Abstract
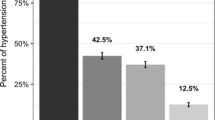
Antihypertensive drugs remain one of the main beneficial strategies for cardiovascular disease prevention. The objective of our study was to investigate the associations of different clinical and socioeconomic (SES) factors, and the use of primary care medicine with treatment and adherence (proportion of days covered (PDC) by treatment) to hypertension management in French participants aware of their hypertension. Cross-sectional analyses of treatment for hypertension and adherence to treatment were performed using data from 396 participants from the ESTEBAN survey, a representative sample of the French population. Logistic regression analyses were performed to investigate associations between SES factors (age, sex, education, income, civil status), clinical factors, health care (general practitioner (GP) visits, cardiologist visits, number of consultations, home blood pressure measurement (HBPM)), treatment and adherence. A total of 265 of the 396 hypertensive patients were treated. Antihypertensive drug use was more common among elderly individuals (OR: 2.73 [1.14; 4.32), diabetic patients (OR: 4.18 [1.92; 6.44] and overweight hypertensive patients (OR = 3.04 [1.09; 4.99]). GP consultations and HBPM were associated with increased treatment (OR: 1.03 [1.01; 1.05]; OR: 1.97 [1.06; 2.61], respectively). The PDC was higher among men (p = 0.045) and couples living together (p = 0.018) but lower among diabetic patients (p = 0.012) and patients visiting a cardiologist (p = 0.008). Education and income levels were not associated with either treatment or the PDC. In France, SES factors seemed to have little impact on treatment and adherence to antihypertensive drug regimens. However, treatment administered by GPs and HBPM may play key roles in hypertension management. Although the PDC was quite low, both the number of GP consultations and HBPM were positively associated with pharmacological treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lim GB. Global burden of cardiovascular disease. Nat Rev Cardiol. 2013;10:59 https://doi.org/10.1038/nrcardio.2012.194
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43:10–17. https://doi.org/10.1161/01.HYP.0000103630.72812.10
Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62:218–25. https://doi.org/10.1161/HYPERTENSIONAHA.113.00687
Ninomiya T, Perkovic V, Turnbull F, Neal B, Barzi F, Cass A. Blood Pressure Lowering Treatment Trialists’ Collaboration et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ. 2013;347:f5680. https://doi.org/10.1136/bmj.f5680.
Ishisaka DY, Jukes T, Romanelli RJ, Wong KS, Schiro TA. Disparities in adherence to and persistence with antihypertensive regimens: an exploratory analysis from a community-based provider network. J Am Soc Hypertens. 2012;6:201–9. https://doi.org/10.1016/j.jash.2012.02.004
Lagu T, Weiner MG, Eachus S, Tang SSK, Schwartz JS, Turner BJ. Effect of patient comorbidities on filling of antihypertensive prescriptions. Am J Manag Care. 2009;15:24–30.
Wamala S, Merlo J, Bostrom G, Hogstedt C, Agren G. Socioeconomic disadvantage and primary non-adherence with medication in Sweden. Int J Qual Health Care J Int Soc Qual Health Care. 2007;19:134–40. https://doi.org/10.1093/intqhc/mzm011
Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK, Andersson Sundell K, Petzold M, et al. Adherence to antihypertensive therapy and elevated blood pressure: should we consider the use of multiple medications? PloS One. 2015;10:e0137451 https://doi.org/10.1371/journal.pone.0137451
Wettermark B, Hammar N, Fored CM, MichaelFored C, Leimanis A, Otterblad Olausson P, et al. The new Swedish Prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16:726–35. https://doi.org/10.1002/pds.1294
Balicco A, Oleko A, Boschat L, Deschamps V, Saoudi A, Zeghnoun A, et al. Esteban design: a cross-sectional health survey about environment, biomonitoring, physical activity and nutrition (2014-2016). Toxicologie Analytique Clin. 2017;29:517–37. https://doi.org/10.1016/j.toxac.2017.06.003
Vallée A, Gabet A, Deschamps V, Blacher J, Olié V. Relationship between nutrition and alcohol consumption with blood pressure: the ESTEBAN survey. Nutrients. 2019; 11. https://doi.org/10.3390/nu11061433
Vallée A, Perrine A-L, Deschamps V, Blacher J, Olié V. Relationship between dynamic changes in body weight and blood pressure: the ESTEBAN survey. Am J Hypertens. https://doi.org/10.1093/ajh/hpz096.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. List of authors/Task Force members: 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2018;36:2284–309. https://doi.org/10.1097/HJH.0000000000001961
Choudhry NK, Shrank WH, Levin RL, Lee JL, Jan SA, Brookhart MA, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15:457–64.
