Abstract
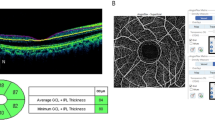
Malignant hypertension, a form of hypertensive emergency, causes acute damage in vital organs such as the brain, eyes, and kidneys. We aimed to examine the concurrency of acute hypertensive damage across the target organs to elucidate the underlying analogous pathophysiology. This single-center retrospective study evaluated the characteristics of organ damage, short-term clinical course, and interorgan relationships in patients with malignant hypertension treated between 2008 and 2019. Baseline characteristics of 20 patients who met our inclusion criteria were mean age 48 ± 13 years and blood pressure 222 ± 18/142 ± 16 mmHg; the median estimated glomerular filtration rate and urinary protein level were 49 mL/min/1.73 m2 (interquartile range [IQR] 27–79) and 1.9 g/g creatinine (IQR 0.2–4.0), respectively. Posterior reversible encephalopathy syndrome (PRES) was found in 60% of patients with major involvement and a wide variety of distribution patterns in the brainstem. In the fundus, serous retinal detachment was found in 60% of patients. Patients with PRES and serous retinal detachment showed higher levels of urinary protein than those without symptoms (P = 0.007 and 0.02, respectively), and proteinuria >1 g/g creatinine highly complicated both PRES and serous retinal detachment (91%). Matrix analysis also showed that the three symptoms were highly associated with each other. These results demonstrate the close relationship and concurrency of hypertensive acute organ damage in the brain, eyes, and kidneys. A common analogous mechanism, such as hyperperfusion-induced capillary leakage in each organ, implies an underlying pathophysiology of PRES, serous retinal detachment, and proteinuria.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, et al. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30:463–6.
Kitiyakara C, Guzman NJ. Malignant hypertension and hypertensive emergencies. J Am Soc Nephrol. 1998;9:133–42.
Peixoto AJ. Acute severe hypertension. N. Engl J Med. 2019;381:1843–52.
Rubin S, Cremer A, Boulestreau R, Rigothier C, Kuntz S, Gosse P. Malignant hypertension: diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J Hypertens. 2019;37:316–24.
Gonzalez R, Morales E, Segura J, Ruilope LM, Praga M. Long-term renal survival in malignant hypertension. Nephrol Dial Transpl. 2010;25:3266–72.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Healton EB, Brust JC, Feinfeld DA, Thomson GE. Hypertensive encephalopathy and the neurologic manifestations of malignant hypertension. Neurology. 1982;32:127–32.
Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008;29:1036–42.
Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015;14:914–25.
Nagayama Y, Inoue Y, Inui K, Yoshimura A. Comparison of renal outcome among japanese patients with or without microangiopathic hemolysis in malignant phase hypertension: a single-center retrospective study. Nephron. 2017;137:197–204.
Hayreh SS, Servais GE, Virdi PS. Fundus lesions in malignant hypertension. VI. Hypertensive choroidopathy. Ophthalmology. 1986;93:1383–400.
Lee CS, Choi EY, Lee M, Kim H, Chung H. Serous retinal detachment in preeclampsia and malignant hypertension. Eye (Lond). 2019;33:1707–14.
van den Born BJ, Honnebier UP, Koopmans RP, van Montfrans GA. Microangiopathic hemolysis and renal failure in malignant hypertension. Hypertension. 2005;45:246–51.
Ito S. Cardiorenal syndrome: an evolutionary point of view. Hypertension. 2012;60:589–95.
Ito S, Nagasawa T, Abe M, Mori T. Strain vessel hypothesis: a viewpoint for linkage of albuminuria and cerebro-cardiovascular risk. Hypertens Res. 2009;32:115–21.
Nagasawa T, Mori T, Ohsaki Y, Yoneki Y, Guo Q, Sato E, et al. Albuminuria indicates the pressure-associated injury of juxtamedullary nephrons and cerebral strain vessels in spontaneously hypertensive stroke-prone rats. Hypertens Res. 2012;35:1024–31.
Rizzoni D, Rizzoni M, Nardin M, Chiarini G, Agabiti-Rosei C, Aggiusti C, et al. Vascular aging and disease of the small vessels. High Blood Press Cardiovasc Prev. 2019;26:183–9.
Wong TY, Mitchell P. The eye in hypertension. Lancet. 2007;369:425–35.
Aguilar MI, O’Meara ES, Seliger S, Longstreth WT Jr., Hart RG, Pergola PE, et al. Albuminuria and the risk of incident stroke and stroke types in older adults. Neurology. 2010;75:1343–50.
Wong CW, Wong TY, Cheng CY, Sabanayagam C. Kidney and eye diseases: common risk factors, etiological mechanisms, and pathways. Kidney Int. 2014;85:1290–302.
Chua J, Chin CWL, Hong J, Chee ML, Le TT, Ting DSW, et al. Impact of hypertension on retinal capillary microvasculature using optical coherence tomographic angiography. J Hypertens. 2019;37:572–80.
Tamura K, Maeda A, Uneda K, Wakui H, Dejima T, Mitsuhashi H, et al. An increase in perfusion pressure and activation of the renin-angiotensin system in the pathogenesis of hypertension and injury: strain vessels and the cerebrovascular-renal connection. Hypertens Res. 2012;35:972–4.
