Abstract
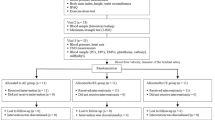
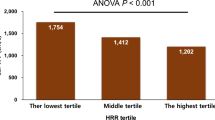
Coronary artery disease and cardiovascular mortality are increased in patients with an exaggerated blood pressure response to exercise. The exact cause of this increase remains unknown, but previous studies have indicated the presence of endothelial dysfunction in peripheral arteries and subclinical atherosclerosis in these patients. The present study aimed to clarify whether coronary microvascular dysfunction is also present in patients with exaggerated blood pressure response to exercise. A total of 95 patients undergoing exercise testing were consecutively enrolled. Flow-mediated vasodilatation and carotid intima-media thickness were measured using standardized methods. A transthoracic echocardiography examination was performed to measure coronary flow velocity reserve. Patients with an exaggerated blood pressure response to exercise had significantly lower coronary flow velocity reserve than the controls (2.06 (1.91–2.36) vs. 2.27 (2.08–2.72), p = 0.004), and this difference was caused by a reduction in hyperemic flow velocity (57.5 (51.3–61.5) vs. 62.0 (56.0–73.0), p = 0.004) rather than a difference in basal flow (26.5 (22.3–29.8) vs. 26.0 (24.0–28.8), p = 0.95). Patients with an exaggerated blood pressure response to exercise also had a significantly greater carotid intima-media thickness and significantly lower flow-mediated vasodilatation than controls. However, an exaggerated blood pressure response to exercise remained a significant predictor of coronary microvascular dysfunction after adjusting for confounders (OR: 3.60, 95% CI: 1.23–10.54, p = 0.02). Patients with an exaggerated blood pressure response to exercise show signs of coronary microvascular dysfunction, in addition to endothelial dysfunction and subclinical atherosclerosis. This finding might explain the increased risk of coronary artery disease and cardiovascular mortality in these patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Miyai N, Arita M, Miyashita K, Morioka I, Shiraishi T, Nishio I. Blood pressure response to heart rate during exercise test and risk of future hypertension. Hypertension. 2002;39:761–6.
Tanaka S, Masuda T, Kamada Y, Hamazaki N, Kamiya K, Ogura MN, et al. Excessive SBP elevation during moderate exercise discriminates patients at high risk of developing left ventricular hypertrophy from hypertensive patients. J Hypertens. 2018;36:1291–8.
Mottram PM, Haluska B, Yuda S, Leano R, Marwick TH. Patients with a hypertensive response to exercise have impaired systolic function without diastolic dysfunction or left ventricular hypertrophy. J Am Coll Cardiol. 2004;43:848–53.
Mariampillai JE, Liestøl K, Kjeldsen SE, Prestgaard EE, Engeseth K, Bodegard J, et al. Exercise systolic blood pressure at moderate workload is linearly associated with coronary disease risk in healthy men. Hypertension. 2020;75:44–50.
Mundal R, Kjeldsen SE, Sandvik L, Erikssen G, Thaulow E, Erikssen J. Exercise blood pressure predicts cardiovascular mortality in middle-aged men. Hypertension. 1994;24:56–62.
Kjeldsen SE, Mundal R, Sandvik L, Erikssen G, Thaulow E, Erikssen J. Supine and exercise systolic blood pressure predict cardiovascular death in middle-aged men. J Hypertens. 2001;19:1343–8.
Stewart KJ, Sung J, Silber HA, Fleg JL, Kelemen MD, Turner KL, et al. Exaggerated exercise blood pressure is related to impaired endothelial vasodilator function. Am J Hypertens. 2004;17:314–20.
Michishita R, Ohta M, Ikeda M, Jiang Y, Yamato H. An exaggerated blood pressure response to exercise is associated with nitric oxide bioavailability and inflammatory markers in normotensive females. Hypertens Res. 2016;39:792–8.
Sicari R, Rigo F, Cortigiani L, Gherardi S, Galderisi M, Picano E. Additive prognostic value of coronary flow reserve in patients with chest pain syndrome and normal or near-normal coronary arteries. Am J Cardiol. 2009;103:626–31.
Brainin P, Frestad D, Prescott E. The prognostic value of coronary endothelial and microvascular dysfunction in subjects with normal or non-obstructive coronary artery disease: A systematic review and meta-analysis. Int J Cardiol. 2018;254:1–9.
Erdogan D, Yildirim I, Ciftci O, Ozer I, Caliskan M, Gullu H, et al. Effects of normal blood pressure, prehypertension, and hypertension on coronary microvascular function. Circulation. 2007;115:593–9.
Caliskan M, Caliskan Z, Gullu H, Keles N, Bulur S, Turan Y, et al. Increased morning blood pressure surge and coronary microvascular dysfunction in patient with early stage hypertension. J Am Soc Hypertens. 2014;8:652–9.
