Abstract
Hypertension is a leading cause of cardiovascular disease and despite established strategies to lower blood pressure, the control of hypertension remains poor. This is true even in high-income countries with well-established welfare and medical systems. Among the social factors associated with hypertension (i.e., social determinants of hypertension, SDHT), individual socioeconomic status (SES), including education, income, and occupation, can be crucial for hypertension management (prevalence, awareness, treatment, and control). This article reviews the findings of recently published studies that examined the association between SES and hypertension management in high-income countries. It also discusses social prescribing, which targets social isolation and loneliness as modifiable SDHT to improve hypertension management.
Similar content being viewed by others
Introduction
High blood pressure (BP, hypertension) is a leading cause of cardiovascular disease. Between 1990 and 2015, the prevalence of elevated systolic BP (≥140 mmHg) substantially increased, and disability-adjusted life-years and deaths associated with elevated BP also increased [1]. This high prevalence of hypertension is consistent globally, regardless of a country’s income status: low, middle, or high [2]. To minimize the burden of hypertension, several guidelines emphasize the management of the hypertension cascade: development (prevalence), screening (to promote awareness), treatment, and control [3,4,5]. The control of hypertension has generally improved in recent decades [3, 6]; however, despite the availability of low-cost and effective antihypertensive medications, the rates of controlled hypertension remain less than 50%, even in high-income countries [2, 3].
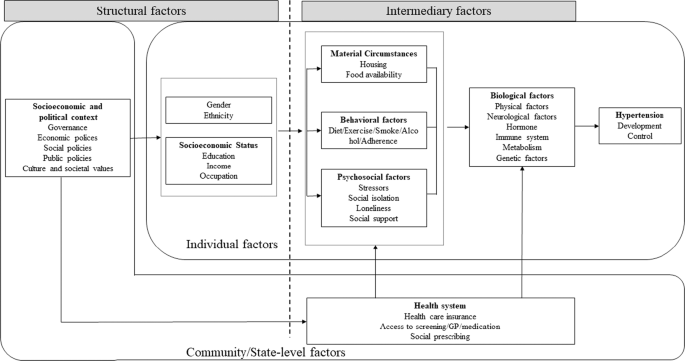
Primordial prevention aims to avoid the establishment of social, economic, and environmental conditions that contribute to an elevated risk of disease [7, 8]. Among these conditions, social factors, particularly individual socioeconomic status (SES) measures, including educational attainment, income level, and occupation, have been repeatedly found to be associated with hypertension (i.e., social determinants of hypertension, SDHT) (Fig. 1) [2, 9, 10]. Intermediary factors of individual SES that lead to hypertension development include material circumstances (e.g., housing and healthy food availability), behavioral factors (e.g., diet, exercise, smoking, and alcohol consumption), and psychosocial factors (e.g., stressors, social isolation, and loneliness). Individual SES can also affect hypertension control via these same factors and additional behavioral factors, such as adherence to medical guidance and medication, which can be influenced by community/state-level factors such as the level of national health systems.
Conceptual framework of social determinants of hypertension. Based on World Health Organization (2010) [10]
This article evaluated the SDHT and hypertension management cascade (prevalence/incidence, awareness, treatment, and control). It was restricted to studies in high-income countries with well-established welfare and medical systems because the effect of these factors on hypertension management was expected to vary across various levels of national medical systems. Furthermore, this review focused on social isolation and loneliness as modifiable SDHT to improve hypertension management from the perspective of social prescribing.
SES and hypertension
A literature review of articles published between January 2000 and June 2021 was performed via the MEDLINE database to assess the influence of SES on the prevalence/incidence, awareness, treatment, and control of hypertension in high-income countries. We included the keywords “socioeconomic factors” (MeSH) or “socioeconomic factors” and “hypertension” in the title/abstract search, and added “prevalence,” “incidence,” “awareness,” “treatment,” or “control”. The titles and abstracts of the references were screened and those that were apparently irrelevant reports were excluded. We retrieved full-text articles for the remaining references and screened them to identify studies for inclusion. Our inclusion criteria were articles written in English and studies conducted in high-income countries. The Supplementary Table presents the data on the detailed study characteristics of the included studies.