Schneider S The International Standard Classification of Education 2011. Emerald Group Publishing Limited. Birkelund GE, editor
Satoh A, Arima H, Ohkubo T, Nishi N, Okuda N, Ae R, et al. NIPPON DATA2010 Research Group. Associations of socioeconomic status with prevalence, awareness, treatment, and control of hypertension in a general Japanese population: NIPPON DATA2010. J Hypertens. 2017;35:401–8. https://doi.org/10.1097/HJH.0000000000001169
Nguyen QC, Waddell EN, Thomas JC, Huston SL, Kerker BD, Gwynn RC. Awareness, treatment, and control of hypertension and hypercholesterolemia among insured residents of New York City, 2004. Prev Chronic Dis. 2011;8:A109.
Egan BM, Sutherland SE, Rakotz M, Yang J, Hanlin RB, Davis RA, et al. Improving Hypertension Control in Primary Care With the Measure Accurately, Act Rapidly, and Partner With Patients Protocol. Hypertension. 2018;72:1320–7. https://doi.org/10.1161/HYPERTENSIONAHA.118.11558
Fang J, Yang Q, Ayala C, Loustalot F. Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens. 2014;27:1377–86. https://doi.org/10.1093/ajh/hpu061
Di Chiara T, Scaglione A, Corrao S, Argano C, Pinto A, Scaglione R. Education and hypertension: impact on global cardiovascular risk. Acta Cardiol. 2017;72:507–13. https://doi.org/10.1080/00015385.2017.1297626
de Gaudemaris R, Lang T, Chatellier G, Larabi L, Lauwers-Cancès V, Maître A, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension. 2002;39:1119–25. https://doi.org/10.1161/01.hyp.0000018912.05345.55
McManus RJ, Mant J, Roalfe A, Oakes RA, Bryan S, Pattison HM, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. BMJ. 2005;331:493 https://doi.org/10.1136/bmj.38558.393669.E0
McGrath BP. Home monitoring of blood pressure. Aust Prescr. 2015;38:16–19. https://doi.org/10.18773/austprescr.2015.005
Hamilton GA. Measuring adherence in a hypertension clinical trial. Eur J Cardiovasc Nurs J Work Group Cardiovasc Nurs Eur Soc Cardiol. 2003;2:219–28. https://doi.org/10.1016/S1474-5151(03)00058-6
Mennini FS, Marcellusi A, von der Schulenburg JMG, Gray A, Levy P, Sciattella P, et al. Cost of poor adherence to anti-hypertensive therapy in five European countries. Eur J Health Econ HEPAC Health Econ Prev Care. 2015;16:65–72. https://doi.org/10.1007/s10198-013-0554-4
Lefort M, Neufcourt L, Pannier B, Vaïsse B, Bayat S, Grimaud O, et al. Sex differences in adherence to antihypertensive treatment in patients aged above 55: The French League Against Hypertension Survey (FLAHS). J Clin Hypertens. 2018;20:1496–503. https://doi.org/10.1111/jch.13387
Corrao G, Zambon A, Parodi A, Mezzanzanica M, Merlino L, Cesana G, et al. Do socioeconomic disparities affect accessing and keeping antihypertensive drug therapy? Evidence from an Italian population-based study. J Hum Hypertens. 2009;23:238–44. https://doi.org/10.1038/jhh.2008.84
Alsabbagh MHDW, Lemstra M, Eurich D, Lix LM, Wilson TW, Watson E, et al. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2014;17:288–96. https://doi.org/10.1016/j.jval.2013.11.011
Van Wijk BL, Klungel OH, Heerdink ER, de Boer A. Rate and determinants of 10-year persistence with antihypertensive drugs. J Hypertens. 2005;23:2101–7.
Braverman J, Dedier J. Predictors of medication adherence for African American patients diagnosed with hypertension. Ethn Dis. 2009;19:396–400.
