Abstract
Compromised placentation strongly predisposes to preeclampsia (PE) which is a severe complication of pregnancy. Pregnancy-associated plasma protein-A2 (PAPP-A2) has higher expression in the placenta than in any other tissues. However, the possible role of PAPP-A2 in placental development and in the pathogenesis of PE remains unclear. In this study, we aimed at exploring placental expression of PAPP-A2 in early- and late-onset of severe PE and its role in the mechanism inducing the development of PE. We found that expression of PAPP-A2 mRNA and protein was elevated in placentas from women with severe PE compared to control placentas and was localized to differentiated trophoblasts; higher in early-onset PE than that in late-onset PE. PAPP-A2 was expressed in the cytoplasm of both primary trophoblasts and HTR-8/SVneo cells. Elevated PAPP-A2 attenuated migration, invasion, explant outgrowth and network formation of trophoblast cells in vitro without affecting cell proliferation and apoptosis. PAPP-A2 attenuated trophoblast invasion and migration by restraining epithelial–mesenchymal translations via downregulation of the Hedgehog signaling pathway. Overall, the increased expression of placental PAPP-A2 is specific to different period of PE onset and PAPP-A2 may contribute to poor placentation and inadequate angiogenesis thereby leading to the development of preeclampsia.
Similar content being viewed by others
Introduction
Preeclampsia (PE) is a severe disorder unique to human gestation that affects 2–8% of pregnancies and carries significant maternal–fetal morbidity and mortality [1, 2]. It is characterized by new onset of maternal hypertension and proteinuria after 20 weeks of gestation [3]. The pathogenesis of PE remains unclear, but it has been widely acknowledged that the condition originates from within the placenta [4]. While poor initial placentation strongly predisposes to early-onset preeclampsia (EOPE, <34 weeks’ gestation), late-onset preeclampsia (LOPE, 34 weeks’ onwards) is the condition largely associated with maternal cardiovascular or metabolic disorders [2, 5, 6]. Furthermore, delivery of the placenta (and fetus) remains the only curative recourse. Normal implantation involves invasion of trophoblasts into the endometrium. Inadequate trophoblast invasion into the maternal decidua coinciding with impaired spiral artery remodeling appears to be an early indication to a later progression in the development of PE [7].
Pregnancy-associated plasma protein-A2 (PAPP-A2, also known as pappalysin-2) was first identified in 2001 [8]. Its sequence of amino acid residues is 45% homologous with pregnancy-associated plasma protein-A (PAPP-A), and it is the only homolog of PAPP-A in the vertebrate genome [8, 9]. Together, these proteins make up the human pappalysin family [10]. Both are metzincin metalloproteases that specifically cleave insulin-like growth factor binding proteins (IGFBPs), resulting in local activation of insulin-like growth factors (IGFs) [11]. PAPP-A has been extensively studied for its biomarker roles in Down’s syndrome [12], yet the physiological and pathological functions of PAPP-A2 are largely unknown.
Placental and serum PAPP-A2 is significantly increased in preeclampsia, as well as in HELLP syndrome and fetal growth restriction [13,14,15,16]. However, there is not much information about the expression pattern of PAPP-A2 in different stages of preeclampsia. PAPP-A2 is highly associated with the IGF signaling pathway that appears involved in the etiology of PE [11, 17]. IGFBPs, along with the enzymatic modifiers, PAPPA, PAPP-A2 or ADAM (a disintegrin and metalloprotease), may contribute to the regulation of placental differentiation and growth via the IGF pathway [13]. PAPP-A2 is also indispensable for postnatal growth and bone development via its involvement to the IGF pathway [18,19,20,21]. In zebrafish embryos, PAPP-A2 modulates bone morphogenetic protein (Bmp) and notch signaling by independent mechanisms [9]. However, the mechanism for the effects of PAPP-A2 on extravillous trophoblast (EVT) invasion remains unclear.
In this study, we hypothesized that PAPP-A2 might play an important role during placentation. To date, the physiological and potential pathological functions of PAPP-A2 in normal and severe PE have not been clarified. Therefore, the aim of this study was to investigate the expression pattern of PAPPA2 in the placentas of EOPE and LOPE and to investigate the potential role of PAPP-A2 in angiogenesis and placentation and the underlying mechanism in PE.