Education and hypertension
The association between education and hypertension prevalence/incidence in high-income countries is relatively consistent [2, 11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. A meta-analysis, for example, reported that lower educational attainment is associated with an increased prevalence/incidence of hypertension in high-income countries (odds ratio [OR] (lowest vs. highest education level category): 1.69 [95% confidential interval: 1.49 to 1.91]) [9].
In general, the role of education in improving the awareness, treatment, and control of hypertension in high-income countries seems to be small. Several studies reported a null association between education and hypertension awareness [2, 11, 16, 21, 30,31,32,33,34,35], treatment [2, 16, 18, 32, 33, 35, 36], and control [2, 11, 15, 19, 21, 22, 30,31,32,33, 35, 37, 38]. A few studies have reported a significant but inconsistent association between education and hypertension awareness and treatment. For example, a study in South Korea reported an association between educational attainment and better awareness among women [15], while a study in Spain reported greater awareness among people with lower educational attainment [18]. Two studies conducted in Singapore [11] and South Korea [19] reported better treatment among people with high educational attainment, while three studies in Switzerland [21], Australia [39], and Japan [30] reported lower treatment among these people those. The reasons behind such inconsistent findings remain unclear. In some settings, highly educated people may think that they can manage their BP with a nonpharmacological approach or that a nonpharmacological approach might be presented more often by general practitioners (GPs). However, the associations, although only observed in a few studies in Spain [18], Austria [40], and France [41], between education and hypertension control are consistent. In some high-income countries, hypertension in people with high educational attainment might be better controlled than in those with low educational attainment.
Income and hypertension
The association between income and hypertension prevalence/incidence in high-income countries is relatively consistent [11, 12, 15, 22, 25, 42, 43]. A meta-analysis, for example, reported that lower income is associated with an increased prevalence/incidence of hypertension in high-income countries (OR (lowest vs. highest income category)): 1.36 ([1.16 to 1.59]) [9].
In general, it seems that income does not play an important role in improving the awareness, treatment, and control of hypertension in high-income countries. Several studies reported a null association between income and hypertension awareness [19, 30, 32, 33, 36], treatment [19, 30, 32, 33, 36], and control [11, 15, 19, 30, 32]. Only a few studies have reported positive associations between income level and hypertension treatment (Singapore [11] and the United States [44]) and control (the United States [33, 45]). Income may improve the treatment and control of hypertension only in limited settings.
Occupation and hypertension
Although evidence for employment is relatively scarce compared to that for education and income, employment has been associated with lower hypertension prevalence/incidence in high-income countries [14, 16, 22]. A meta-analysis, for example, indicated that a lower occupational grade is associated with an increased prevalence/incidence of hypertension in high-income countries (OR (lowest vs. highest occupational grade category): 1.63 (1.27 to 2.09)) [9].
The evidence for occupation and the awareness/treatment/control of hypertension is scarce and inconclusive. Some recent studies showed a null association between employment and hypertension awareness [11, 30], treatment [11, 19], and control [30, 37]. Meanwhile, a study in Finland [16] showed that retirement is associated with better awareness of hypertension than being employed, while a study in Scotland [35] showed that unemployment due to sickness is associated with better awareness than full-time employment. Two studies in Japan [30] and Australia [39] showed that unemployment is associated with better treatment compared to employment. A study in Finland [16] showed that retirement, but not unemployment, is associated with better treatment compared to employment. A study in Scotland [35] showed that those who are unemployed and seeking work undergo worse treatment than those with full-time jobs, while unemployment due to sickness was associated with better treatment than full-time employment. A few reports have shown null [30, 37] associations between employment and hypertension control. A study in Singapore [11] showed that retirement/unemployment was associated with better control compared to employment/studying full-time. A study in Scotland [35] showed that being a homemaker or retired was associated with worse control compared to having a full-time job.
