Abstract
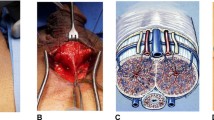
The penoscrotal (PS), infrapubic (IP), and subcoronal (SC) incisions are used for inserting an inflatable penile prosthesis (IPP). Each surgical approach has its advantages and disadvantages and experts continue to debate which technique has the best outcomes. We performed a critical review of the published English-language studies up to April 2020 investigating the PS, IP, or SC approach for IPP placement. The PS approach is the most frequently used incision. The available data do not suggest a difference between PS and IP approach in size of the implanted prostheses, achieved penile length, patient satisfaction, infection rate, and risk of urethral injury. The risk of dorsal nerve injury, even if low, seems to be greater for IP approach. IP technique is associated with shorter operative time and earlier use of IPP compared with PS approach. Despite limited available data it is reasonable to assume that SC approach, compared with other approaches, has longer operative time and similar infection rate. The time to device activation with SC technique could be similar to the IP approach, but there is only minimal data that can confirm this hypothesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Salonia A, Bettocchi C, Carvalho J, Corona G, Jones TH, Kadioglu A, et al. EAU guidelines on sexual and reproductive health. In: European Association of Urology Guidelines. EAU Guidelines Office, Arnhem, The Netherlands; 2020.
Wilson SK, Delk JR. Historical advances in penile prostheses. Int J Impot Res. 2000;12:S101–7.
Beheri G. Surgical treatment of impotence. Plast Reconstr Surg. 1966;38:92–7.
Scott F, Bradley WE, Timm GW. Management of erectile impotence use of implantable inflatable prosthesis. Urology. 1973;2:80–2.
Mobley DF. Early history of inflatable penile prosthesis surgery: a view from someone who was there. Asian J Androl. 2015;17:225–9.
Houlihan MD, Köhler TS, Wilson SK, Hatzichristodoulou G. Penoscrotal approach for IPP: still up-to-date after more than 40 years? Int J Impot Res. 2020;32:2–9.
Barrett D, Furlow W. Penile prosthesis implantation. In: Segraves R, Schoenberg H, editors. Diagnosis and treatment of erectile disturbances: a guide for clinicians. New York: Plenum Medical Book Co.; 1985. pp. 219–40.
Perito PE. Minimally invasive infrapubic inflatable penile implant. J Sex Med. 2008;5:27–30.
Palmisano F, Boeri L, Cristini C, Antonini G, Spinelli MG, Franco G, et al. Comparison of infrapubic vs penoscrotal approaches for 3-piece inflatable penile prosthesis placement: do we have a winner? Sex Med Rev. 2018;6:631–9.
Levine LA, Becher E, Bella A, Brant W, Kohler T, Martinez-Salamanca JI, et al. Penile prosthesis surgery: current recommendations from the International Consultation on Sexual Medicine. J Sex Med. 2016;13:489–518.
Egydio PH. Surgical straightening with tunical incision and grafting technique-single relaxing incision based on geometrical principles. In: Levine L, editor. Peyronie’s disease textbook: a guide to clinical management. Totowa; Hymana Press; 2006. p. 227–39.
Weinberg AC, Pagano MJ, Deibert CM, Valenzuela RJ. Sub-coronal inflatable penile prosthesis placement with modified no-touch technique: a step-by-step approach with outcomes. J Sex Med. 2016;13:270–6.
Park SH. Subcoronal inflatable penile prosthesis under local anesthesia. J Vis Surg. 2019;5:65.
Trost LW, Boonjindasup AG, Hellstrom WJG. Comparison of infrapubic versus transcrotal approaches for inflatable penile prosthesis placement: a multi-institution report. Int J Impot Res. 2015;27:86–9.
Sharma N, Berookhim B, Nelson C, Jenkins L, Mulhall J. 028 contemporary practice patterns for penile prosthesis implantation. J Sex Med. 2017;14:e13–4.
Montague DK, Angermeir KW. Surgical approaches for penile prosthesis implantation: penoscrotal vs infrapubic. Int J Impot Res. 2003;15:S134–5.
Shebl SE, Ali S. Infrapubic versus penoscrotal approaches for Implantation of semi-rigid penile prosthesis. Open J Urol. 2017;07:146–58.
