Abstract
The use of artificial intelligence in numerous prediction and classification tasks, including clinical research and healthcare management, is becoming increasingly more common. This review describes the current status and a future possibility for artificial intelligence in blood pressure management, that is, the possibility of accurately predicting and estimating blood pressure using large-scale data, such as personal health records and electronic medical records. Individual blood pressure continuously changes because of lifestyle habits and the environment. This review focuses on two topics regarding controlling changing blood pressure: a novel blood pressure measurement system and blood pressure analysis using artificial intelligence. Regarding the novel blood pressure measurement system, we compare the conventional cuff-less method with the analysis of pulse waves using artificial intelligence for blood pressure estimation. Then, we describe the prediction of future blood pressure values using machine learning and deep learning. In addition, we summarize factor analysis using “explainable AI” to solve a black-box problem of artificial intelligence. Overall, we show that artificial intelligence is advantageous for hypertension management and can be used to establish clinical evidence for the practical management of hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lecun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–444.
Karras T, Laine S, Aila T. A style-based generator architecture for generative adversarial networks. In: Proceedings of the IEEE Computer Society Conference on Computer Vision and Pattern Recognition. 2019;4396–4405. https://doi.org/10.1109/CVPR.2019.00453.
Devlin J, Chang M-W, Lee K, Toutanova K. BERT: pre-training of deep bidirectional transformers for language understanding. arXiv:1810.04805 [cs.CL]. 2018.
McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova N, Ashrafian H, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577:89–94.
Hannun AY, Rajpurkar P, Haghpanahi M, Tison GH, Bourn C, Turakhia MP, et al. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat Med. 2019;25:65–69. https://doi.org/10.1038/s41591-018-0268-3.
Attia ZI, Noseworthy PA, Lopez-Jimenez F, Asirvatham SJ, Deshmukh AJ, Gersh BJ, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet. 2019;394:861–867.
Hinton G. Deep learning-a technology with the potential to transform health care. JAMA. 2018;320:1101–1102. https://doi.org/10.1001/jama.2018.11100.
Shortliffe EH, Sepúlveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018;320:2199–2200.
Beam AL, Kohane IS. Big data and machine learning in health care. JAMA. 2018;319:1317–1318.
Park SH, Han K. Methodologic guide for evaluating clinical performance and effect of artificial intelligence technology for medical diagnosis and prediction. Radiology. 2018;286:800–809.
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2:230–243.
Santhanam P, Ahima RS. Machine learning and blood pressure. J Clin Hypertens. 2019;21:1735–1737.
Fujiyoshi A, Ohkubo T, Miura K, Murakami Y, Nagasawa SY, Okamura T, et al. Blood pressure categories and long-term risk of cardiovascular disease according to age group in Japanese men and women. Hypertens Res. 2012;35:947–953.
Yusuf S, Thom T, Abbott RD. Changes in hypertension treatment and in congestive heart failure mortality in the united states. Hypertension. 1989;13:I-74–I–79.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–1481.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71:e127–e248.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104.
Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis. Hypertension. 2008;52:1045–1050.
Hanazawa T, Asayama K, Watabe D, Tanabe A, Satoh M, Inoue R, et al. Association between amplitude of seasonal variation in self-measured home blood pressure and cardiovascular outcomes: HOMED-BP (Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure) study. J Am Heart Assoc. 2018;7. https://doi.org/10.1161/JAHA.117.008509.
Wang J, Shi X, Ma C, Zheng H, Xiao J, Bian H, et al. Visit-to-visit blood pressure variability is a risk factor for all-cause mortality and cardiovascular disease: a systematic review and meta-analysis. J Hypertens. 2017;35:10–17.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. N. Engl J Med. 1997;336:1117–1124.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). J Am Med Assoc. 1998;279:839–846.
Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. Exercise and hypertension. Med Sci Sports Exerc. 2004;36:533–553. https://doi.org/10.1249/01.MSS.0000115224.88514.3A.
Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ. The effect of temperature on systolic blood pressure. Blood Press Monit. 2007;12:195–203.
Nagele E, Jeitler K, Horvath K, Semlitsch T, Posch N, Herrmann KH, et al. Clinical effectiveness of stress-reduction techniques in patients with hypertension: systematic reviewand meta-analysis. J Hypertens. 2014;32:1936–1944.
Xu Y, Zhang W, Wang D, Ping P. A calibration method for cuffless continue blood pressure measurement using Gaussian normalized pulse transit time. In: I2MTC 2018—2018 IEEE International Instrumentation and Measurement Technology Conference: Discovering New Horizons in Instrumentation and Measurement, Proceedings. Institute of Electrical and Electronics Engineers Inc., 2018;1–5. https://doi.org/10.1109/I2MTC.2018.8409817.
Bhattacharya T, Gupta A, Singh ST, Roy S, Prasad A. Robust motion artefact resistant circuit for calculation of Mean Arterial Pressure from pulse transit time. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS. Institute of Electrical and Electronics Engineers Inc., 2017, 3553–3556. https://doi.org/10.1109/EMBC.2017.8037624.
Van Velzen MHN, Loeve AJ, Niehof SP, Mik EG. Increasing accuracy of pulse transit time measurements by automated elimination of distorted photoplethysmography waves. Med Biol Eng Comput. 2017;55:1989–2000.
Rosenberger ME, Buman MP, Haskell WL, McConnell MV, Carstensen LL. Twenty-four Hours of Sleep, Sedentary Behavior, and Physical Activity with Nine Wearable Devices. Med Sci Sports Exerc. 2016;48:457–465.
Moon EW, Tan NC, Allen JC, Jafar TH. The use of wireless, smartphone app–assisted home blood pressure monitoring among hypertensive patients in Singapore: pilot randomized controlled trial. JMIR mHealth uHealth. 2019;7:2366–2370.
Werbos PJ. Backpropagation through time: what it does and how to do it. Proc IEEE. 1990;78:1550–1560.
Hochreiter S, Schmidhuber J. Long short-term memory. Neural Comput. 1997;9:1735–1780.
Wang Z, Yan W, Oates T. Time series classification from scratch with deep neural networks: A strong baseline. In: Proceedings of the International Joint Conference on Neural Networks. Institute of Electrical and Electronics Engineers Inc., 2017, 1578–1585. https://doi.org/10.1109/IJCNN.2017.7966039.
Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N. Engl J Med. 2019;381:1909–1917.
Ólafsdóttir AF, Attvall S, Sandgren U, Dahlqvist S, Pivodic A, Skrtic S, et al. A clinical trial of the accuracy and treatment experience of the flash glucose monitor freestyle libre in adults with type 1 diabetes. Diabetes Technol Ther. 2017;19:164–172.
Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘anticipation medicine’ for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262–281.
Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of a wrist-type home nocturnal blood pressure monitor in the sitting and supine position according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-9600T. J Clin Hypertens. 2019;21:463–469.
Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2:2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens. 2019;21:853–858.
Association for the Advancement of Medical Instrumentation American National Standard. ANSI/AAMI/ISO 81060-2:2013 non-invasive sphygmomanometers—part 2: clinical investigation of automated measurement type. 2013. www.aami.org. Accessed 10 Mar 2020.
Mukkamala R, Hahn JO, Inan OT, Mestha LK, Kim CS, Toreyin H, et al. Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans Biomed Eng. 2015;62:1879–1901.
Sharma M, Barbosa K, Ho V, Griggs D, Ghirmai T, Krishnan S, et al. Cuff-less and continuous blood pressure monitoring: a methodological review. Technologies. 2017;5:21.
Monte-Moreno E. Non-invasive estimate of blood glucose and blood pressure from a photoplethysmograph by means of machine learning techniques. Artif Intell Med. 2011;53:127–138.