Care should be taken while interpreting the findings in this field because the situations of people with different employment statuses cannot be described simply. For example, the notion of unemployment was defined differently in the studies mentioned above. Some studies differentiated between students, homemakers, retired people, people seeking work, and people with sickness, while others did not. Even among employed people, full-time work and part-time work differently affect the hypertension care cascade because, for example, people with full-time jobs have less time to visit their general practitioner than people with part-time jobs and those who do not work.
Future directions
In high-income countries, individuals with high SES, such as those with high educational attainment, high income, and employment, are consistently associated with a low prevalence of hypertension. Several pathways can be identified, such as disparities in material circumstances, health behaviors (e.g., due to less health literacy, learned effectiveness, and personal control) [46, 47], and psychological stressors (i.e., due to a low problem-solving ability) [48, 49] between people with high and low SES. Closing the SES gap, as a long-term strategy, and/or reducing disparities in intermediary factors of SDHT between people with high and low SES are potential approaches to reduce disparities in hypertension prevalence in high-income countries.
However, SES is not likely to play an important role in hypertension control. This is probably because once established welfare and health care systems are achieved, these factors do not considerably change the accessibility to medical care or the affordability of antihypertensive drugs in contrast to their expected changes in low-income countries where health systems are often weak. In this context, closing the gap in SES is not considered a promising approach to improve hypertension control.
Targeting modifiable intermediary factors of SDHT: Social prescribing
A possible target of SDHT is a modifiable intermediary factor. Social prescribing, which is “a way of linking patients in primary care with sources of support within the community [50],” can be an approach to improve some psychosocial factors, such as social isolation (the objective state of having few social connections with others) and loneliness (a subjective feeling of being isolated) [51, 52]. In response to increasing concerns about the societal and health impacts of social isolation and loneliness [53, 54], some countries, such as the UK and Japan, have recently appointed “ministers of loneliness”.
Social isolation/loneliness and hypertension
Although evidence is limited, a few studies have reported the prevalence of an association between hypertension and social isolation, as well as loneliness and elevated BP in the U.S [55, 56]. Possible mechanisms by which social isolation and loneliness influence BP levels and hypertension control are psychological stress [57] and social contagion: [58] behaviors spread in a social network through the diffusion of information or the transmission of behavioral norms. Health-related behaviors, such as physical activity, smoking, and medication adherence, can be adversely affected in the case of socially isolated people with a small social network [54, 59]. However, little is known about how social isolation and loneliness are related to the awareness, treatment, and control of hypertension.
Social prescribing for hypertension
A systematic review suggested that the current evidence is insufficient to demonstrate definitive guidance for social prescribing [50]. There is little evidence for hypertension; however, some studies that focused on social participation suggest the potential of social prescribing in hypertension care. A cross-sectional study and a longitudinal study in Japan, for example, reported the association of membership in social organizations with a lower prevalence of hypertension [60, 61]. A multilevel analysis showed a lower prevalence of hypertension among people in communities with high proportions of people participating in social organizations, suggesting a spillover effect of social participation on hypertension: [62] hypertension might be prevented only by living in communities that are rich in social participation.
A study in Sweden reported that low social participation is associated with low adherence to antihypertensive medication [63]. Although a cross-national analysis showed that membership in social organizations was associated with control in lower-middle-income/low-income countries but not in high-income/upper-middle-income countries [64], a recent study in Japan showed an association between social participation and better control of hypertension among older people [65].
Future directions
The role of social prescribing in improving hypertension control is inconclusive. However, the lack of robust evidence does not necessarily mean that social prescribing is ineffective. Future studies should address the complex issue of social prescribing. Furthermore, wide variations in the nature of the interventions are required [51].
Face-to-face social interaction, which is supposed to be prescribed in social prescribing, can be restricted in specific settings, such as the ongoing COVID-19 pandemic. Social connections on the internet are a possible alternative to face-to-face social interactions in this case. The use of the internet for communication, for example, has been related to fewer feelings of loneliness [66] and the onset of depression [67], suggesting a simultaneous BP-lowering effect among people who use the internet to communicate. Although this remains unclear, social contagion might also be observed in online social connections where health-related behaviors, such as physical activity, smoking, and medication adherence, can be altered. Future studies should examine the role of online social connections in hypertension control as a new resource that is referred to in social prescribing.