Materials and methods
Participants and tissue collection
A total of 36 women with singleton pregnancies complicated by severe PE (18 EOPE and 18 LOPE) were enrolled. Gestational age-matched controls were 18 pregnant women with uncomplicated preterm deliveries for the EOPE group, and 18 healthy pregnancies without complications for the LOPE group. Severe PE was defined as systolic pressure >160 mmHg and/or diastolic blood pressure >110 mmHg on at least two occasions, with proteinuria (>5 g/24 h), oliguria <500 mL/24 h or multiorgan involvement such as pulmonary edema, abnormal liver function, right upper quadrant pain, thrombocytopenia or fetal growth restriction [22,23,24,25]. EOPE was defined as onset of PE at <34 weeks' gestation, and LOPE was from 34 weeks' onwards [26]. Placental tissue samples of PE and controls were obtained from each participant immediately after delivery and stored at −80 ℃ until processed. Placental tissue samples from early pregnancy (5–12 weeks’ gestation) were obtained from pregnancy termination and primary culture was performed immediately.
This study has been approved by the ethics committee at Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology (Wuhan, China). Each participant provided written informed consent.
Reverse transcription quantitative real-time polymerase chain reaction (RT-qPCR)
Total RNA was extracted from tissues using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s protocol. The cDNA was synthesized from total RNA using a reverse transcription kit (TaKaRa, Japan) and then stored at −20 °C until use. Quantification of transcripts was performed by a real-time PCR (Bio-Rad CFX96 system) using the SYBR Premix ExTaq Kit (TaKaRa, Japan). The PCR primers used were listed in Table 1. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used to normalize the data. All experiments were performed in triplicate.
Western blot assay
Cells and tissues were lysed in RIPA lysis buffer (Beyotiem, Shanghai, China) containing a protease inhibitor cocktail (Roche Applied Science, Indianapolis, IN, USA). Protein samples were separated by 8% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) under reducing conditions and transferred to a polyvinylidene fluoride membrane (Millipore, Billerica, MA, USA). The membranes were incubated sequentially with primary antibody (PAPP-A2, R&D Systems, Minneapolis, MN, USA; E-cadherin/ZO-1/ Vimentin/Snail/Slug, Cell Signaling Technology, Danvers, MA, USA; N-cadherin/GAPDH, Proteintech, Wuhan, China; Gli1/Gli2, Abcam, Cambridge, UK) and then horseradish peroxidase (HRP)-conjugated secondary antibody. Proteins were detected by an enhanced chemiluminescent detection kit (Amersham, Biosciences, Uppsala, Sweden), and the image was captured using VisionWorksLS image acquisition and analysis software, and the EC3 imaging system (UVP LLC, Upland, CA, USA).
Immunohistochemistry (IHC)
IHC was performed as previously described [27]. In brief, paraffin-embedded tissues were deparaffinized and rehydrated in xylene and gradients of ethanol. After boiling in citrate buffer at 92–98 ℃ for 15 min to retrieve antigen, the slides were incubated with 3% H2O2 to quench endogenous peroxidase and were blocked with bovine serum for 30 min. The slides were then incubated with primary antibodies against PAPP-A2 (Novus, Littleton, CO, USA) overnight at 4 ℃. Controls were processed by omitting primary antibodies. The following day, the slides were incubated with biotinylated secondary antibody for 30 min. After incubation, the slides were stained with 3,3′-Diaminobenzidine (DAB) working reagent and counterstained with hematoxylin. Immunostaining scoring of PAPPA2 in the tissues was evaluated by three independent observers based on staining intensity [28].
Primary trophoblast and cell culture
Trophoblasts were obtained from placental villous tissues of early pregnancy as previously described [29]. Placental villous tissues were dissected and digested with 0.25% trypsin (Sigma-Aldrich, St. Louis, MO, USA). Trophoblasts were purified by Percoll (Sigma-Aldrich, St. Louis, MO, USA) density gradient centrifugation and then collected at density between 1.048 and 1.062 g/mL. Cell viability which was identified by trypan blue was over 95%. Cell identity was confirmed via staining with cytokeratin 7 (CK7, Abcam, Cambridge, UK). Primary trophoblasts were cultured in Dulbecco’s Modified Eagle Medium (DMEM)/high glucose (GIBCO, Waltham, MA, USA) medium with 15% fetal bovine serum (FBS, GIBCO, Waltham, MA, USA).
