Abstract
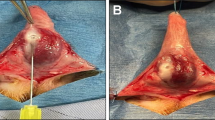
The cause of Peyronie’s disease (PD) is still not completely understood. The objective of this study, therefore, was to analyze the histological and biochemical alterations that occur after the instillation of blood in the tunica albuginea (TA) of rats with an emphasis on the remodeling process of ECM. Thirty male Wistar rats were divided into 4 groups: two control groups with instillation of distilled water in TA followed by penectomy after 15 days or 45 days, respectively and two experimental groups with instillation of blood in TA followed by penectomy after 15 days or 45 days, respectively. Histological, immunofluorescent and immunohistochemical analyses were performed. The higher presence of fibrotic tissue in rats injected with blood demonstrated alterations in TA similar to inflammation found in PD. The increased expression of TGF-β, MMP9, HPSE, and biglycan associated with the decreased expression of syndecan-1 and aggrecan in the experimental groups suggested an enhancement in the remodeling of ECM. The results contribute to show that blood instillation on TA appears to trigger alterations in the ECM similar to the ones found in inflammatory diseases such as PD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Sommer F, Schwarzer U, Wassmer G, Bloch W, Braun M, Klotz T, et al. Epidemiology of Peyronie’s disease. Int J Impot Res. 2002;14:379–83.
Gokce A, Abd Elmageed ZY, Lasker GF, Bouljihad M, Braun SE, Kim H, et al. Intratunical injection of genetically modified adipose tissue-derived stem cells with human interferon alpha-2b for treatment of erectile dysfunction in a rat model of tunica albugineal fibrosis. J Sex Med. 2015;12:1533–44.
Kwon KD, Choi MJ, Park JM, Song KM, Kwon MH, Batbold D, et al. Silencing histone deacetylase 2 using small hairpin RNA induces regression of fibrotic plaque in a rat model of Peyronie’s disease. BJU Int. 2014;114:926–36.
Gelbard MK, Dorey F, James K. The natural history of Peyronie’s disease. J Urol. 1990;144:1376–9.
Nelson CJ, Mulhall JP. Psychological impact of Peyronie’s disease: a review. J Sex Med. 2013;10:653–60.
Chung E, Ralph D, Kagioglu A, Garaffa G, Shamsodini A, Bivalacqua T, et al. Evidence-based management guidelines on Peyronie’s disease. J Sex Med. 2016;13:905–23.
Ralph D, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, Usta M, et al. The management of Peyronie’s disease: evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–74.
Gonzalez-Cadavid NF, Rajfer J. Mechanisms of disease: new insights into the cellular and molecular pathology of Peyronie’s disease. Nat Clin Pract Urol. 2005;2:291–7.
Chung E, De Young L, Brock GB. Rat as an animal model for Peyronie’s disease research: a review of current methods and the peer-reviewed literature. Int J Impot Res. 2011;23:235–41.
Badalamente MA, Hurst LC. The biochemistry of Dupuytren’s disease. Hand Clin. 1999;15:35–42. v-vi.
Matos LL, Stabenow E, Tavares MR, Ferraz AR, Capelozzi VL, Pinhal MA. Immunohistochemistry quantification by a digital computer-assisted method compared to semiquantitative analysis. Clin (Sao Paulo). 2006;61:417–24.
Charan J, Kantharia ND. How to calculate sample size in animal studies? J Pharmacol Pharmacother. 2013;4:303–6.
Ahuja SK, Sikka SC, Hellstrom WJ. Stimulation of collagen production in an in vitro model for Peyronie’s disease. Int J Impot Res. 1999;11:207–12.
Qian A, Meals RA, Rajfer J, Gonzalez-Cadavid NF. Comparison of gene expression profiles between Peyronie’s disease and Dupuytren’s contracture. Urology. 2004;64:399–404.
Ratajczak-Wielgomas K, Gosk J, Rabczynski J, Augoff K, Podhorska-Okolow M, Gamian A, et al. Expression of MMP-2, TIMP-2, TGF-beta1, and decorin in Dupuytren’s contracture. Connect Tissue Res. 2012;53:469–77.