Conclusion
Determinants of hypertension and its care are diverse and often interconnected; therefore, holistic and comprehensive approaches are required. This article highlighted the contribution of the SDHT in high-income countries. The SDHT are a crucial factor in understanding the dynamics of hypertension. Future studies should examine whether intervening in SDHT is effective in reducing hypertension prevalence and achieving optimal hypertension control. Particularly, social prescribing, which involves referring people to community resources to reduce social isolation and loneliness via face-to-face and online connections, has the potential to improve hypertension control.
References
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global Burden of Hypertension and Systolic Blood Pressure of at Least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82.
Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. Group ESD. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2018;71:e127–248.
Beckman AL, Herrin J, Nasir K, Desai NR, Spatz ES. Trends in cardiovascular Health of US Adults by Income, 2005-2014. JAMA Cardiol. 2017;2:814–6.
Bonita R, Beaglehole R, Kjellström T, World Health O. Basic epidemiology. 2nd ed ed. Geneva: World Health Organization; 2006.
Social Determinants of Health in Non-communicable Diseases: Case Studies from Japan: Springer Nature, 2020.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33:221–9.
Organization WH. A Conceptual Framework for Action on the Social Determinants of Health 2010.
Liew SJ, Lee JT, Tan CS, Koh CHG, Van Dam R, Müller-Riemenschneider F. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: a cross-sectional study. BMJ Open. 2019;9:e025869.
Gee ME, Bienek A, McAlister FA, Robitaille C, Joffres M, Tremblay MS, et al. Factors associated with lack of awareness and uncontrolled high blood pressure among Canadian adults with hypertension. Can J Cardiol. 2012;28:375–82.
Yip W, Wong TY, Jonas JB, Zheng Y, Lamoureux EL, Nangia V, et al. Prevalence, awareness, and control of hypertension among Asian Indians living in urban Singapore and rural India. J Hypertens. 2013;31:1539–46.
Rodrigues AP, Gaio V, Kislaya I, Graff-Iversen S, Cordeiro E, Silva AC, et al. Sociodemographic disparities in hypertension prevalence: Results from the first Portuguese National Health Examination Survey. Rev Port Cardiol (Engl Ed). 2019;38:547–55.
Lee HY. Socioeconomic Disparities in the Prevalence, Diagnosis, and Control of Hypertension in the Context of a Universal Health Insurance System. J Korean Med Sci. 2017;32:561–7.
Sivén SS, Niiranen TJ, Aromaa A, Koskinen S, Jula AM. Social, lifestyle and demographic inequalities in hypertension care. Scand J Public Health. 2015;43:246–53.
Redondo A, Benach J, Subirana I, Martinez JM, Muñoz MA, Masiá R, et al. Trends in the prevalence, awareness, treatment, and control of cardiovascular risk factors across educational level in the 1995-2005 period. Ann Epidemiol. 2011;21:555–63.
Perez-Fernandez R, Mariño AF, Cadarso-Suarez C, Botana MA, Tome MA, Solache I, et al. Prevalence, awareness, treatment and control of hypertension in Galicia (Spain) and association with related diseases. J Hum Hypertens. 2007;21:366–73.
Cha SH, Park HS, Cho HJ. Socioeconomic disparities in prevalence, treatment, and control of hypertension in middle-aged Koreans. J Epidemiol. 2012;22:425–32.
Bann D, Fluharty M, Hardy R, Scholes S. Socioeconomic inequalities in blood pressure: co-ordinated analysis of 147,775 participants from repeated birth cohort and cross-sectional datasets, 1989 to 2016. BMC Med. 2020;18:338.
Guessous I, Bochud M, Theler JM, Gaspoz JM, Pechère-Bertschi A. 1999-2009 Trends in prevalence, unawareness, treatment and control of hypertension in Geneva, Switzerland. PLoS One. 2012;7:e39877.
Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: Analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS One. 2017;12:e0178334.
Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA 2018;320:1338–48.
Park CS, Ha KH, Kim HC, Park S, Ihm SH, Lee HY. The Association between Parameters of Socioeconomic Status and Hypertension in Korea: the Korean Genome and Epidemiology Study. J Korean Med Sci. 2016;31:1922–8.