The human HTR-8/SVneo cell line was purchased from the China Center for Type Culture Collection (CCTCC, Wuhan, China) [27]. It was derived from invasive EVT transfected with simian virus 40 large T antigen48 and used as a common model for EVT migration and invasion. HTR-8/SVneo cells were maintained in DMEM/high glucose medium supplemented with 10% FBS. The cells were cultured at 37 ℃ in a 5% CO2 humidified incubator. The small interfering RNA (siRNA) for silencing PAPP-A2 and a scrambled siRNA control were purchased from Genomeditech (Shanghai, China). The target sequence for PAPP-A2 was as follows: forward primer, 5′-GCUUAUCUCGGCAAUCAAAtt-3′; reverse primer, 5′-UUUGAUUGCCGAGAUAAGCgt-3′. Transfection was performed using lipofectamine 3000 regent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. After 48–72 h, transfection efficiency was determined by mRNA and protein expression analysis.
Immunofluorescence
Cells were fixed with 4% paraformaldehyde for 15 min, and then washed in phosphate buffered saline (PBS) and blocked with 10% goat serum for 1 h. Cells were subsequently incubated with the primary antibodies against PAPP-A2, CK7 or negative control (NC) overnight at 4 ℃. Cells were subsequently incubated with secondary Cy5 conjugated goat anti-rabbit antibody or FITC conjugated goat anti-mouse antibody (Invitrogen, Carlsbad, CA, USA) at room temperature for 1 h. All slides were counterstained with DAPI for nucleus staining and analyzed under a fluorescent microscope (Olympus IX73, Tokyo, Japan).
Cell proliferation assay
HTR-8/SVneo cells were placed in 96-well plates in DMEM/high glucose medium containing 10% FBS until 60–65% confluence. The cells were then incubated with recombinant human PAPP-A2 (rPAPP-A2) (R&D, Minneapolis, MN, USA) at concentrations of 0, 1.5, 3, 7.5 or 15 nM. After incubating for 24–72 h, the medium was removed and replaced with 100 μL of fresh serum-free culture medium. Cell proliferation was determined by the Cell Counting Kit-8 (Dojindo, Kumamoto, Japan) as per the manufacturer’s instructions. The absorbance was read at 450 nm. All procedures were conducted in sexplicates at least three times.
Cell apoptosis assay
HTR-8/SVneo cells were seeded in 12-well plates in a medium containing 1.5 nM rPAPP-A2, or PBS as the control. After 48 h, the cells were digested with 0.25% trypsin and re-suspended in binding buffer before incubation with fluorescein isothiocyanate (FITC)-Annexin V solution and propidium iodide (PI) as per the manufacturer’s instructions (BD Biosciences, New York, NY, USA).
Migration and invasion assays
The effect of PAPP-A2 on migration of HTR-8/SVneo cells was assessed by the wound-healing assay. Cells were pretreated with 1.5 nM rPAPP-A2 for 48 h and then seeded in 6-well plates until 80% confluence. A sterile 20 μL tip was used to generate the wound. The wound was photographed at 24 h and the affected area assessed by Image J software, and later compared to the initial wound area. For invasive assays, transwell inserts containing polycarbonate filters with 8 μm pores were coated with 50 μL matrigel matrix (1 × 104 mg/mL). After 48 h pretreatment with 1.5 nM of PAPP-A2, the HTR-8/SVneo cells were seeded into the upper chamber at a density of 5 × 104 cells/well with 100 μL serum-free DMEM medium. DMEM medium with 10% FBS acted as a chemoattractant in the lower chamber. After 24 h, the cells on the upper side of the inserts were removed by cotton swabbing. The remaining cells were fixed and stained with 0.5% crystal violet. The number of invading cells were photographed and counted. All experiments were done in triplicate wells and at least three times.
