Abstract
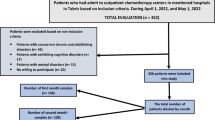
Sexual function is important for health and quality of life. We evaluated effects of lower urinary tract symptoms (LUTS), urinary incontinence (UI) and coital incontinence, and/or pelvic organ prolapse (POP) on sexual functions and quality of life of women over 50 years of age. Secondary objectives were to compare rate of sexual activity, effects of type of UI and coital incontinence on sexual functions and quality of life among age groups. Female-Sexual-Function-Index (FSFI), Pelvic-Organ-Prolapse/Urinary-Incontinence Sexual-Function-Questionnaire-12 (PISQ-12), and King’s-Health-Questionnaire (KHQ) were used for evaluation. Between 2013 and 2018, 1256 women were included. 565 women were 50–59 years (Group 1), 440 were 60–69 (Group 2), 251 were over 70 (Group-3). 763 women (60.7%) suffered from LUTS, 141 women (11.2%) suffered from POP only, and 352 women (28%) suffered from POP + LUTS. Younger women were more sexually active (p = 0.001). FSFI and PISQ-12 scores of women suffering from LUTS, POP + LUTS, and POP only were similar. Lubrication and orgasm scores were worse in Group 3 (p = 0.006 and 0.037). Type of UI did not affect FSFI and PISQ-12 scores. Coital incontinence was correlated with mixed UI in Groups 1 (p = 0.01) and 2 (p = 0.03). There was no association with coital incontinence and type of UI in Group 3. Coital incontinence had adverse effect in FSFI, PISQ-12 scores. In younger women, coital incontinence had an adverse effect on desire and arousal domains. KHQ scores were worse in women having LUTS in comparison to women suffering from POP only (p = 0.00) and were worse in Groups 1 and 2 (p = 0.002 and 0.013). KHQ scores were worse in women suffering from urge or mixed UI (p = 0.00). Coital incontinence had adverse effect in KHQ scores. In conclusion, aging, LUTS, UI, and coital incontinence have detrimental effects on sexual functions and quality of life. Urge or mixed UI have more adverse effects on quality of life. Quality of life is worse in younger women suffering from UI and coital incontinence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25:723–46.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardization subcommittee of the International Continence Society. Urology. 2003;61:37–49.
Salonia A, Zanni G, Briganti A, Deho F, Fabbri F, Colombo R, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur Urol. 2004;45:642–8.
Handa VL, Cundiff G, Chang HH, Helzsouer KJ. Female sexual function and pelvic floor disorders. Obstet Gynecol. 2008;111:1045–52.
Sarikaya S, Yildiz FG, Senocak C, Bozkurt OF, Karatas OF. Urinary incontinence as a cause of depression and sexual dysfunction: questionnaire-based study. Rev Int Androl 2018;pii: S1698-031X 30082-7. https://doi.org/10.1016/j.androl.2018.08.003.
Roos AM, Thakar R, Sultan AH, Burger CW, Paulus AT. Pelvic floor dysfunction: womens’ sexual concerns unraveled. J Sex Med. 2014;11:743–52.
Naeinian MR, Shaeiri MR, Hosseini FS. General health and quality of life in patients with sexual dysfunctions. Urol J. 2011;8:127–31.
Lee DM, Tetley J, Pendleton N. Urinary incontinence and sexual health in a population sample of older people. BJU Int. 2018;122:300–8.
Thomas HN, Hamm M, Hess R, Thurston RC. Changes in sexual function among midlife women: ‘I’m older… and I’m wiser’. Menopause. 2018;25:286–92.
Maher CF, Baessler KK, Barber MD, Cheon C, Consten ECJ, Cooper KG, et al. Summary: 2017 international consultation on incontinence evidence-based surgical pathway for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2018. https://doi.org/10.1097/SPV.0000000000000591.
Winkelman WD, Haviland MJ, Elkadry EA. Long-term pelvic symptoms, recurrence, satisfaction, and regret following colpocleisis. Female Pelvic Med Reconstr Surg. 2018. https://doi.org/10.1097/SPV.0000000000000602.
Thompson JC, Rogers RG. Surgical management of pelvic organ prolapse and its impact on sexual function. SexMed Rev. 2016;4:213–20.
Rogers RG, Pauls RN, Thakar R, Morin M, Kuhn A, Petri E, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the assessment of sexual health of women with female pelvic floor dysfunction. Neurourol Urodyn. 2018;37:1220–40.
El-Azab AS, Yousef HA, Seifeldein GS. Coital incontinence: relation to detrusor overactivity and stress incontinence. Neurourol Urodyn. 2011;30:520–4.
Caruso S, Brescia R, Matarazzo MG, Giunta G, Rapisarda AMC, Cianci A. Effects of urinary incontinence subtypes on women’s sexual function and quality of life. Urology. 2017;108:59–68.
Illiano E, Mahfouz W, Giannitsas K, Kocjancic E, Vittorio B, Athanasopoulos A. et al. Coital incontinence in women with urinary incontinence: an international study. J Sex Med. 2018; https://doi.org/10.1016/j.jsxm.2018.08.009.
Aslan G, Köseoğlu H, Sadik O, Gimen S, Cihan A, Esen A. Sexual function in women with urinary incontinence. Int J Impot Res. 2005;17:248–51.
Salonia A, Briganti A, Deho F, Zanni G, Rigatti P, Montorsi F. Women’s sexual dysfunction: a review of the ‘surgical landscape’. Eur Urol. 2006;50:44–52.
