Abstract
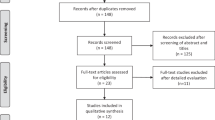
Despite the high prevalence of erectile dysfunction, patients are reluctant to seek medical advice, which leads to low diagnostic rates in clinical practice. Artificial intelligence has been widely applied in the diagnosis of many diseases and may alleviate the situation. However, the applications of artificial intelligence in erectile dysfunction have not been reviewed to date. Therefore, the assistance from artificial intelligence needs to be summarized. In this review, 418 publications before January 10, 2021, regarding artificial intelligence applications in diagnosing and predicting erectile dysfunction, were retrieved from five databases, including PubMed, EMBASE, the Cochrane Library, and two Chinese databases (WANFANG and CNKI). In addition, the reference lists of the included studies or relevant reviews were checked to avoid bias. Finally, 30 articles were reviewed to summarize the current status, merits, and limitations of applying artificial intelligence in diagnosing and predicting erectile dysfunction. The results showed that artificial intelligence contributed to developing novel diagnostic questionnaires, equipment, expert systems, classifiers by images and predictive models. However, most of the included studies were not subjected to external validations, resulting in doubt on the generalizability. In the future, more rigorously designed studies with high-quality datasets for erectile dysfunction are required.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Moor J. The Dartmouth college artificial intelligence conference: the next fifty years. AI Mag. 2006;27:87–91.
Oh JH, Kerns S, Ostrer H, Powell SN, Rosenstein B, Deasy JO. Computational methods using genome-wide association studies to predict radiotherapy complications and to identify correlative molecular processes. Sci Rep. 2017;7:43381.
Chen J, Chen Y, Chen G, Dai Y, Yao Z, Lu Q. Altered brain networks in psychogenic erectile dysfunction: a resting-state fMRI study. Andrology. 2017;5:1073–81.
Chen YF, Lin CS, Hong CF, Lee DJ, Sun C, Lin HH. Design of a clinical decision support system for predicting erectile dysfunction in men using NHIRD dataset. IEEE J Biomed Health Inf. 2019;23:2127–37.
Kamnitsas K, Ledig C, Newcombe VFJ, Simpson JP, Kane AD, Menon DK, et al. Efficient multi-scale 3D CNN with fully connected CRF for accurate brain lesion segmentation. Med Image Anal. 2017;36:61–78.
Kräter M, Abuhattum S, Soteriou D, Jacobi A, Krüger T, Guck J, et al. AIDeveloper: deep learning image classification in life science and beyond. Adv Sci. 2021;8:e2003743.
Zhang CW, Zhang Q, Gao XB, Liu P, Guo HQ. High accuracy and effectiveness with deep neural networks and artificial intelligence in pathological diagnosis of prostate cancer: initial results. J Urol. 2018;199:E935.
Saeed K, Rahkama V, Eldfors S, Bychkov D, Mpindi JP, Yadav B, et al. Comprehensive drug testing of patient-derived conditionally reprogrammed cells from castration-resistant prostate cancer. Eur Urol. 2017;71:319–27.
Hung AJ, Chen J, Gill IS. Automated performance metrics and machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surg. 2018;153:770–1.
Zheng H, Ji J, Zhao L, Chen M, Shi A, Pan L, et al. Prediction and diagnosis of renal cell carcinoma using nuclear magnetic resonance-based serum metabolomics and self-organizing maps. Oncotarget. 2016;7:59189–98.
Alonso-Silverio GA, Pérez-Escamirosa F, Bruno-Sanchez R, Ortiz-Simon JL, Muñoz-Guerrero R, Minor-Martinez A, et al. Development of a laparoscopic box trainer based on open source hardware and artificial intelligence for objective assessment of surgical psychomotor skills. Surg Innov. 2018;25:380–8.
Li L, Fan W, Li J, Li Q, Wang J, Fan Y, et al. Abnormal brain structure as a potential biomarker for venous erectile dysfunction: evidence from multimodal MRI and machine learning. Eur Radio. 2018;28:3789–800.
NIH Consensus Development Panel on Impotence. NIH consensus conference: impotence. JAMA. 1993;270:83–90.
Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007;120:151–7.
Ayta IA, Mckinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–6.