Jarvelainen H, Sainio A, Koulu M, Wight TN, Penttinen R. Extracellular matrix molecules: potential targets in pharmacotherapy. Pharmacol Rev. 2009;61:198–223.
Neely AN, Clendening CE, Gardner J, Greenhalgh DG, Warden GD. Gelatinase activity in keloids and hypertrophic scars. Wound Repair Regen. 1999;7:166–71.
Arthur MJ. Fibrogenesis II. Metalloproteinases and their inhibitors in liver fibrosis. Am J Physiol Gastrointest Liver Physiol. 2000;279:G245–9.
Eckes B, Zigrino P, Kessler D, Holtkotter O, Shephard P, Mauch C, et al. Fibroblast-matrix interactions in wound healing and fibrosis. Matrix Biol. 2000;19:325–32.
Ulrich D, Hrynyschyn K, Pallua N. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in sera and tissue of patients with Dupuytren’s disease. Plast Reconstr Surg. 2003;112:1279–86.
McKenzie EA. Heparanase: a target for drug discovery in cancer and inflammation. Br J Pharmacol. 2007;151:1–14.
Dudas J, Kovalszky I, Gallai M, Nagy JO, Schaff Z, Knittel T, et al. Expression of decorin, transforming growth factor-beta 1, tissue inhibitor metalloproteinase 1 and 2, and type IV collagenases in chronic hepatitis. Am J Clin Pathol. 2001;115:725–35.
Beanes SR, Dang C, Soo C, Wang Y, Urata M, Ting K, et al. Down-regulation of decorin, a transforming growth factor-beta modulator, is associated with scarless fetal wound healing. J Pediatr Surg. 2001;36:1666–71.
Imai K, Hiramatsu A, Fukushima D, Pierschbacher MD, Okada Y. Degradation of decorin by matrix metalloproteinases: identification of the cleavage sites, kinetic analyses and transforming growth factor-beta1 release. Biochem J. 1997;322:809–14.
Kozma EM, Olczyk K, Wisowski G, Glowacki A, Bobinski R. Alterations in the extracellular matrix proteoglycan profile in Dupuytren’s contracture affect the palmar fascia. J Biochem. 2005;137:463–76.
Kozma EM, Glowacki A, Olczyk K, Ciecierska M. Dermatan sulfate remodeling associated with advanced Dupuytren’s contracture. Acta Biochim Pol. 2007;54:821–30.
Lopez-Casillas F, Payne HM. Andres IVEotEMCA, Collagen Types I and II by Articular Cartilage-Derived Chondrocytes.J. L., Massague J. Betaglycan can act as a dual modulator of TGF-beta access to signaling receptors: mapping of ligand binding and GAG attachment sites. J Cell Biol. 1994;124:557–68.
Zavadil J, Bitzer M, Liang D, Yang YC, Massimi A, Kneitz S, et al. Genetic programs of epithelial cell plasticity directed by transforming growth factor-beta. Proc Natl Acad Sci USA. 2001;98:6686–91.
Schneevoigt J, Fabian C, Leovsky C, Seeger J, Bahramsoltani M. In vitro expression of the extracellular matrix components aggrecan, collagen types I and II by articular cartilage-derived chondrocytes. Anat Histol Embryol. 2017;46(1):43-50.
Acknowledgements
This work received financial support from FAPESP (São Paulo Research Foundation), CNPq (National Counsel of Technological and Scientific Development) and CAPES (Staff Development Committee of Higher Education).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cohen, D.J., Oliveira, A.V., Theodoro, T.R. et al. Extracellular matrix alterations after blood instillation in tunica albuginea of rats. Int J Impot Res 30, 85–92 (2018). https://doi.org/10.1038/s41443-017-0015-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-017-0015-1
This article is cited by
-
Biglycan: an emerging small leucine-rich proteoglycan (SLRP) marker and its clinicopathological significance
Molecular and Cellular Biochemistry (2021)