O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: Recommendations of the European Society of Hypertension. Br Med J. 2001;322:531–536.
Ruiz-Rodríguez JC, Ruiz-Sanmartín A, Ribas V, Caballero J, García-Roche A, Riera J, et al. Innovative continuous non-invasive cuffless blood pressure monitoring based on photoplethysmography technology. Intensive Care Med. 2013;39:1618–1625.
Sideris C, Kalantarian H, Nemati E, Sarrafzadeh M. Building Continuous Arterial Blood Pressure Prediction Models Using Recurrent Networks. In: 2016 IEEE International Conference on Smart Computing, SMARTCOMP 2016. Institute of Electrical and Electronics Engineers Inc., 2016. https://doi.org/10.1109/SMARTCOMP.2016.7501681.
Su P, Ding XR, Zhang YT, Liu J, Miao F, Zhao N. Long-term blood pressure prediction with deep recurrent neural networks. In: 2018 IEEE EMBS International Conference on Biomedical and Health Informatics, BHI 2018. Institute of Electrical and Electronics Engineers Inc., 2018, 323–328. https://doi.org/10.1109/BHI.2018.8333434.
Moody GB, Mark RG. A database to support development and evaluation of intelligent intensive care monitoring. In: Computers in Cardiology. IEEE, 1996, 657–660. https://doi.org/10.1109/cic.1996.542622.
Shimazaki S, Bhuiyan S, Kawanaka H, Oguri K. Features Extraction for Cuffless Blood Pressure Estimation by Autoencoder from Photoplethysmography. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS. Institute of Electrical and Electronics Engineers Inc., 2018, 2857–2860. https://doi.org/10.1109/EMBC.2018.8512829.
Hinton GE, Salakhutdinov RR. Reducing the dimensionality of data with neural networks. Science. 2006;313:504–507.
Yan C, Li Z, Zhao W, Hu J, Jia D, Wang H, et al. Novel Deep Convolutional Neural Network for Cuff-less Blood Pressure Measurement Using ECG and PPG Signals. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS. Institute of Electrical and Electronics Engineers Inc., 2019, 1917–1920. https://doi.org/10.1109/EMBC.2019.8857108p.
Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation 2000;101. https://doi.org/10.1161/01.cir.101.23.e215.
Mohebbian MR, Dinh A, Wahid K, Alam MS. Blind, cuff-less, calibration-free and continuous blood pressure estimation using optimized inductive group method of data handling. Biomed Signal Process Control. 2020;57:101682.
Schmidhuber J. Deep learning in neural networks: an overview. Neural Netw 2015;61:85–117. https://doi.org/10.1016/j.neunet.2014.09.003.
Kario K, Shimbo D, Tomitani N, Kanegae H, Schwartz JE, Williams B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens. 2020;22:135–141.
Watanabe N, Bando YK, Kawachi T, Yamakita H, Futatsuyama K, Honda Y, et al. Development and validation of a novel cuff-less blood pressure monitoring device. JACC Basic Transl Sci. 2017;2:631–642.
Coravos A, Khozin S, Mandl KD. Developing and adopting safe and effective digital biomarkers to improve patient outcomes. npj Digit Med. 2019;2:1–5.
Hirata T, Nakamura T, Kogure M, Tsuchiya N, Narita A, Miyagawa K, et al. Reduced sleep efficiency, measured using an objective device, was related to an increased prevalence of home hypertension in Japanese adults. Hypertens Res. 2020;43:23–29.
Iwahori T, Miura K, Ueshima H. Time to consider use of the sodium-to-potassium ratio for practical sodium reduction and potassium increase. Nutrients. 2017;9. https://doi.org/10.3390/nu9070700.
Huang S, Xu Y, Yue L, Wei S, Liu L, Gan X, et al. Evaluating the risk of hypertension using an artificial neural network method in rural residents over the age of 35 years in a Chinese area. Hypertens Res. 2010;33:722–726.
