134.
Rikimaru A, Maruyama T, Shirai M, Dendo I. Pressure recording of contraction of the dog testis. Tohoku J Exp Med. 1972;108:305–6. https://doi.org/10.1620/tjem.108.305.
Qin DN, Lung MA. Effect of testicular capsulotomy on secretion of testosterone and gonadotrophins in rats. Asian J Androl. 2000;2:257–61.
Qin DN, Lung MA. Effect of testicular capsulotomy on fertility of rats. Asian J Androl. 2001;3:21–5.
Banks FCL, Knight GE, Calvert RC, Turmaine M, Thompson CS, Mikhailidis DP, et al. Smooth muscle and purinergic contraction of the human, rabbit. Rat, Mouse Testicular Capsul 1. 2006;480:473–80.
Isaza-Restrepo A, Martin-Saavedra JS, Velez-Leal JL, Vargas-Barato F, Riveros-Dueñas R. The Peritoneum: Beyond the Tissue - A Review. Front Physiol. 2018;9:738. https://doi.org/10.3389/fphys.2018.00738.
Liu L. Applied anatomy of the scrotum and its contents. In Scrotoscopic Surgery. Academic Press; 2019. pp. 1–8.
Çayan S, Orhan İ, Altay B, Aşcı R, Akbay E, Ayas B, et al. Fertility outcomes and predictors for successful sperm retrieval and pregnancy in 327 azoospermic men with a history of cryptorchidism who underwent microdissection testicular sperm extraction. Andrology. 2021;9:253–9. https://doi.org/10.1111/andr.12910.
Hattori M, Tonooka A, Zaitsu M, Mikami K, Suzue-Yanagisawa A, Uekusa T, et al. Overexpression of aquaporin 1 in the tunica vaginalis may contribute to adult-onset primary hydrocele testis. Adv Urol. 2014;2014:202434. https://doi.org/10.1155/2014/202434.
Dandapat MC, Padhi NC, Patra AP. Effect of hydrocele on testis and spermatogenesis. Br J Surg. 1990;77:1293–4. https://doi.org/10.1002/bjs.1800771132.
Stula I, Družijanić N, Sršen D, Capkun V, Perko Z, Sapunar A, et al. Influence of inguinal hernia mesh repair on testicular flow and sperm autoimmunity. Hernia. 2012;16:417–24. https://doi.org/10.1007/s10029-012-0918-1.
Shin D, Lipshultz LI, Goldstein M, Barmé GA, Fuchs EF, Nagler HM, et al. Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermia. Ann Surg. 2005;241:553–8. https://doi.org/10.1097/01.sla.0000157318.13975.2a.
Fallatah M, Aljuhaiman A, Alali H, Ahmed S, Alhathal N. Urology case reports infertility secondary to an infected hydrocele: a case report. Urol Case Rep. 2020;28:101071. https://doi.org/10.1016/j.eucr.2019.101071
Abdel Aal H, el Atribi A, Abdel Hafiz A, Aidaros M. Azoospermia in bilharziasis and the presence of sperm antibodies. J Reprod Fertil. 1975;42:403–6. https://doi.org/10.1530/jrf.0.0420403.
Abdel-Naser MB, Wollina U, Lohan M, Zouboulis CC, Altenburg A. Schistosomiasis (Bilharziasis) ova: An incidental finding in testicular tissue of an obstructive azoospermic man. Andrologia. 2018;50:e13131. https://doi.org/10.1111/and.13131.
Chandra RV, Dowling RJ, Ulubasoglu M, Haxhimolla H, Costello AJ. Rational approach to diagnosis and management of blunt scrotal trauma. Urology. 2007;70:230–4. https://doi.org/10.1016/j.urology.2007.03.064.
Decoste RC, Carter MD, Merrimen J. Paratesticular fibrous pseudotumour: Intraoperative frozen section analysis can help prevent unnecessary orchiectomy. J Can Urol Assoc. 2015;9:E731–3.
Zhang Z, Yang J, Li M, Cai W, Liu Q, Wang T, et al. Paratesticular fibrous pseudotumor: a report of five cases and literature review. Front Med. 2014;8:484–8.