First trimester villous explant cultures
The placental villi were fully dissected before being explanted into the Millicell-CM culture dish inserts coated with matrigel and placed into 24-well culture plates. Serum free DMEM/F12 medium was added to the upper inserts and 10% FBS was added to the lower chamber. Explants were incubated with rPAPP-A2 (1.5 nM) or an equal volume of media for 72 h. Assessment of EVT outgrowth was performed as described previously [30]. EVT migration distance was measured by SPOT software (SPOT Imaging Solutions, Sterling Heights, MI, USA) from the villous tip to the distal edge. EVT outgrowths were quantified using the Adobe Illustrator software by dividing the area for 72 h by the initial area of the explant at 0 h.
Tube formation assay
Matrigel ~60 μL was layered into wells of the 96-well plate and then 5 × 104 pretreated cells (1.5 nM PAPP-A2 treatment, 50 nM PAPP-A2 siRNA transfection or 50 nM scrambled siRNA control transfection) were added and incubated at 37 ℃ for 8 h. Observations were made using an optical microscope (Olympus IX73, Tokyo, Japan). Phase-contrast images were taken at different time points to document developmental stages. Tube length and total number of branch points were assessed in four quadrants at ×10 magnification. Quantification was measured using Image J software. The assay was done in triplicate and repeated at least three times.
Statistical analysis
Results are presented as mean value ± standard error of mean (SEM) or as percentage of the control value from at least three independent experiments. Statistical analyses were performed with Prism 6.0 GraphPad software. Student’s t-test was used to compare between two groups and one-way analysis of variance (ANOVA) was used to compare multiple groups. A P-value < 0.05 was considered significant.
Results
Characteristics of the participants
The demographic and clinical characteristics of the participants in the four study groups are shown in Table 2. The preterm and normal pregnancy groups were matched with EOPE and LOPE, respectively, in terms of maternal age, weight, gestational age at delivery and incidence of primiparae. All participants presented with PE had proteinuria, and both PE groups had systolic and diastolic blood pressures that were significantly higher than their matched control groups.
Upregulation of PAPP-A2 mRNA and protein expression in PE
Expression of the molecules that limit cytotrophoblasts invasion and differentiation is dysregulated during development of PE. Therefore, we analyzed the levels of PAPP-A2 mRNA and protein in placental tissues from women with and without PE to evaluate if PAPP-A2 expression is affected during placental ischemia.
PAPP-A2 mRNA was detected by real-time PCR analysis of placental tissue. As shown in Fig. 1a, placental PAPP-A2 mRNA levels in the PE groups were higher than in controls. The EOPE group was significantly higher than the preterm control group, while the LOPE group was only slightly higher than the heathy control group (preterm, 0.51 ± 0.07 vs. EOPE, 4.76 ± 0.12; p < 0.0001; normal, 1.27 ± 0.20 vs. LOPE, 2.03 ± 0.10; p < 0.05). In addition, the expression of PAPP-A2 mRNA in placental tissue from women with EOPE was higher than that from those with LOPE. GAPDH was used to normalize the total RNA added during amplification. The results were expressed as the ratio of PAPP-A2 to GAPDH (Fig. 1a). Consistent with the mRNA results, PAPP-A2 protein was also present in higher levels in PE tissues than in controls (Fig. 1b, c; preterm, 0.31 ± 0.04 vs. EOPE, 3.63 ± 0.45; p < 0.01; normal, 0.76 ± 0.11 vs. LOPE, 1.77 ± 0.69; p < 0.05). Immunohistochemistry identified the level and localization of PAPP-A2 protein expression in placenta (Fig. 1d–f). PAPPA2-positive signals were observed in the syncytiotrophoblast layer of the villi and invasive extravillous trophoblasts at the basal plate zone, but not in the cytotrophoblasts at early gestation. EOPE showed stronger signal than its matched preterm group and LOPE group also had higher signal than matched normal pregnancy (Figs. 1e, f). Consistent with the above results, the intensity of the signal in EOPE group was significantly higher than that in LOPE group. These results indicated that PAPP-A2 expression is enhanced in PE.