Lin H, Zhao L, Wu H, Cao M, Jiang H. Sexual life and medication taking behaviours in young men: an online survey of 92620 respondents in China. Int J Clin Pr. 2020;74:e13417.
Jang I, Lee JU, Lee JM, Kim BH, Moon B, Hong J, et al. LC-MS/MS software for screening unknown erectile dysfunction drugs and analogues: artificial neural network classification, peak-count scoring, simple similarity search, and hybrid similarity search algorithms. Anal Chem. 2019;91:9119–28.
Zhang Y, Tian X, Xia K, Zhuang J, Feng X, Zhou M, et al. Construction of intelligent expert system and its preliminary clinical application in the real world of diagnosis of sexual dysfunction. J Clin Urol. 2018;33:603–6.
Alemozaffar M, Regan MM, Cooperberg MR, Wei JT, Michalski JM, Sandler HM, et al. Prediction of erectile function following treatment for prostate cancer. JAMA. 2011;306:1205–14.
Clark HD, Wells GA, Huët C, Mcalister FA, Salmi LR, Fergusson D, et al. Assessing the quality of randomized trials: Reliability of the jadad scale. Control Clin Trials. 1999;20:448–52.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of case-control studies in meta-analyses. Eur J Epidemiol. 2011;25:603–5.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. Grade: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Montorsi F, Oelke M, Henneges C, Brock G, Salonia A, D’anzeo G, et al. Exploratory decision-tree modeling of data from the randomized REACTT trial of tadalafil versus placebo to predict recovery of erectile function after bilateral nerve-sparing radical prostatectomy. Eur Urol. 2016;70:529–37.
Bi Q, Goodman KE, Kaminsky J, Lessler J. What is machine learning? A primer for the epidemiologist. Am J Epidemiol. 2019;188:2222–39.
Jordan MI, Mitchell TM. Machine learning: trends, perspectives, and prospects. Science. 2015;349:255–60.
Macyszyn L, Akbari H, Pisapia JM, Da X, Attiah M, Pigrish V, et al. Imaging patterns predict patient survival and molecular subtype in glioblastoma via machine learning techniques. Neuro Oncol. 2016;18:417–25.
Xiong Y, Zhang YC, Zhang FX, Wu CJ, Huang XYZ, Qin F, et al. Risks and subgroups of cognitive impairment under different marital status among older adults: a latent profile analysis. J Mens Health. 2021;17:234–42.
Hossain MA, Saiful Islam SM, Quinn JMW, Huq F, Moni MA. Machine learning and bioinformatics models to identify gene expression patterns of ovarian cancer associated with disease progression and mortality. J Biomed Inf. 2019;100:103313.
Mahmud M, Kaiser MS, Hussain A, Vassanelli S. Applications of deep learning and reinforcement learning to biological data. IEEE Trans Neural Netw Learn Syst. 2018;29:2063–79.
Binik YM, Servan-Schreiber D, Freiwald S, Hall KS. Intelligent computer-based assessment and psychotherapy. An expert system for sexual dysfunction. J Nerv Ment Dis. 1988;176:387–400.
Selby LV, Narain WR, Russo A, Strong VE, Stetson P. Autonomous detection, grading, and reporting of postoperative complications using natural language processing. Surgery. 2018;164:1300–5.
Aramaki E, Miyabe M, Honda C, Isozaki S, Wakamiya S, Sato A, et al. KOTOBAKARI study: using natural language processing of patient short narratives to detect cancer related cognitive impairment. Stud Health Technol Inf. 2019;264:1111–5.
Jannini EA, Granata AM, Hatzimouratidis K, Goldstein I. Use and abuse of Rigiscan in the diagnosis of erectile dysfunction. J Sex Med. 2009;6:1820–9.
Van Kollenburg RAA, De Bruin. DM. Validation of the electronic version of the international index of erectile function (IIEF-5 and IIEF-15): a crossover study. J Med Internet Res. 2019;21:e13490.
Glavaš S, Valenčić L, Trbojević N, Tomašić AM, Turčić N, Tibauth S, et al. Erectile function in cardiovascular patients: its significance and a quick assessment using a visual-scale questionnaire. Acta Cardiol. 2015;70:712–9.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the international index of erectile function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Wagner G, Gerstenberg T, Levin RJ. Electrical activity of corpus cavernosum during flaccidity and erection of the human penis: a new diagnostic method? J Urol. 1989;142:723–5.