Ammar T, Sidhu PS, Wilkins CJ. Male infertility: the role of imaging in diagnosis and management. Br J Radiol. 2012;85:S59–68. https://doi.org/10.1259/bjr/31818161.
Xu C, Liu M, Zhang F, Liu J, Jiang X, Teng J, et al. The association between testicular microlithiasis and semen parameters in Chinese adult men with fertility intention: experience of 226 cases. Urology. 2014;84:815–20. https://doi.org/10.1016/j.urology.2014.03.021
Thomas K, Wood SJ, Thompson AJ, Pilling D, Lewis-Jones DI. The incidence and significance of testicular microlithiasis in a subfertile population. Br J Radiol. 2000;73:494–7. https://doi.org/10.1259/bjr.73.869.10884745.
Koch T, Hansen AH, Priskorn L, Petersen JH, Carlsen E, Main KM, et al. A history of cryptorchidism is associated with impaired testicular function in early adulthood: A cross-sectional study of 6376 men from the general population. Hum Reprod. 2020;35:1765–80.
Mieusset R, Bujan L, Massat G, Mansat A, Pontonnier F. Andrology: Clinical and biological characteristics of infertile men with a history of cryptorchidism. Hum Reprod. 1995;10:613–9.
Turgut AT, Ünsal A, Özden E, Kosar P, Kosar U, Emir L. Unilateral idiopathic hydrocele has a substantial effect on the ipsilateral testicular geometry and resistivity indices. J Ultrasound Med. 2006;25:837–43.
Kukadia AN, Ercole CJ, Gleich P, Hensleigh H, Pryor JL. Testicular trauma: Potential impact on reproductive function. J Urol. 1996;156:1643–6.
Kordzadeh A, Liu MO, Jayanthi NV. Male infertility following inguinal hernia repair: a systematic review and pooled analysis. Hernia. 2017;21:1–7. https://doi.org/10.1007/s10029-016-1560-0.
Bouchot O, Branchereau J, Perrouin-Verbe MA. Influence of inguinal hernia repair on male fertility. J Visc Surg. 2018;155:S37–40. https://doi.org/10.1016/j.jviscsurg.2018.04.008.
Dangi A, Gupta S, Tamaknand V, Godara R, Garg P. Persistent mullerian duct syndrome presenting as an inguinal. Hernia: a Case Report Int J Surg Med. 2017;3:1.
Hassan A, El-Mogy S, Zalata K, Mostafa T. Testicular schistosomiasis: A case study. Fertil Steril. 2011;95:2124.e1–e4. https://doi.org/10.1016/j.fertnstert.2010.12.050.
Adisa J, Egbujo EM, Yahaya BA, Echejoh G. Primary infertility associated with schitosoma mansoni: A case report from the Jos Plateau, north central Nigeria. Afr Health Sci. 2012;12:563–5.
Lopes RI, Leite KR, Prando D, Lopes RN. Testicular schistosomiasis caused by schistosoma mansoni: A case report from Brazil. Brazilian. J Infect Dis. 2007;11:523–4.
Alahmar AT, Sengupta P, Dutta S, Calogero AE. Coenzyme Q10, oxidative stress markers, and sperm DNA damage in men with idiopathic oligoasthenoteratospermia. Clin Exp Reprod Med. 2021;48:150–5.
Darbandi M, Darbandi S, Agarwal A, Baskaran S, Dutta S, Sengupta P, et al. Reactive oxygen species-induced alterations in H19-Igf2 methylation patterns, seminal plasma metabolites, and semen quality. J Assist Reprod Genet. 2019;36:241–53.
Conzi R, Damasio MB, Bertolotto M, Secil M, Ramanathan S, Rocher L, et al. Sonography of scrotal wall lesions and correlation with other modalities. J Ultrasound Med. 2017;36:2149–63.
Jurewicz M, Gilbert BR. Imaging and angiography in male factor infertility. Fertil Steril. 2016;105:1432–42. https://doi.org/10.1016/j.fertnstert.2016.04.009.
Belva F, Bonduelle M, Roelants M, Michielsen D, Van Steirteghem A, Verheyen G, et al. Semen quality of young adult ICSI offspring: The first results. Hum Reprod. 2016;31:2811–20.
Kayalioglu G, Altay B, Uyaroglu FG, Bademkiran F, Uludag B, Ertekin C. Morphology and innervation of the human cremaster muscle in relation to its function. Anat Rec. 2008;291:790–6.