PAPP-A2 (pregnancy-associated plasma protein-A2) mRNA and protein levels are elevated in preeclampsia placentas compared with gestation-matched controls. Real-time PCR (a), western blot (b, c), immunohistochemistry (e) detected the relative abundance of PAPP-A2 mRNA and protein in placental tissue lysate. Quantification analysis (a, c) and scoring of PAPP-A2 expression (f) showed that PAPP-A2 expression was elevated in EOPE (compared with gestation-matched preterm pregnancy) and LOPE (gestation-matched normal pregnancy). PAPP-A2 protein was localized to STBs but not in CTBs of the chorionic villi at early gestation (d-a). d-b showed CK7 staining to identify all trophoblasts. d-c and d-d demonstrated that CK7 positive (lower inserts) EVTs at BP showed prominent PAPP-A2 staining. d-d showed that STBs that are CK7 positive (lower inserts) stained for PAPP-A2. The upper insert is a partial enlargement of villus. EOPE severe early onset preeclampsia, LOPE severe late onset preeclampsia, STB syncytiotrophoblasts, EVT extravillous trophoblasts, BP basal plate. Data are expressed as mean ± SEM (*p < 0.05, **p < 0.01 and ****p < 0.0001)
PAPP-A2 expression in placental trophoblast cells
We conducted this experiment using primary placental trophoblasts isolated by an enzymatic digestion technique and the HTR-8/SVneo cell line. Immunofluorescent microscopy using PAPP-A2 antibody showed a positive signal in the cytoplasm of both primary trophoblasts and the immortalized trophoblast cell line (Fig. 2). Our results supported that PAPP-A2 protein was expressed in placental trophoblast cells.
Expression of PAPP-A2 (pregnancy-associated plasma protein-A2) in primary villous trophoblasts and HTR-8/SVneo cells. Immunofluorescent staining of the cells with PAPP-A2 antibody and monoclonal cytokeratin 7(CK7) antibody as shown in the photographs (bar = 50 μm). CK7 acts as the marker of placental trophoblasts
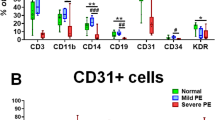
PAPP-A2 inhibits trophoblast migration, invasion and tube formation
EVT migration and invasion are key events in human placentation. Incubation of HTR-8/SVneo cells with 0–15 nM of rPAPP-A2 for 48 h caused no significant effect on proliferation (Fig. 3a, p > 0.05). Furthermore, the effect of PAPP-A2 on apoptosis in HTR-8/SVneo cells was investigated via flow cytometry with FITC-Annexin V and PI staining. Cells exposed to rPAPP-A2 were not significantly different to controls (Figs. 3b, c, p > 0.05).
PAPP-A2 (pregnancy-associated plasma protein-A2) shows no effect on proliferation and apoptosis of HTR-8/SVneo cells. a Proliferation of HTR-8/SVneo cells after treatment with recombinant PAPP-A2 (rPAPP-A2, 0–15 nM) for 48 h. The statistical significance of the differences between groups was determined by analysis of variance (ANOVA). b, c HTR-8/SVneo cells were harvested with recombinant PAPP-A2 (rPAPP-A2, 1.5 nM) for analysis with Annexin V staining. (NS means not significant)
To determine the effect of rPAPP-A2 on EVT migration, we performed the wound-healing assay with HTR-8/SVneo cells. In the absence of rPAPP-A2 (control), HTR-8/SVneo cells migrated to the middle of the area at 24 h. However, after exposure to rPAPP-A2, the migration velocity of HTR-8/SVneo cells slowed significantly (Fig. 4a, b; 88.98 ± 1.74 vs. 42.40 ± 1.46). The first trimester human placental villous explants were cultured on matrigel to model villous outgrowth and invasion (Fig. 4c). Compared to the control group, the migration distance and area of outgrown cells treated with rPAPP-A2 were substantially decreased (Fig. 4d; 100 ± 0.00 vs. 57.40 ± 3.28).
PAPP-A2 (pregnancy-associated plasma protein-A2) suppresses the migration of trophoblast cells and the outgrowth of EVTs from human placental explant. a, b Migration of HTR-8/SVneo cells after treatment with recombinant PAPP-A2 (rPAPP-A2, 1.5 nM) for 0 and 24 h by wound-healing assay (Bar = 100 μm). c, d The outgrowth area of the placental explants treated with 1.5 nM rPAPP-A2 was significantly lowered compared with that of explants treated with an equal volume of media as a control for 72 h (Bar = 100 μm). Data are expressed as mean ± SEM. (***p < 0.001, ****p < 0.0001)
The effect of PAPP-A2 on invasion of HTR-8/SVneo cells was studied using the transwell assay. Incubation of HTR-8/SVneo cells with rPAPP-A2 resulted in a significant decrease in cell invasion (Fig. 5d, e; control, 262.50 ± 5.14; rPAPP-A2, 120 ± 6.75; p < 0.0001). However, PAPP-A2 did not affect the proliferation and apoptosis of EVT within 72 h of observation. The suppressive effects of PAPP-A2 were detected in migration and invasion assays but did not impair cell proliferation and apoptosis.