Krafft ME, Boñaga L. Computergestützte Auswertung des glattmuskulären Elektromyogramms der Corpora cavernosa (CC-EMG) mittels Fast-Fourier-Transformation (FFT). Aktuelle Urologie. 1996;27:291–8.
Stief CG, Kellner B, Hartung C, Hauck E, Schlote N, Truss M, et al. Computer-assisted evaluation of the smooth-muscle electromyogram of the corpora cavernosa by fast Fourier transformation. Eur Urol. 1997;31:329–34.
Gorek M, Stief CG, Hartung C, Jonas U. Computer-assisted interpretation of electromyograms of corpora cavernosa using fuzzy logic. World J Urol. 1997;15:65–70.
Kellner B, Stief CG, Hinrichs H, Hartung C. Computerized classification of corpus cavernosum electromyogram signals by the use of discriminant analysis and artificial neural networks to support diagnosis of erectile dysfunction. Urol Res. 2000;28:6–13.
El-Sakka AI. Association between International Index of Erectile Function and axial penile rigidity in patients with erectile dysfunction. Int J Impot Res. 2003;15:426–9.
Ng WK, Ng EY, Chia SJ. The engineering analysis of bioheat equation and penile hemodynamic relationships in the diagnosis of erectile dysfunction: part I-theoretical study and mathematical modeling. Int J Impot Res. 2008;20:295–306.
Ng WK, Ng YK, Tan YK. Qualitative study of sexual functioning in couples with erectile dysfunction: prospective evaluation of the thermography diagnostic system. J Reprod Med. 2009;54:698–705.
Ng EY, Ng WK, Huang J, Tan YK. The engineering analysis of bioheat equation and penile hemodynamic relationships in the diagnosis of erectile dysfunction: part II-model optimization using the ANOVA and Taguchi method. Int J Impot Res. 2008;20:285–94.
Udelson D, Nehra A, Hatzichristou DG, Azadzoi K, Moreland RB, Krane J, et al. Engineering analysis of penile hemodynamic and structural-dynamic relationships: Part I–Clinical implications of penile tissue mechanical properties. Int J Impot Res. 1998;10:15–24.
Udelson D, Nehra A, Hatzichristou DG, Azadzoi K, Moreland RB, Krane RJ, et al. Engineering analysis of penile hemodynamic and structural-dynamic relationships: part III–Clinical considerations of penile hemodynamic and rigidity erectile responses. Int J Impot Res. 1998;10:89–99.
Udelson D, Park K, Sadeghi-Nejad H, Salimpour P, Krane RJ, Goldstein I. Axial penile buckling forces vs Rigiscan radial rigidity as a function of intracavernosal pressure: why Rigiscan does not predict functional erections in individual patients. Int J Impot Res. 1999;11:327–37.
Yuan J, Qin F. Intelligent monitor of erectile function: US, 9888878. 2018.2.13. www.freepatentsonline.com/9888878.html
Cera N, Di Pierro ED, Ferretti A, Tartaro A, Romani GL, Perrucci MG. Brain networks during free viewing of complex erotic movie: new insights on psychogenic erectile dysfunction. PLoS ONE. 2014;9:e105336.
Elhanbly S, Elkholy A. Nocturnal penile erections: the role of RigiScan in the diagnosis of vascular erectile dysfunction. J Sex Med. 2012;9:3219–26.
Nakahara T, Narula J, Tijssen JGP, Agarwal S, Chowdhury MM, Coughlin PA. et al. (18)F-Fluoride positron emission tomographic imaging of penile arteries and erectile dysfunction. J Am Coll Cardiol. 2019;73:1386–94.
Haskins AE, Han PK, Lucas FL, Bristol I, Hansen M. Development of clinical models for predicting erectile function after localized prostate cancer treatment. Int J Urol. 2014;21:1227–33.
Rabbani F, Stapleton AM, Kattan MW, Wheeler TM, Scardino PT. Factors predicting recovery of erections after radical prostatectomy. J Urol. 2000;164:1929–34.