Baek TH, Lee HY, Lim NK, Park HY. Gender differences in the association between socioeconomic status and hypertension incidence: the Korean Genome and Epidemiology Study (KoGES). BMC Public Health. 2015;15:852.
Pereira M, Lunet N, Paulo C, Severo M, Azevedo A, Barros H. Incidence of hypertension in a prospective cohort study of adults from Porto, Portugal. BMC Cardiovasc Disord. 2012;12:114.
Conen D, Glynn RJ, Ridker PM, Buring JE, Albert MA. Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009;30:1378–84.
Dupre ME. Educational differences in health risks and illness over the life course: a test of cumulative disadvantage theory. Soc Sci Res. 2008;37:1253–66.
Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment: the NHANES I epidemiologic followup study. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152:272–8.
Satoh A, Arima H, Ohkubo T, Nishi N, Okuda N, Ae R, et al. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J Hypertens. 2017;35:401–8.
Abu-Saad K, Chetrit A, Eilat-Adar S, Alpert G, Atamna A, Gillon-Keren M, et al. Blood pressure level and hypertension awareness and control differ by marital status, sex, and ethnicity: a population-based study. Am J Hypertens. 2014;27:1511–20.
Nguyen QC, Waddell EN, Thomas JC, Huston SL, Kerker BD, Gwynn RC. Awareness, treatment, and control of hypertension and hypercholesterolemia among insured residents of New York City, 2004. Prev Chronic Dis. 2011;8:A109.
Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–65.
Tompkins G, Forrest LF, Adams J. Socio-economic differences in the association between self-reported and clinically present diabetes and hypertension: secondary analysis of a population-based cross-sectional study. PLoS One. 2015;10:e0139928.
Chen R, Tunstall-Pedoe H, Morrison C, Connaghan J, A’Brook R. Trends and social factors in blood pressure control in Scottish MONICA surveys 1986-1995: the rule of halves revisited. J Hum Hypertens. 2003;17:751–9.
Vallée A, Grave C, Gabet A, Blacher J, Olié V. Treatment and adherence to antihypertensive therapy in France: the roles of socioeconomic factors and primary care medicine in the ESTEBAN survey. Hypertens Res. 2021;44:550–60.
McNaughton CD, Jacobson TA, Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96:165–70.
Patel R, Lawlor DA, Whincup P, Montaner D, Papacosta O, Brindle P, et al. The detection, treatment and control of high blood pressure in older British adults: cross-sectional findings from the British Women’s Heart and Health Study and the British Regional Heart Study. J Hum Hypertens. 2006;20:733–41.
Appleton SL, Neo C, Hill CL, Douglas KA, Adams RJ. Untreated hypertension: prevalence and patient factors and beliefs associated with under-treatment in a population sample. J Hum Hypertens. 2013;27:453–62.
Rohla M, Haberfeld H, Tscharre M, Huber K, Weiss TW. Awareness, treatment, and control of hypertension in Austria: a multicentre cross-sectional study. J Hypertens. 2016;34:1432–40.
de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cances V, Maitre A, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension 2002;39:1119–25.
Andersen UO, Jensen GB. Gender difference and economic gradients in the secular trend of population systolic blood pressure. Eur J Intern Med. 2013;24:568–72.
Matthews KA, Kiefe CI, Lewis CE, Liu K, Sidney S, Yunis C. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension 2002;39:772–6.
LeBrón AM, Schulz AJ, Mentz G, Gamboa C, Reyes A. Antihypertensive Medication Use: Implications for Inequities in Cardiovascular Risk and Opportunities for Intervention. J Health Care Poor Underserved. 2018;29:192–201.
Shahu A, Herrin J, Dhruva SS, Desai NR, Davis BR, Krumholz HM, et al. Disparities in socioeconomic context and association with blood pressure control and cardiovascular outcomes in ALLHAT. J Am Heart Assoc. 2019;8:e012277.
Nowotny KM, Masters RK, Boardman JD. The relationship between education and health among incarcerated men and women in the United States. BMC Public Health. 2016;16:916.