PAPP-A2 (pregnancy-associated plasma protein-A2) suppresses the invasion and tube formation of trophoblast cells. Real-time PCR (a), western blot (b) and quantification of PAPP-A2 protein (c) demonstrated a significant reduction of PAPP-A2 mRNA and protein in HTR-8/SVneo cells transfected with siRNA specific for PAPP-A2 (50 nM, si-A2) compared with scrambled siRNA controls (si-C). d, e, The effect of treatment with 1.5 nM recombinant PAPP-A2 (rA2) or si-A2 on the invasion of HTR-8/SVneo cells by transwell assay (Bar = 20 μm). f, g, The network formation of HTR-8/SVneo cells cultured with 1.5 nM r-A2 or si-A2 assessed by the matrigel assay. (Bar = 100 μm). Data are expressed as mean ± SEM. (**p < 0.01, ***p < 0.001, ****p < 0.0001, NS means not significant, NC means negative control)
To ascertain these findings on PAPP-A2, we performed siRNA-mediated PAPP-A2 knockdown. Transfection of PAPP-A2 siRNA into cells resulted in a significant reduction in PAPP-A2 mRNA and protein expression in HTR-8/SVneo cells compared with transfection of the control scramble siRNA (Fig. 5a–c; mRNA, 0.600 ± 0.058, 0.077 ± 0.011; protein, 0.4616 ± 0.047, 0.099 ± 0.025). However, knockdown of PAPP-A2 expression in HTR-8/SVneo cells did not affect invasion (Fig. 5d, e). The results indicated that only abnormally elevated PAPP-A2 inhibited the invasion of trophoblasts and knockdown of PAPP-A2 did not cause any effect.
PAPP-A2 suppresses tube formation of EVT
Remodeling of maternal spiral arteries increases placental blood flow thereby ensuring sufficient oxygen and nutrient supply to the fetus. As this process is associated with trophoblast invasion we examined tube formation in HTR-8/SVneo cells. These cells were pretreated with 1.5 nM of rPAPP-A2 for 24 h and then seeded into a 96-well plate. The rate of formation of classical tube-like structures was decreased in PAPP-A2 treated cells compared to controls (Fig. 5f, g; 69 ± 5.05 vs. 34.25 ± 3.88; p < 0.01). In accord with the above findings, knockdown of PAPP-A2 expression in HTR-8/SVneo cells did not affect tube formation of trophoblasts.
PAPPA2 suppresses trophoblast invasion by inhibiting EMT via the Hedgehog signaling pathway
In order to explore whether PAPPA2 inhibited invasion of trophoblasts by mediating epithelial–mesenchymal translations (EMT), we performed a series of RT-qPCR and western blot assays to detect EMT markers. We have found that elevated PAPP-A2 decreased the expression of Vimentin and N-cadherin (the mesenchymal markers) whereas E-cadherin, ZO-1 (the epithelial markers) were upregulated in trophoblast cells (Fig. 6a–c). These results demonstrated that PAPPA2 suppresses trophoblast invasion by restraining EMT. To further investigate the molecular mechanisms of PAPP-A2 in regulating EMT, we analyzed the Hedgehog signaling pathway, including Gli1, Gli2, Snail and Slug. The mRNA and protein levels of Gli1, Gli2, Snail and Slug were significantly decreased in PAPP-A2-treated HTR8/SVneo cells, compared with normal controls. (Fig. 6d–f).