Imai E, Horio M, Nitta K, Yamagata K, Iseki K, Hara S, et al. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin Exp Nephrol. 2007;11:41–50.
Morimoto R, Ono Y, Tezuka Y, Kudo M, Yamamoto S, Arai T, et al. Rapid screening of primary aldosteronism by a novel chemiluminescent immunoassay. Hypertension. 2017;70:334–41.
Tamaki Y, Araie M, Kawamoto E, Eguchi S, Fujii H. Non-contact, two-dimensional measurement of tissue circulation in choroid and optic nerve head using laser speckle phenomenon. Exp Eye Res. 1995;60:373–83.
Isono H, Kishi S, Kimura Y, Hagiwara N, Konishi N, Fujii H. Observation of choroidal circulation using index of erythrocytic velocity. Arch Ophthalmol. 2003;121:225–31.
Kunikata H, Nakazawa T. Recent clinical applications of laser speckle flowgraphy in eyes with retinal disease. Asia Pac J Ophthalmol (Philos). 2016;5:151–8.
Iadecola C, Davisson RL. Hypertension and cerebrovascular dysfunction. Cell Metab. 2008;7:476–84.
Feske SK. Posterior reversible encephalopathy syndrome: a review. Semin Neurol. 2011;31:202–15.
Bidani AK, Griffin KA. Pathophysiology of hypertensive renal damage: implications for therapy. Hypertension. 2004;44:595–601.
Sanerkin NG. Vascular lesions of malignant essential hypertension. J Pathol. 1971;103:177–84.
Delaey C, Van De, Voorde J. Regulatory mechanisms in the retinal and choroidal circulation. Ophthalmic Res. 2000;32:249–56.
Kiel JW, Shepherd AP. Autoregulation of choroidal blood flow in the rabbit. Invest Ophthalmol Vis Sci. 1992;33:2399–410.
Mishima E, Hashimoto J, Akiyama Y, Seiji K, Takase K, Abe T, et al. Posterior reversible encephalopathy syndrome treated with renin-angiotensin system blockade. J Neurol Sci. 2015;355:219–21.
Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc. 2010;85:427–32.
Gao B, Lv C. Central-variant posterior reversible encephalopathy syndrome: more than meets the eye. AJR Am J Roentgenol. 2014;203:W454.
Ho CM, Chan KH. Posterior reversible encephalopathy syndrome with vasospasm in a postpartum woman after postdural puncture headache following spinal anesthesia. Anesth Analg. 2007;105:770–2.
Pilato F, Distefano M, Calandrelli R. Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome: clinical and radiological considerations. Front Neurol. 2020;11:34.
Dewilde E, Huygens M, Cools G, Van Calster J. Hypertensive choroidopathy in pre-eclampsia: two consecutive cases. Ophthalmic Surg Lasers Imaging Retin. 2014;45:343–6.
Bourke K, Patel MR, Prisant LM, Marcus DM. Hypertensive choroidopathy. J Clin Hypertens (Greenwich). 2004;6:471–2.
Saito M, Noda K, Saito W, Hirooka K, Hashimoto Y, Ishida S. Increased choroidal blood flow and choroidal thickness in patients with hypertensive chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2020;258:233–40.
Paronetto F. Immunocytochemical observations on the vascular necrosis and renal glomerular lesions of malignant nephrosclerosis. Am J Pathol. 1965;46:901–15.
Iwasaki T, Mishima E, Suzuki T, Kikuchi K, Toyohara T, Seiji K, et al. Kidney enlargement effect of angioplasty for nonatherosclerotic renovascular disease: reversibility of ischemic kidney. Hypertens Res. 2020. https://doi.org/10.1038/s41440-020-0473-6.
Hayreh SS, Servais GE, Virdi PS. Cotton-wool spots (inner retinal ischemic spots) in malignant arterial hypertension. Ophthalmologica. 1989;198:197–215.
Henderson AD, Bruce BB, Newman NJ, Biousse V. Hypertension-related eye abnormalities and the risk of stroke. Rev Neurol Dis. 2011;8:1–9.
Acknowledgements
We thank Y. Sasaki for technical assistance. This work is partially supported by the Tohoku University Center for Gender Equality Promotion (TUMUG) Support Project and a grant from the Japan Foundation for Applied Enzymology.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mishima, E., Funayama, Y., Suzuki, T. et al. Concurrent analogous organ damage in the brain, eyes, and kidneys in malignant hypertension: reversible encephalopathy, serous retinal detachment, and proteinuria. Hypertens Res 44, 88–97 (2021). https://doi.org/10.1038/s41440-020-0521-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-0521-2
Keywords
This article is cited by
-
Impact of early initiation of renin-angiotensin blockade on renal function and clinical outcomes in patients with hypertensive emergency: a retrospective cohort study
BMC Nephrology (2023)
-
Genetic, clinical, and pathological study of patients with severe hypertension-associated renal microangiopathy
Journal of Nephrology (2023)
-
Hypertensive eye disease
Nature Reviews Disease Primers (2022)
-
What is the impact of blood pressure on neurological symptoms and the risk of ESKD in primary and secondary thrombotic microangiopathies based on clinical presentation: a retrospective study
BMC Nephrology (2022)
-
Potential common pathophysiological pathway of hypertension-mediated organ damage in hypertensive emergency
Hypertension Research (2021)