Abstract
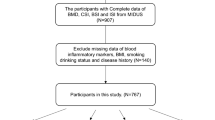
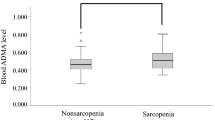
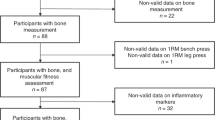
Calciprotein particles (CPPs) are tiny mineral–protein aggregates consisting of calcium-phosphate and fetuin-A. Recent studies have suggested that CPPs may contribute to the pathogenesis of chronic inflammation and arteriosclerosis. Reduced skeletal muscle mass and strength reportedly contribute independently to increased serum phosphate levels. This finding suggests that reduced skeletal muscle mass and strength can endogenously induce an increase in circulating CPP levels. Therefore, we investigated the potential association between circulating CPP levels and skeletal muscle mass and strength in middle-aged and older adults. One hundred eighty-two middle-aged and older adults (age, 46–83 years) were included in this cross-sectional study (UMIN000034741). Circulating CPP levels were measured using the gel filtration method. Appendicular skeletal muscle mass was assessed using multifrequency bioelectrical impedance analysis with a tetrapolar eight-point tactile electrode system. The skeletal muscle mass index was calculated from appendicular skeletal muscle mass and height. Handgrip and knee extension strengths were used as measures of skeletal muscle strength. The skeletal muscle mass index was negatively correlated with circulating CPP levels (r = −0.31; P < 0.05). This association remained significant after adjustment for potential covariates (β = −0.34; P < 0.05). In contrast, skeletal muscle strength, represented by handgrip strength and knee extension strength, was not significantly associated with circulating CPP levels. In middle-aged and older adults, a lower skeletal muscle mass index was independently associated with higher circulating CPP levels. The present results suggest that maintaining skeletal muscle mass may prevent an increase in circulating CPP levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Lüscher TF. Prevention: some important steps forward, but many unmet needs in a world with cardiovascular disease as the leading cause of death. Eur Heart J. 2016;37:3179–81.
Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24:1161–70.
Rogers MA, Aikawa E. Cardiovascular calcification: artificial intelligence and big data accelerate mechanistic discovery. Nat Rev Cardiol. 2019;16:261–74.
Heiss A, DuChesne A, Denecke B, Grötzinger J, Yamamoto K, Renneé T, et al. Structural basis of calcification inhibition by α2-HS glycoprotein/fetuin-A: formation of colloidal calciprotein particles. J Biol Chem. 2003;278:13333–41. https://doi.org/10.1074/jbc.M210868200.
Hu MC, Shiizaki K, Kuro-o M, Moe OW. Fibroblast growth factor 23 and Klotho: physiology and pathophysiology of an Endocrine Network of Mineral Metabolism. Annu Rev Physiol. 2013;75:503–33. https://doi.org/10.1146/annurev-physiol-030212-183727.
Kuro-o M. The Klotho proteins in health and disease. Nat Rev Nephrol. 2019;15:27–44. https://doi.org/10.1038/s41581-018-0078-3.
Kuro-O M. Phosphate as a pathogen of arteriosclerosis and aging. J Atheroscler Thromb. 2021;28:203–13.
Hamano T, Matsui I, Mikami S, Tomida K, Fujii N, Imai E, et al. Fetuin-mineral complex reflects extraosseous calcification stress in CKD. J Am Soc Nephrol. 2010;21:1998–2007. https://doi.org/10.1681/ASN.2009090944.
Smith ER, Ford ML, Tomlinson LA, Rajkumar C, McMahon LP, Holt SG. Phosphorylated fetuin-A-containing calciprotein particles are associated with aortic stiffness and a procalcific milieu in patients with pre-dialysis CKD. Nephrol Dial Transplant. 2012;27:1957–66. https://doi.org/10.1093/ndt/gfr609.
Smith ER, Cai MM, McMahon LP, Pedagogos E, Toussaint ND, Brumby C, et al. Serum fetuin-A concentration and fetuin-A-containing calciprotein particles in patients with chronic inflammatory disease and renal failure. Nephrology. 2013;18:215–21. https://doi.org/10.1111/nep.12021.
Miura Y, Iwazu Y, Shiizaki K, Akimoto T, Kotani K, Kurabayashi M, et al. Identification and quantification of plasma calciprotein particles with distinct physical properties in patients with chronic kidney disease. Sci Rep. 2018;8:1256 https://doi.org/10.1038/s41598-018-19677-4.
Chen YY, Kao TW, Chou CW, Wu CJ, Yang HF, Lai CH, et al. Exploring the link between serum phosphate levels and low muscle strength, dynapenia, and sarcopenia. Sci Rep. 2018;8:3573. https://doi.org/10.1038/s41598-018-21784-1.
Mastorakos G, Valsamakis G, Paltoglou G, Creatsas G. Management of obesity in menopause: diet, exercise, pharmacotherapy and bariatric surgery. Maturitas. 2010;65:219–24.