PAPP-A2 (pregnancy-associated plasma protein-A2) suppresses trophoblast invasion by restraining Hedgehog signaling pathway mediated EMT. Real-time PCR (a) and western blot (b, c) analysis of E-cadherin, ZO-1, Vimentin and N-cadherin in HTR-8/SVneo cells treated with or without recombinant PAPP-A2 (rA2, NC). The mRNA and protein levels of Gli1, Gli2, Snail and Slug were detected by RT-qPCR (d) and western blot (e, f) analysis, respectively. Data are expressed as mean ± SEM. (**p < 0.01, ***p < 0.001, ****p < 0.0001)
Discussion
In this present work, we have analyzed the expression of PAPP-A2 in placenta under different pathological and physiological conditions and also questioned and investigated the role of PAPP-A2 in placental development and angiogenesis in vitro. Evidence for the functional role of PAPP-A2 in placentation was deficient and controversial in some aspects. To our knowledge, it is the first time that PAPP-A2 is shown to have no effect on trophoblast proliferation and apoptosis but can suppress trophoblast migration, invasion by inducing EMT which can be related with the pathogenesis of PE.
PE arises subsequent to impaired spiral artery remodeling which results in reduced placental perfusion. Poor placentation ensues, causing systemic pathophysiological changes in the maternal circulation [31]. It is becoming clear that the etiology of EOPE and LOPE, as well as intra-uterine growth restriction may be caused by overlapping yet distinct underlying reasons. The pathogenesis of PE is established prior to the appearance of clinical symptoms. LOPE accounts for ~80% of PE cases worldwide with normal placental morphology and umbilical artery Doppler profiles while EOPE tends to be more severe with abnormal placental villous and vascular morphology [1]. Unlike previous studies, we have studied PAPP-A2 expression in EOPE and LOPE groups separately. PAPP-A2 synthesis was significantly higher in EOPE compared with preterm controls, whereas LOPE placentas produced slightly increased expression when compared with healthy controls. We then demonstrated differential PAPP-A2 expression in EOPE versus LOPE placentas, showing higher expression in EOPE that lead us to assume that the extent of increased PAPP-A2 expression seems to correlate with PE severity and the underlying mechanisms behind the different types of PE.
Immunohistochemistry was performed to identify specific sites and levels of PAPP-A2 expression in EOPE and LOPE placentas. Placental tissues from PE demonstrated increased levels of PAPP-A2, with higher levels in EOPE. Consistent with previous research results [13, 14], PAPP-A2 was expressed in syncytiotrophoblasts, invasive cytotrophoblasts but not in villous cytotrophoblasts. In preterm placenta, equivalent to the second trimester, a marked decrease staining was seen. PAPP-A2 is expressed in syncytiotrophoblasts throughout pregnancy and EVT in the basal plate showed intense expression of PAPP-A2. We speculated that PAPP-A2 participates in the differentiation of trophoblasts and the invasive phenotype of EVT.
Adequate uterine blood flow and intervillous space perfusion play important roles in sustaining normal pregnancies and fetal growth. They are achieved by extravillous trophoblast invasion and spiral remodeling of large diameter vessels [32]. The mechanism for the inhibitory effects of PAPP-A2 on EVT invasion remains unclear. Previous studies have identified that IL-11, partly via upregulation of PAPP-A2, impairs EVT invasion into the endometrium and endovascular EVT remodeling of the maternal spiral artery [33]. It has been reported that the presence of hypoxia responsive element (HRE) and two nuclear factor (NF)-kB binding sites within the PAPP-A2 promoter region, supports a link between hypoxia and elevated PAPP-A2 expression in the severe EOPE placenta [34]. Thus, the upregulation of PAPP-A2 in PE may be due to placental ischemia and hypoxia, resulting in poor placentation. Further research is required to fully comprehend the molecular mechanisms underpinning the development of PE.
In our study, additional rPAPP-A2 suppresses trophoblast cell migration, invasion and tube formation suggesting that PAPP-A2 participates in the pathogenesis of pregnancy-associated complications. Therefore, we propose that increased expression of placental PAPP-A2 may have a negative effect on trophoblast function but does not impair cell proliferation and apoptosis. This may lead to poor remodeling of maternal spiral arteries and the abnormal uteroplacental arterial blood flow associated with PE. Previous studies [14, 35] showed that PAPP-A2 was expressed in normal pregnancy and variations over gestation suggested that PAPP-A2 may have a physiological effect in maintaining a normal pregnancy. Once a certain threshold was exceeded, pathological effects might occur which may explain why knockdown of endogenous PAPP-A2 did not affect the migration and invasion of trophoblast. Thus, PAPP-A2 has the potential to be a therapeutic target or predictor of severe PE. Previous study shows that serum PAPP-A2 has good sensitivity and specificity for PE severity [13], further supporting its potential application in PE detection.