Aglianò M, Lorenzoni P, Franci D, Messina M, Guarna M, Molinaro F, et al. Immunohistochemical detection of myosin heavy chain isoforms in human cremaster muscle. Ital J Anat Embryol. 2015;120:149.
Tanji N, Tanji K, Hiruma S, Hashimoto S, Yokoyama M. Histochemical study of human cremaster in varicocele patients. Arch Androl. 2000;45:197–202.
Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, et al. Transcriptional co-activator PGC-1 alpha drives the formation of slow-twitch muscle fibres. Nature. 2002;418:797–801. https://doi.org/10.1038/nature00904.
Naldaiz-Gastesi N, Goicoechea M, Aragón IM, Pérez-López V, Fuertes-Alvarez S, Herrera-Imbroda B, et al. Isolation and characterization of myogenic precursor cells from human cremaster muscle. Sci Rep. 2019;9:1–15.
Yang Y, Wu X, Leng Q, Su W, Wang S, Xing R, et al. Microstructures of the spermatic cord with three-dimensional reconstruction of sections of the cord and application to varicocele. Syst Biol Reprod Med. 2020;66:216–22. https://doi.org/10.1080/19396368.2020.1741723.
Schwarz GM, Hirtler L. The cremasteric reflex and its muscle – a paragon of ongoing scientific discussion: A systematic review. Clin Anat. 2017;30:498–507.
Sigalos JT, Pastuszak AW. Chronic orchialgia: Epidemiology, diagnosis and evaluation. Transl Androl Urol. 2017;6:S37–43.
Kavoussi PK. Microsurgical subinguinal cremaster muscle release for chronic orchialgia secondary to hyperactive cremaster muscle reflex in adults. Andrologia. 2020;52:1–3.
Favorito LA, Anderson KM, Costa SF, Costa WS, Sampaio FJ. Structural study of the cremaster muscle in patients with retractile testis. J Pediatr Surg. 2018;53:780–3. https://doi.org/10.1016/j.jpedsurg.2017.04.013.
Howe AS, Vasudevan V, Kongnyuy M, Rychik K, Thomas LA, Matuskova M, et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol. 2017;6:1159–66.
Jacobsen FM, Rudlang TM, Fode M, Østergren PB, Sønksen J, Ohl DA, et al. The impact of testicular torsion on testicular function. World J Mens Health. 2019;37:298–307.
Yilmaz U, Yang CC, Berger RE. Dartos reflex: A sympathetically mediated scrotal reflex. Muscle Nerve. 2006;33:363–8.
Holstein AF, Orlandini GE, Baumgarten HG. Morphological analysis of tissue components in the tunica dartos of man. Cell Tissue Res. 1974;154:329–44.
Soler JM, Previnaire JG, Amarenco G. Dartos reflex as autonomic assessment in persons with spinal cord injury. Spinal Cord Ser Cases. 2017;3:17097. https://doi.org/10.1038/s41394-017-0024-9
Shafik A. Abscent Dartos [Internet]. 1978. p. 354. https://doi.org/10.1111/j.1464-410x.1978.tb03649.x.
Shafik A, Olfat S. Aligamentous testicle New clinicopathologic entity in genesis of male infertility and its treatment by orchiopexy. Urology. 1979;13:54–7.
Cairo AF, Shafik H. Anatomy and function of scrotal ligament. Urology. 1977;9:651–5.
Ganapathy A, Jayaraman Pushpaja J, Kapoor K, Sharma MK, Singh S, Jhajhria SK. Structural and functional significance of scrotal ligament: a comparative histological study. Anat Sci Int. 2021;96:106–11. https://doi.org/10.1007/s12565-020-00566-8
Cavalie G, Bellier A, Marnas G, Boisson B, Robert Y, Rabattu PY, et al. Anatomy and histology of the scrotal ligament in adults: inconsistency and variability of the gubernaculum testis. Surg Radio Anat. 2018;40:365–70.
Cho I-C, Kim SK, Choi KB, Min SK, Bae JY, Ko JS. Idiopathic calcinosis cutis of the scrotum: a case report. Korean J Urol Oncol. 2017;15:88–91.