Zaydun G, Tomiyama H, Hashimoto H, Arai T, Koji Y, Yambe M, et al. Menopause is an independent factor augmenting the age-related increase in arterial stiffness in the early postmenopausal phase. Atherosclerosis. 2006;184:137–42. https://doi.org/10.1016/j.atherosclerosis.2005.03.043.
Enomoto M, Adachi H, Fukami A, Kumagai E, Nakamura S, Nohara Y, et al. A useful tool as a medical checkup in a general population—bioelectrical impedance analysis. Front Cardiovasc Med. 2017;4:3. https://doi.org/10.3389/fcvm.2017.00003.
Lee SY, Ahn S, Kim YJ, Ji MJ, Kim KM, Choi SH, et al. Comparison between dual-energy x-ray absorptiometry and bioelectrical impedance analyses for accuracy in measuring whole body muscle mass and appendicular skeletal muscle mass. Nutrients. 2018;10:738. https://doi.org/10.3390/nu10060738.
Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 2016;31:643–50.
Kamide N, Kamiya R, Nakazono T, Ando M. Reference values for hand grip strength in Japanese community-dwelling elderly: a meta-analysis. Environ Health Prev Med. 2015;20:441–6. https://doi.org/10.1007/s12199-015-0485-z.
Suzuki M, Yamada S, Inamura A, Omori Y, Kirimoto H, Sugimura S, et al. Reliability and validity of measurements of knee extension strength obtained from nursing home residents with dementia. Am J Phys Med Rehabil. 2009;88:924–33. https://doi.org/10.1097/PHM.0b013e3181ae1003.
Hiraki K, Yasuda T, Hotta C, Izawa KP, Morio Y, Watanabe S, et al. Decreased physical function in pre-dialysis patients with chronic kidney disease. Clin Exp Nephrol. 2013;17:225–31. https://doi.org/10.1007/s10157-012-0681-8.
Katoh M, Yamasaki H. Comparison of reliability of isometric leg muscle strength measurements made using a hand-held dynamometer with and without a restraining belt. J Phys Ther Sci. 2009;21:37–42. https://doi.org/10.1589/jpts.21.37.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. GFR estimation using standardized serum cystatin C in Japan. Am J Kidney Dis. 2013;61:197–203. https://doi.org/10.1053/j.ajkd.2012.07.007.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92. https://doi.org/10.1053/j.ajkd.2008.12.034.
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. Performance of GFR equations in Japanese subjects. Clin Exp Nephrol. 2013;17:352–8. https://doi.org/10.1007/s10157-012-0704-5.
Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese Clinical Practice Guideline for Diabetes 2019. Diabetol Int. 2020;11:165–223. https://doi.org/10.1007/s13340-020-00439-5.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481. https://doi.org/10.1038/S41440-019-0284-9.
Rogerson PA. Statistical Methods for Geography. SAGE Publ Ltd; Thousand Oaks, CA, USA. 2001.
Kim KM, Lim S, Oh TJ, Moon JH, Choi SH, Lim JY, et al. Longitudinal changes in muscle mass and strength, and bone mass in older adults: gender-specific associations between muscle and bone losses. J Gerontol Ser A Biol Sci Med Sci. 2018;73:1062–9. https://doi.org/10.1093/gerona/glx188.
Anagnostis P, Gkekas NK, Achilla C, Pananastasiou G, Taouxidou P, Mitsiou M, et al. Type 2 diabetes mellitus is associated with increased risk of sarcopenia: a systematic review and meta-analysis. Calcif Tissue Int. 2020;107:453–63.
Bai T, Fang F, Li F, Ren Y, Hu J, Cao J. Sarcopenia is associated with hypertension in older adults: a systematic review and meta-analysis. BMC Geriatr. 2020;20:279. https://doi.org/10.1186/s12877-020-01672-y.
Gatate Y, Nakano S, Mizuno Y, Muramatsu T, Senbonmatsu T, Nishimura S, et al. Mid-term predictive value of calciprotein particles in maintenance hemodialysis patients based on a gel-filtration assay. Atherosclerosis. 2020;303:46–52. https://doi.org/10.1016/j.atherosclerosis.2020.03.016.
Suzuki Y, Mitsushima S, Kato A, Yamaguchi T, Ichihara S. High-phosphorus/zinc-free diet aggravates hypertension and cardiac dysfunction in a rat model of the metabolic syndrome. Cardiovasc Pathol. 2014;23:43–49. https://doi.org/10.1016/j.carpath.2013.06.004.
Bozic M, Panizo S, Sevilla MA, Riera M, Soler MJ, Pascual J, et al. High phosphate diet increases arterial blood pressure via a parathyroid hormone mediated increase of renin. J Hypertens. 2014;32:1822–32. https://doi.org/10.1097/HJH.0000000000000261.
Mohammad J, Scanni R, Bestmann L, Hulter HN, Krapf R. A controlled increase in dietary phosphate elevates BP in healthy human subjects. J Am Soc Nephrol. 2018;29:2089–98. https://doi.org/10.1681/ASN.2017121254.