Cho S-J, Kim J. Factors associated with nonadherence to antihypertensive medication. Nurs Health Sci. 2014;16:461–7. https://doi.org/10.1111/nhs.12145
Leenen FHH, Coletta E. Pharmacokinetic and antihypertensive profile of amlodipine and felodipine-ER in younger versus older patients with hypertension. J Cardiovasc Pharm. 2010;56:669–75. https://doi.org/10.1097/FJC.0b013e3181fc45bb
Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ Couns. 2016;99:1079–86. https://doi.org/10.1016/j.pec.2016.01.020
Hyman DJ, Pavlik V. Medication adherence and resistant hypertension. J Hum Hypertens. 2015;29:213–8. https://doi.org/10.1038/jhh.2014.73
Coons SJ. Medication compliance: the search for answers continues. Clin Ther. 2001;23:1294–5. https://doi.org/10.1016/s0149-2918(01)80108-9
Uchmanowicz B, Chudiak A, Uchmanowicz I, Rosińczuk J, Froelicher ES. Factors influencing adherence to treatment in older adults with hypertension. Clin Inter Aging. 2018;13:2425–41. https://doi.org/10.2147/CIA.S182881
Nishimura S, Kumamaru H, Shoji S, Sawano M, Kohsaka S, Miyata H. Adherence to antihypertensive medication and its predictors among non-elderly adults in Japan. Hypertens Res. 2020;43:705–14. https://doi.org/10.1038/s41440-020-0440-2
Lebeau J-P, Cadwallader J-S, Aubin-Auger I, Mercier A, Pasquet T, Rusch E, et al. The concept and definition of therapeutic inertia in hypertension in primary care: a qualitative systematic review. BMC Fam Pr. 2014;15:130 https://doi.org/10.1186/1471-2296-15-130
Vallée A, Gabet A, Grave C, Sorbets E, Blacher J, Olié V. Patterns of hypertension management in France in 2015: The ESTEBAN survey. J Clin Hypertens. 2020. https://doi.org/10.1111/jch.13834.
Burnier M, Egan BM. Adherence in hypertension. Circ Res. 2019;124:1124–40. https://doi.org/10.1161/CIRCRESAHA.118.313220
Burnier M. Drug adherence in hypertension. Pharm Res. 2017;125:142–9. https://doi.org/10.1016/j.phrs.2017.08.015
Colantonio LD, Rosenson RS, Deng L, Monda KL, Dai Y, Farkouh ME, et al. Adherence to statin therapy among US adults between 2007 and 2014. J Am Heart Assoc. 2019;8:e010376 https://doi.org/10.1161/JAHA.118.010376
Nielsen SF, Nordestgaard BG. Negative statin-related news stories decrease statin persistence and increase myocardial infarction and cardiovascular mortality: a nationwide prospective cohort study. Eur Heart J. 2016;37:908–16. https://doi.org/10.1093/eurheartj/ehv641
Smith SC. Adherence to medical therapy and the global burden of cardiovascular disease. J Am Coll Cardiol. 2016;67:1516–8. https://doi.org/10.1016/j.jacc.2016.02.016
Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. 2018;34:575–84. https://doi.org/10.1016/j.cjca.2017.12.005
Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care. 2003;26:1408–12. https://doi.org/10.2337/diacare.26.5.1408
Acknowledgements
The authors thank the Centers for Health Examinations, the Cetaf and the laboratories involved in the data collection, as well as the entire ESTEBAN team and study participants. The ESTEBAN study, part of the National Biosafety initiative, is financed by the Ministry of Solidarities and Health and the Ministry of Ecological and Solidarity Transition. The authors thank Jeffrey Arsham for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AV, CG, AG and VO have no conflicts of interest. Outside of this work, JB has received research support or has served on advisory boards or as a speaker for Abbott, Amgen, Astellas, Astra-Zeneca, Bayer, Boehringer, Ingelheim, Bouchara-Recordati, Daiichi Sankyo, Ferring, Gilead, Icomed, Medexact, Medtronic, Novartis, Novo Nordisk, Quantum Genomics, Saint Jude, Sanofi Aventis, and Servier.
Ethic approval
All procedures performed in studies involving human participants were in accordance with the ethics standards of the institutional and/or national research committee and with the principles of the 1964 Helsinki declaration and its later amendments or comparable ethics standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
IRB approval
The study was registered with the French National Agency for Medicines and Health Products Safety (No. 2012-A00456-34) and was approved by the Advisory Committee for Protection of Persons in Biomedical Research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vallée, A., Grave, C., Gabet, A. et al. Treatment and adherence to antihypertensive therapy in France: the roles of socioeconomic factors and primary care medicine in the ESTEBAN survey. Hypertens Res 44, 550–560 (2021). https://doi.org/10.1038/s41440-020-00603-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-00603-z
Keywords
This article is cited by
-
Sex differences in the association between socioeconomic status and untreated hypertension among residents with hypertension in rural Khánh Hòa, Vietnam: a post-hoc analysis
BMC Cardiovascular Disorders (2024)
-
Social determinants of hypertension in high-income countries: A narrative literature review and future directions
Hypertension Research (2022)
-
Improving patient adherence: the last obstacle to achieving hypertension control
Hypertension Research (2021)