Grande P, Antonini G, Cristini C, De Berardinis E, Gatto A, Di Lascio G, et al. Penoscrotal versus minimally invasive infrapubic approach for inflatable penile prosthesis placement: a single-center matched-pair analysis. World J Urol. 2018;36:1167–74.
Gupta NK, Ring J, Trost L, Wilson SK, Köhler TS. The penoscrotal surgical approach for inflatable penile prosthesis placement. Transl Androl Urol. 2017;6:628–38.
Jayadevan R, Eleswarapu SV, Mills JN. Infrapubic approach for placement of inflatable penile prosthesis: contemporary review of technique and implications. Int J Impot Res. 2020;32:10–7.
Wilson S, Henry G, Delk J. IPP & AUS through one incision. Int J Imp Res. 2002;2(Suppl 3):533.
Vollstedt A, Gross MS, Antonini G, Perito PE. The infrapubic surgical approach for inflatable penile prosthesis placement. Transl Androl Urol. 2017;6:620–7.
Park S, Wilson S, Morey A. Inflatable penile prosthesis implantation is possible under local anesthesia with conscious sedation: technique and results. J Sex Med. 2015;12:39–40.
Wilson SK, Mora-Estaves C, Egydio P, Ralph D, Habous M, Love C, et al. Glans necrosis following penile prosthesis implantation: prevention and treatment suggestions. Urology. 2017;107:144–8.
Karpman E, Bella A, Brant W, Christine B, Kansas B, Jones L, et al. Pd26-10 outcomes of ipp placement by surgical approach, penoscrotal vs infrapubic, results from a prospective multicenter study. J Urol. 2015;193:e569–70.
Antonini G, Busetto GM, De Berardinis E, Giovannone R, Vicini P, Del Giudice F, et al. Minimally invasive infrapubic inflatable penile prosthesis implant for erectile dysfunction: evaluation of efficacy, satisfaction profile and complications. Int J Impot Res. 2016;28:4–8.
Kramer A, Chason J. Residents at the university of maryland medical system provide insight to learning infrapubic approach for ipp surgery: relative benefits but novel challenges exposed in first 15 cases. J Sex Med. 2010;7:1298–305.
Candela J, Hellstrom W. Three-piece inflatable penile prosthesis implantation: a comparison of the penoscrotal and infrapubic surgical approaches. J La State Med Soc. 1996;148:296–301.
Eid JF. Penile implant: review of a “no-touch” technique. Sex Med Rev. 2016;4:294–300.
Carlos EC, Sexton SJ, Lentz AC. Urethral Injury and the Penile Prosthesis. Sex Med Rev. 2019;7:360–8.
Sexton SJ, Granieri MA, Lentz AC. Survey on the contemporary management of intraoperative urethral injuries during penile prosthesis implantation. J Sex Med. 2018;15:576–81.
Oberlin DT, Matulewicz RS, Bachrach L, Hofer MD, Brannigan RE, Flury SC. National practice patterns of treatment of erectile dysfunction with penile prosthesis implantation. J Urol. 2015;193:2040–4.
Bogoraz N. On complete plastic reconstruction of a penis sufficient for coitus [in Russian]. Sov Surg. 1936;8:303–9.
Lash H, Zimmerman D, Loeffler R. Silicone implantation: inlay method. Plast Reconstr Surg. 1964;34:75–80.
Pearman RO. Treatment of organic impotence by implantation of a penile prosthesis. J Urol. 1967;97:716–9.
Small M, Carrion H, Gordon J. Small-carrion penile prosthesis: new implant for management of impotence. Urology. 1975;5:479–86.
Barry JM, Seifert A. Penoscrotal approach for placement of paired penile implants for impotence. J Urol. 1979;122:325–6.
Jonas U, Jacobi GH. Silicone-silver penile prosthesis: description, operative approach and results. J Urol. 1980;123:865–7.
Smith AD. Circumcision incision for insertion of semirigid penile prosthesis. Urology. 1981;18:609.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SKW is consultant for AMT, Coloplast, International Medical Devices, and Lecturer for Boston Scientific. JRO is proctor and expert advisor for Coloplast, and proctor for Boston Scientific. CM has no conflict of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Otero, J.R., Manfredi, C. & Wilson, S.K. The good, the bad, and the ugly about surgical approaches for inflatable penile prosthesis implantation. Int J Impot Res 34, 128–137 (2022). https://doi.org/10.1038/s41443-020-0319-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-0319-4