Kuro-o M. Klotho, phosphate and FGF-23 in ageing and disturbed mineral metabolism. Nat Rev Nephrol. 2013;9:650–60. https://doi.org/10.1038/nrneph.2013.111.
Gruber M, Greisen P, Junker CM, Hélix-Nielsen C. Phosphorus binding sites in proteins: structural preorganization and coordination. J Phys Chem B. 2014;118:1207–15. https://doi.org/10.1021/jp408689x.
Westheimer FH. Why nature chose phosphates. Science. 1987;235:1173–8. https://doi.org/10.1126/science.2434996.
Morley JE, Anker SD, von Haehling S. Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology—update 2014. J Cachexia Sarcopenia Muscle. 2014;5:253–9.
Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012;24:623–7. https://doi.org/10.1097/BOR.0b013e328358d59b
Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol. 2003;95:1717–27.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: The Health, Aging and Body Composition Study. J Gerontol Ser A Biol Sci Med Sci. 2006;61:1059–64. https://doi.org/10.1093/gerona/61.10.1059.
Tonelli M, Sacks F, Pfeffer M, Gao Z, Curhan G. Relation between serum phosphate level and cardiovascular event rate in people with coronary disease. Circulation. 2005;112:2627–33. https://doi.org/10.1161/CIRCULATIONAHA.105.553198.
Narang R, Ridout D, Nonis C, Kooner JS. Serum calcium, phosphorus and albumin levels in relation to the angiographic severity of coronary artery disease. Int J Cardiol. 1997;60:73–79. https://doi.org/10.1016/S0167-5273(97)02971-9.
Peri-Okonny P, Baskin KK, Iwamoto G, Mitchell JH, Smith SA, Kim HK, et al. High-phosphate diet induces exercise intolerance and impairs fatty acid metabolism in mice. Circulation. 2019;139:1422–34. https://doi.org/10.1161/CIRCULATIONAHA.118.037550.
Schaap LA, Pluijm SMF, Deeg DJH, Visser M. Inflammatory markers and loss of muscle mass (Sarcopenia) and strength. Am J Med. 2006;119:526.e9–17. https://doi.org/10.1016/j.amjmed.2005.10.049.
Navarro-González JF, Mora-Fernández C, Muros M, Herrera H, García J. Mineral metabolism and inflammation in chronic kidney disease patients: a cross-sectional study. Clin J Am Soc Nephrol. 2009;4:1646–54. https://doi.org/10.2215/CJN.02420409.
Li X, Moody MR, Engel D, Walker S, Clubb FJ, Sivasubramanian N, et al. Cardiac-specific overexpression of tumor necrosis factor-α causes oxidative stress and contractile dysfunction in mouse diaphragm. Circulation. 2000;102:1690–6. https://doi.org/10.1161/01.CIR.102.14.1690.
Hughes VA, Frontera WR, Wood M, Evans WJ, Dallal GE, Roubenoff R, et al. Longitudinal muscle strength changes in older adults: Influence of muscle mass, physical activity, and health. J Gerontol Ser A Biol Sci Med Sci. 2001;56:209–17. https://doi.org/10.1093/gerona/56.5.B209.
Karlsson MK, Obrant KJ, Nilsson BE, Johnell O. Changes in bone mineral, lean body mass and fat content as measured by dual energy X-ray absorptiometry: a longitudinal study. Calcif Tissue Int. 2000;66:97–99. https://doi.org/10.1007/s002230010020.
Baumgartner RN, Waters DL, Gallagher D, Morley JE, Garry PJ. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev. 1999;107:123–36. https://doi.org/10.1016/S0047-6374(98)00130-4.
Waters DL, Yau CL, Montoya GD, Baumgartner RN. Serum sex hormones, IGF-1, and IGFBP3 exert a sexually dimorphic effect on lean body mass in aging. J Gerontol Ser A Biol Sci Med Sci. 2003;58:648–52. https://doi.org/10.1093/gerona/58.7.m648.
Bhasin S, Storer TW, Berman N, Callegari C, Clevenger B, Phillips J, et al. The effects of supraphysiologic doses of testosterone on muscle size and strength in normal men. N Engl J Med. 1996;335:1–7. https://doi.org/10.1056/NEJM199607043350101.
Acknowledgements
The authors would like to thank all participants in the study. We also thank our (SM’s) laboratory members and Michiru Hotta at the University of Tsukuba for their technical assistance.
Funding
This work was supported in part by a Grant-in-Aid for Scientific Research KAKENHI from the Ministry of Education, Culture, Sports, Science, and Technology, Japan (19H03995) and MEXT Leading Initiative for Excellent Young Researchers Grant Number JPMXS0320200234. MY and MM were recipients of a Grant-in-Aid for Research Fellowships of Japan Society for the Promotion of Science for Young Scientists (21J10316, 20J20892).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yoshioka, M., Kosaki, K., Matsui, M. et al. Association of circulating calciprotein particle levels with skeletal muscle mass and strength in middle-aged and older adults. Hypertens Res 45, 900–910 (2022). https://doi.org/10.1038/s41440-022-00870-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00870-y