Kwon T, Lee C, Jung J, Kim CS. Neurovascular bundle size measured on 3.0-T magnetic resonance imaging is associated with the recovery of erectile function after robot-assisted radical prostatectomy. Urol Oncol. 2017;35:542.e511–42.e517.
Safavy S, Kilday PS, Slezak JM, Abdelsayed GA, Harrison TN, Jacobsen SJ, et al. Effect of a smoking cessation program on sexual function recovery following robotic prostatectomy at Kaiser Permanente Southern California. Perm J. 2017;21:16–138.
Hamidi N, Altinbas NK, Gokce MI, Suer E, Yagci C, Baltaci S, et al. Preliminary results of a new tool to evaluate cavernous body fibrosis following radical prostatectomy: penile elastography. Andrology. 2017;5:999–1006.
KleinJan GH, Sikorska K, Korne CM, Brouwer OR, Buckle T, Tillier C, et al. A prediction model relating the extent of intraoperative fascia preservation to erectile dysfunction after nerve-sparing robot-assisted radical prostatectomy. J Robot Surg. 2019;13:455–62.
Abdollah F, Sun M, Suardi N, Gallina A, Bianchi M, Tutolo M, et al. Prediction of functional outcomes after nerve-sparing radical prostatectomy: results of conditional survival analyses. Eur Urol. 2012;62:42–52.
Briganti A, Gallina A, Suardi N, Capitanio U, Tutolo M, Bianchi M, et al. Predicting erectile function recovery after bilateral nerve sparing radical prostatectomy: a proposal of a novel preoperative risk stratification. J Sex Med. 2010;7:2521–31.
Novara G, Ficarra V, D’Elia C, Secco S, De Gobbi A, Cavalleri S, et al. Preoperative criteria to select patients for bilateral nerve-sparing robotic-assisted radical prostatectomy. J Sex Med. 2010;7:839–45.
Cozzi G, Musi G, Monturano M, Bagnardi V, Frassoni S, Jereczek-Fossa BA, et al. Sexual function recovery after robot-assisted radical prostatectomy: outcomes from an Italian referral centre and predicting nomogram. Andrologia. 2019;51:e13385.
Mulhall JP, Kattan MW, Bennett NE, Stasi J, Nascimento B, Eastham J, et al. Development of nomograms to predict the recovery of erectile function following radical prostatectomy. J Sex Med. 2019;16:1796–802.
Huynh LM, Skarecky D, Wilson T, Lau C, Wagner C, Porter J, et al. Internal and external validation of a 90-day percentage erection fullness score model predicting potency recovery following robot-assisted radical prostatectomy. Eur Urol Oncol. 2020;3:657–62.
Huynh LM, Osann K, Skarecky D, Ahlering TE. Predictive modelling of 2-year potency outcomes using a novel 90-day erection fullness scale after robot-assisted radical prostatectomy. BJU Int. 2018;122:249–54.
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature. 2014;507:315–22.
Schymura MJ, Sun L, Percy-Laurry A. Prostate cancer collaborative stage data items–their definitions, quality, usage, and clinical implications: a review of SEER data for 2004-10. Cancer. 2014;120:3758–70.
Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30.
Barrett T, Troup DB, Wilhite SE, Ledoux P, Rudnev D, Evangelista C, et al. NCBI GEO: archive for high-throughput functional genomic data. Nucleic Acids Res. 2009;37:D885–90.
Funding
This work was supported by the Natural Science Foundation of China [grant numbers 81871147 and 81671453]; and the funding of Health Commission of Sichuan Province [grant numbers 20PJ184 and 20PJ063].
Author information
Authors and Affiliations
Contributions
Conception and design: YX, FQ, and JY. Administrative support: FQ and JY. Provision of study materials or patients: YX and FQ. Collection and assembly of data: YX, FQ, and YZ. Data analysis and interpretation: YX, YZ, FZ, and CW. Manuscript writing: all authors. Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xiong, Y., Zhang, Y., Zhang, F. et al. Applications of artificial intelligence in the diagnosis and prediction of erectile dysfunction: a narrative review. Int J Impot Res 35, 95–102 (2023). https://doi.org/10.1038/s41443-022-00528-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00528-w