Al-Dawsari NA, Raslan W, Dawamneh MF. Pigmented Bowen’s disease of the penis and scrotum in a patient with AIDS. Dermatol Online J. 2014;20:22337.
LACOUR JP, DUBOIS D, PISANI A, ORTONNE JP. Anatomical mapping of Merkel cells in normal human adult epidermis. Br J Dermatol. 1991;125:535–42.
BERMAN B, CHEN VL, FRANCE DS, DOTZ WI, PETRONI G. Anatomical mapping of epidermal Langerhans cell densities in adults. Br J Dermatol. 1983;109:553–8.
Boissy RE. The melanocyte. Its structure, function, and subpopulations in skin, eyes, and hair. Dermatol Clin. 1988;6:161–73.
Nishio H, Mizuno K, Moritoki Y, Kamisawa H, Naiki T, Kurokawa S, et al. Hemiscrotal agenesis: Pathogenesis and management strategies. Int J Urol. 2016;23:523–6.
Vignot L, Saad E, Peyromaure M, Barry Delongchamps N. Giant primary scrotal lipoma: a rare entity with diagnostic pitfalls. Case Rep Urol. 2020;2020:1–3.
Shafik A, Olfat S. Scrotal lipomatosis. Br J Urol. 1981;53:50–4. https://doi.org/10.1111/j.1464-410x.1981.tb03128.x.
Köckerling F, Schug-Pass C. Spermatic cord lipoma—a review of the literature. Front Surg. 2020;7:1–9.
Prabakaran S, Kumanov P, Tomova A, Hubaveshki S, Agarwal A. Adolescent varicocele: Association with somatometric parameters. Urol Int. 2006;77:114–7.
Ergün S, Bruns T, Soyka A, Tauber R. Angioarchitecture of the human spermatic cord. Cell Tissue Res. 1997;288:391–8.
Pieri S, Agresti P, Fiocca G, Regine G. Phlebographic classification of anatomic variants in the right internal spermatic vein confluence. Radio Med. 2006;111:551–61.
Nguyen TT, Trieu TS, Tran TO, Luong TLA. Evaluation of sperm DNA fragmentation index, Zinc concentration and seminal parameters from infertile men with varicocele. Andrologia. 2019;51:1–7.
Pfeifer S, Butts S, Catherino W, Davis O, Dumesic D, Fossum G, et al. Report on varicocele and infertility: A committee opinion. Fertil Steril. 2014;102:1556–60. https://doi.org/10.1016/j.fertnstert.2014.10.007.
Persad E, O’Loughlin CA, Kaur S, Wagner G, Matyas N, Hassler-Di Fratta MR, et al. Surgical or radiological treatment for varicoceles in subfertile men. Cochrane Database Syst Rev. 2021;4:CD000479. https://doi.org/10.1002/14651858.CD000479.pub6.
Bolat D, Gunlusoy B, Yarimoglu S, Ozsinan F, Solmaz S, Imamoglu FG. Isolated thrombosis of right spermatic vein with underlying Factor v Leiden mutation. Can Urol Assoc J. 2016;10:E324–7.
Bakshi S. Correction to: Bilateral spontaneous thrombosis of the pampiniform plexus mimicking incarcerated inguinal hernia: case report of a rare condition and literature review. Surg Case Rep. 2020;6:56. https://doi.org/10.1186/s40792-020-00821-0.
Skoglund RW, McRoberts JW, Ragde H. Torsion of the spermatic cord: a review of the literature and an analysis of 70 new cases. J Urol. 1970;104:604–7. https://doi.org/10.1016/S0022-5347(17)61792-0.
Acknowledgements
We would like to acknowledge Judy Tanios for the critical review of the manuscript. We would like to acknowledge Ramy Salemeh and Marwa Bazzi for their help to generate the figures.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design: GR, VM, M-JK, RI, and NM; Drafting the manuscript: GR, VM, MS, M-JK, RI, and NM. Revising manuscript critically for important intellectual content: All authors. Final approval of the manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Raad, G., Massaad, V., Serdarogullari, M. et al. Functional histology of human scrotal wall layers and their overlooked relation with infertility: a narrative review. Int J Impot Res 35, 428–438 (2023). https://doi.org/10.1038/s41443-022-00573-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00573-5