Völzke H, Fung G, Ittermann T, Yu S, Baumeister SE, Dörr M, et al. A new, accurate predictive model for incident hypertension. J Hypertens. 2013;31:2142–2150.
Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: The Framingham Heart Study. Ann Intern Med. 2008;148:102–110.
Golino HF, de Amaral LSB, Duarte SFP, Gomes CMA, de Soares TJ, Dos Reis LA, et al. Predicting Increased Blood Pressure Using Machine Learning. J Obes. 2014;2014:1–12.
Li X, Wu S, Wang L. Blood Pressure Prediction via Recurrent Models with Contextual Layer. In: Proceedings of the 26th International Conference on World Wide Web - WWW ’17. New York, New York, USA: ACM Press, 2017, 685–693. https://doi.org/10.1145/3038912.3052604.
Kwong EWY, Wu H, Pang GK-H. A prediction model of blood pressure for telemedicine. Health Inform J. 2018;24:227–244.
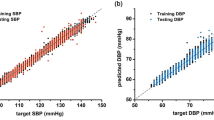
Koshimizu H, Kojima R, Kario K, Okuno Y. Prediction of blood pressure variability using deep neural networks. Int J Med Inf. 2020;136:104067.
Ribeiro MT, Singh S, Guestrin C. ‘Why should i trust you?’ Explaining the predictions of any classifier. In: Proceedings of the ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. New York, New York, USA: Association for Computing Machinery, 2016, 1135–1144. https://doi.org/10.1145/2939672.2939778.
Sundararajan M, Taly A, Yan Q. Axiomatic attribution for deep networks. Proceedings of the 34th International Conference on Machine Learning. 2017;7:5109–5118.
Lundberg SM, Lee SI. A unified approach to interpreting model predictions. In: Advances in Neural Information Processing Systems. 2017, 4766–4775. https://github.com/slundberg/shap. Accessed 14 Mar 2020.
Chiang P-H, Dey S. Personalized Effect of Health Behavior on Blood Pressure: Machine Learning Based Prediction and Recommendation. In 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom). IEEE, 2018, 1–6. https://doi.org/10.1109/HealthCom.2018.8531109.
Elshawi R, Al-Mallah MH, Sakr S. On the interpretability of machine learning-based model for predicting hypertension. BMC Med Inf Decis Mak. 2019;19:146.
Guthrie NL, Carpenter J, Edwards KL, Appelbaum KJ, Dey S, Eisenberg DM, et al. Emergence of digital biomarkers to predict and modify treatment efficacy: machine learning study. BMJ Open. 2019;9:e030710.
Lundberg SM, Nair B, Vavilala MS, Horibe M, Eisses MJ, Adams T, et al. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng. 2018;2:749–760.
Acknowledgements
Hiroshi Koshimizu would like to express my gratitude to Omron Healthcare Co., Ltd. for giving me the time to complete this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Employment: HK (Omron Healthcare Co., Ltd.), None: RK, YO.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koshimizu, H., Kojima, R. & Okuno, Y. Future possibilities for artificial intelligence in the practical management of hypertension. Hypertens Res 43, 1327–1337 (2020). https://doi.org/10.1038/s41440-020-0498-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-0498-x
Keywords
This article is cited by
-
Artificial intelligence in disease diagnosis: a systematic literature review, synthesizing framework and future research agenda
Journal of Ambient Intelligence and Humanized Computing (2023)
-
A deep learning MRI-based signature may provide risk-stratification strategies for nasopharyngeal carcinoma
European Archives of Oto-Rhino-Laryngology (2023)
-
Noninvasive method to validate the variability of blood pressure during arrhythmias
Hypertension Research (2022)
-
Continuous cuffless monitoring of arterial blood pressure via graphene bioimpedance tattoos
Nature Nanotechnology (2022)