Moller LA, Lose G. Sexual activity and lower urinary tract symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2005;17:18–21.
Chu CM, Arya LA, Andy UU. Impact of urinary incontinence on female sexual health in women during midlife. Women’s Midlife Health. 2015;1:6.
Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecology Association (IUGA)/International Continence Society (ICS) joint report on the terminology for pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL. Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol. 2008;199:683.e1–683.e7.
Oksuz E, Malhan S. Kadin Cinsel Fonksiyon Indeksi: Turkce uyarlamasinin gecerlilik ve guvenilirlik analizi. Reliability and validity of the Female Sexual Function Index in a Turkish population. Syndrome. 2005;17:54–60.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208.
Cam C, Sancak P, Karahan N, Sancak A, Celik C, Karateke A. Validation of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12) in a Turkish population. Eur J Obstet Gynecol Reprod Biol. 2009;146:104–7.
Bilgic Celik D, Beji NK, Yalcin O. Turkish adaptation of the short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function questionnaire (PISQ-12): a validation and reliability study. Neurourol Urodyn. 2013;32:1068–73.
Rogers GR, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J. 2003;14:164–8.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. BJOG. 1997;104:1374–9.
Aslan E, Komurcu N, Beji NK, Yalcin O. Bladder training and Kegel exercises for women with urinary complaints living in a rest home. Gerontology. 2008;54:224–31.
Dalpiaz O, Kerschbaumer A, Mitterberger M, Pinggera GM, Colleselli D, Bartsch G, et al. Female sexual dysfunction: a new urogynecological research field. BJU Int. 2008;101:717–21.
Çayan S, Yaman Ö, Orhan I, Usta M, Başar M, Resim S, et al. Prevalence of sexual dysfunction and urinary incontinence and associated risk factors in Turkish women. Eur J Obstet Gynecol Reprod Biol. 2016;203:303–8.
Gozuyesil E, Gokyildiz Surucu S, Alan S. Sexual function and quality of life related problems during the menopausal period. H Health Psychol. 2018;23:1769–80.
Ambler DR, Bieber EJ, Diamond MP. Sexual function in elderly women: a review of current literature. Rev Obstet Gynecol. 2012;5:16–27.
Dombek K, Capistrano EJ, Costa AC, Marinheiro LP. Risk factors associated with sexual dysfunction in Brazilian postmenopausal women. Int J Impot Res. 2016;28:62–67.
Duralde ER, Rowen TS. Urinary incontinence and associated female sexual dysfunction. Sex Med Rev. 2017;5:470–85.
Handelzalts JE, Yakoobi T, Levy S, Peled Y, Wiznitzer A, Krissi H. The impact on genital self-image on sexual function in women with pelvic floor disorders. Eur J Obstet Gynecol Reprod Biol. 2017;211:164–8.
Fashokun TB, Harvie HS, Schimpf MO, Olivera CK, Epstein LB, Jean-Michel M, et al. Sexual activity and function in women with and without pelvic floor disorders. Int Urogynecol J. 2013;24:91–7.
Grzybowska ME, Wydra D. Predictors of sexual function in women with stress urinary incontinence. Neurourol Urodyn. 2018;37:861–8.
Felippe MR, Zambon JP, Girotti ME, Burti JS, Hacad JR, Cadamuro L, et al. What is the real impact of urinary incontinence on female sexual dysfunction? A case control study. Sex Med. 2017;5:e54–e60.
Dennerstein L, Guthrie JR, Hayes RD, DeRogatis LR, Lehert P. Sexual function, dysfunction, and sexual distress in a prospective, population-based sample of middle-aged Australian-born women. J Sex Med. 2008;5:2291–9.
Leiblum SR, Koochacki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive disorder in postmenopausal women: US Results from the Women’s International Study of Health and Sexuality (WISHeS). Menopause. 2006;13:46–56.
Juliato CRT, Melotti IGR, Santos LC Jr, Britto LGO, Riccetto CLZ. Does the severity of overactive bladder symptoms correlate with risk for female sexual dysfunction? J Sex Med. 2017;14:904–9.
Serati M, Salvatore S, Uccella S, Cromi A, Khullar V, Cardozo L, et al. Urinary incontinence at orgasm: relation to detrusor activity and treatment efficacy. Eur Urol. 2008;54:911–7.
Jha S, Strelley K, Radley S. Incontinence during intercourse: myths unravelled. Int Urogynecol J. 2012;23:633–7.
Gray T, Li W, Campbell P, Jha S, Radley S. Evaluation of coital incontinence by electronic questionnaire: prevalence, associations and outcomes in women attending a urogynecology clinic. Int Urogynecol J. 2018;29:969–78.
Grzybowska ME, Wydra DG. Coital incontinence: a factor for deteriorated health related quality of life and sexual function in women with urodynamic stress urinary incontinence. Int Urogynecol J. 2017;28:697–704.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ugurlucan, F.G., Evruke, I., Yasa, C. et al. Sexual functions and quality of life of women over 50 years with urinary incontinence, lower urinary tract symptoms and/or pelvic organ prolapse. Int J Impot Res 32, 535–543 (2020). https://doi.org/10.1038/s41443-019-0219-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0219-7
This article is cited by
-
Retrospective analysis of apical prolapse correction by unilateral pectineal suspension: perioperative and short-term results
International Urogynecology Journal (2023)