Hamer M, Steptoe A. Vascular inflammation and blood pressure response to acute exercise. Eur J Appl Physiol. 2012;112:2375–9. https://doi.org/10.1007/s00421-011-2210-y
Mavani GP, DeVita MV, Michelis MF. A review of the nonpressor and nonantidiuretic actions of the hormone vasopressin. Front Med (Lausanne). 2015;2:19. https://doi.org/10.3389/fmed.2015.00019. Published 2015 Mar 24
Tasevska I, Enhörning S, Persson M, Nilsson PM, Melander O. Copeptin predicts coronary artery disease cardiovascular and total mortality. Heart. 2016;102:127–32. https://doi.org/10.1136/heartjnl-2015-308183
Schill F, Persson M, Engström G, Melander O, Enhörning S. Copeptin as a marker of atherosclerosis and arteriosclerosis. Atherosclerosis. 2021;338:64–8. https://doi.org/10.1016/j.atherosclerosis.2021.10.012
Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Caliskan M, Turan Y, Caliskan Z, Gullu H, Ciftci FC, Avci E, et al. Previous gestational diabetes history is associated with impaired coronary flow reserve. Ann Med. 2015;47:615–23.
Ciftci FC, Caliskan M, Ciftci O, Gullu H, Uckuyu A, Toprak E, et al. Impaired coronary microvascular function and increased intima-media thickness in preeclampsia. J Am Soc Hypertens. 2014;8:820–6.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. International Brachial Artery Reactivity Task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–65.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–104.
Jae SY, Fernhall B, Heffernan KS, Kang M, Lee MK, Choi YH, et al. Exaggerated blood pressure response to exercise is associated with carotid atherosclerosis in apparently healthy men. J Hypertens. 2006;24:881–7.
Dayanikli F, Grambow D, Muzik O, Mosca L, Rubenfire M, Schwaiger M. Early detection of abnormal coronary flow reserve in asymptomatic men at high risk for coronary artery disease using positron emission tomography. Circulation. 1994;90:808–17.
Ha JW, Juracan EM, Mahoney DW, Oh JK, Shub C, Seward JB, et al. Hypertensive response to exercise: a potential cause for new wall motion abnormality in the absence of coronary artery disease. J Am Coll Cardiol. 2002;39:323–7.
Kelshiker MA, Seligman H, Howard JP, Rahman H, Foley M, Nowbar AN, et al. Coronary flow reserve and cardiovascular outcomes: a systematic review and meta-analysis. Eur Heart J. 2021:ehab775. https://doi.org/10.1093/eurheartj/ehab775.
Hoffman JI. Problems of coronary flow reserve. Ann Biomed Eng. 2000;28:884–96.
Lauer MS, Levy D, Anderson KM, Plehn JF. Is there a relationship between exercise systolic blood pressure response and left ventricular mass? The Framingham Heart Study. Ann Intern Med. 1992;116:203–10. https://doi.org/10.7326/0003-4819-116-3-203
Daida H, Allison TG, Squires RW, Miller TD, Gau GT. Peak exercise blood pressure stratified by age and gender in apparently healthy subjects. Mayo Clin Proc. 1996;71:445–52.
Schultz MG, Hare JL, Marwick TH, Stowasser M, Sharman JE. Masked hypertension is “unmasked” by low-intensity exercise. Blood Press Blood Press. 2011;20:284–9. https://doi.org/10.3109/08037051.2011.566251
Schultz MG, Picone DS, Nikolic SB, Williams AD, Sharman JE. Exaggerated blood pressure response to early stages of exercise stress testing and presence of hypertension. J Sci Med Sport. 2016;19:1039–42. https://doi.org/10.1016/j.jsams.2016.04.004
Kayikcioglu M, Payzin S, Yavuzgil O, Kultursay H, Can LH, Soydan I. Benefits of statin treatment in cardiac syndrome-X1. Eur Heart J. 2003;24:1999–2005.
Pizzi C, Manfrini O, Fontana F, Bugiardini R. Angiotensin-converting enzyme inhibitors and 3-hydroxy-3-methylglutaryl coenzyme A reductase in cardiac Syndrome X: role of superoxide dismutase activity. Circulation. 2004;109:53–8.
Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, Nordenskjöld A, Gard A, et al. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation. 2017;135:1481–9.
Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pr. 1994;38:345–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baycan, Ö.F., Çelik, F.B., Güvenç, T.S. et al. Coronary flow velocity reserve is reduced in patients with an exaggerated blood pressure response to exercise. Hypertens Res 45, 1653–1663 (2022). https://doi.org/10.1038/s41440-022-00995-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00995-0
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
Pathophysiology of the exaggerated blood pressure response to exercise
Hypertension Research (2022)