Pampel FC, Krueger PM, Denney JT. Socioeconomic Disparities in Health Behaviors. Annu Rev Socio. 2010;36:349–70.
D’Zurilla TJ, Sheedy CF. Relation between social problem-solving ability and subsequent level of psychological stress in college students. J Personal Soc Psychol. 1991;61:841.
Manstead ASR. The psychology of social class: How socioeconomic status impacts thought, feelings, and behaviour. Br J Soc Psychol. 2018;57:267–91.
Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017;7:e013384.
Drinkwater C, Wildman J, Moffatt S. Social prescribing. BMJ 2019;364:l1285.
Reinhardt GY, Vidovic D, Hammerton C. Understanding loneliness: a systematic review of the impact of social prescribing initiatives on loneliness. Perspect Public Health. 2021;141:204–13.
Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483.
National Academies of Sciences E, and Medicine. Social isolation and loneliness in older adults Opportunities for the health care system. Washington, DC: The National Academies Press; 2020.
Yang YC, Li T, Ji Y. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health. 2013;13:1210.
Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25:132–41.
Ernst JM, Cacioppo JT. Lonely hearts: psychological perspectives on loneliness. Appl Preventive Psychol. 1999;8:1–22.
Berkman LF, Kawachi I, Glymour MM. Social epidemiology. 2nd ed. New York (NY): Oxford University Press; 2014.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–18.
Yazawa A, Inoue Y, Fujiwara T, Stickley A, Shirai K, Amemiya A, et al. Association between social participation and hypertension among older people in Japan: the JAGES Study. Hypertens Res. 2016;39:818–24.
Oshio T, Kan M. Preventive impact of social participation on the onset of non-communicable diseases among middle-aged adults: A 10-wave hazards-model analysis in Japan. Prev Med. 2019;118:272–8.
Nakagomi A, Tsuji T, Hanazato M, Kobayashi Y, Kondo K. Association between community-level social participation and self-reported hypertension in older Japanese: A JAGES multilevel cross-sectional study. Am J Hypertens. 2019;32:503–14.
Johnell K, Råstam L, Lithman T, Sundquist J, Merlo J. Low adherence with antihypertensives in actual practice: the association with social participation–a multilevel analysis. BMC Public Health. 2005;5:17.
Palafox B, Goryakin Y, Stuckler D, Suhrcke M, Balabanova D, Alhabib KF, et al. Does greater individual social capital improve the management of hypertension? Cross-national analysis of 61 229 individuals in 21 countries. BMJ Glob Health. 2017;2:e000443.
Ueno T, Nakagomi A, Tsuji T, Kondo K Association between social participation and hypertension control among older people with self-reported hypertension in Japanese communities. Hypertension Res. 2022. https://doi.org/10.1038/s41440-022-00953-w.
Szabo A, Allen J, Stephens C, Alpass F. Longitudinal analysis of the relationship between purposes of internet use and well-being among older adults. Gerontologist. 2019;59:58–68.
Nakagomi A, Shiba K, Kondo K, Kawachi I Can online communication prevent depression among older people? A longitudinal analysis. J Appl Gerontol. 2020:733464820982147.
Acknowledgements
This study was supported by the Open Innovation Platform with Enterprises, Research Institute and Academia (OPERA, JPMJOP1831) from the Japan Science and Technology (JST). The funding source had no role in the study design, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nakagomi, A., Yasufuku, Y., Ueno, T. et al. Social determinants of hypertension in high-income countries: A narrative literature review and future directions. Hypertens Res 45, 1575–1581 (2022). https://doi.org/10.1038/s41440-022-00972-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00972-7
Keywords
This article is cited by
-
Modifiable risk factors of inequalities in hypertension: analysis of 100 million health checkups recipients
Hypertension Research (2024)
-
The association of body composition and fat distribution with hypertension in community-dwelling older adults: the Bushehr Elderly Health (BEH) program
BMC Public Health (2023)
-
Treatment Intensity, Prescribing Patterns, and Blood Pressure Control in Rural Black Patients with Uncontrolled Hypertension
Journal of Racial and Ethnic Health Disparities (2023)