EMT plays crucial roles in carcinoma progression and metastasis and is associated with the loss of epithelial-cell adhesiveness and polarity, acquisition enhanced mobility and change to a mesenchymal phenotype [36]. Molecularly, EMT involves the decreased level of epithelial-type proteins E-cadherin and ZO-1 and the upregulation of mesenchymal markers including vimentin as well as EMT associated transcriptional factors, including Snail and Slug [37]. Remarkably, EVTs show a phenotype very similar to that of cancer cells, with regards to their capacity for invasion and migration [38]. The invasive phenotype of extravillous trophoblasts is associated with a decline in E-cadherin and increased levels of N-cadherin [39]. In our study, recombinant PAPP-A2 significantly induced mesenchymal–epithelial translations (MET) directing the downregulation of vimentin and N-cadherin expression and increased E-cadherin and ZO-1 expression. Therefore, these results indicated that PAPP-A2 was positively related to EMT markers and PAPP-A2 might suppress EVT invasion by restraining EMT process.
The Hedgehog signaling pathway plays a vital role in regulating cell differentiation during embryonic development and participates in the transformation of epithelial cells into mesenchymal cells in trophoblast cells [40, 41]. Gli1 and Gli2 are transcriptional regulator factors in the Hedgehog signaling pathway. It has been reported that Gli1 induces the expression of key EMT regulators including Twist, Snail and Slug and both Gli1 and Gli2 directly attenuates CDH1 gene encoding E-cadherin in human trophoblasts [42]. In our study, we demonstrated that PAPP-A2 downregulated the expression of Gli1 and Gli2 as well as EMT transcription factors Snail and Slug. Both Snail and Slug repress adherents (E-cadherin) and tight junction components (ZO-1) in ovarian cancer cells [43]. Through our results, we have testified that PAPP-A2 downregulated the invasive ability of trophoblasts by repressing the Hedgehog signaling pathway.
In conclusion, our study demonstrates that elevated placental expression of PAPPA2 expresses changes in placentas associated with severe PE and could regulate the biological functions of trophoblasts. The marked increase in expression in EOPE than LOPE was possibly due to prolonged placental ischemia and hypoxia. Moreover, PAPP-A2 is involved in trophoblast dysfunction via EMT by the Hedgehog signaling pathway. Our findings reveal a potential role for PAPP-A2 in regulating placental function and propose the possible underlying mechanism of PE. PAPP-A2 might be a promising predictor or therapeutic option for severe PE progression. Our present research accentuates on the need for further research into the implications of PAPP-A2 in pregnancy.
References
James JL, Whitley GS, Cartwright JE. Pre-eclampsia: fitting together the placental, immune and cardiovascular pieces. J Pathol. 2010;221:363–78.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–44.
Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS. Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol. 2014;124:771–81.
Carty DM, Delles C, Dominiczak AF. Novel biomarkers for predicting preeclampsia. Trends Cardiovasc Med. 2008;18:186–94.
Herzog EM, Eggink AJ, Willemsen SP, Slieker RC, Wijnands KPJ, Felix JF, Chen J, Stubbs A, van der Spek PJ, van Meurs JB, Steegers-Theunissen RPM. Early- and late-onset preeclampsia and the tissue-specific epigenome of the placenta and newborn. Placenta. 2017;58:122–32.
Redman CW, Sacks GP, Sargent IL. Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999;180(2 Pt 1):499–506.
Brosens IA, Robertson WB, Dixon HG. The role of the spiral arteries in the pathogenesis of preeclampsia. Obstet Gynecol Annu. 1972;1:177–91.
Overgaard MT, Boldt HB, Laursen LS, Sottrup-Jensen L, Conover CA, Oxvig C. Pregnancy-associated plasma protein-A2 (PAPP-A2), a novel insulin-like growth factor-binding protein-5 proteinase. J Biol Chem. 2001;276:21849–53.
Kjaer-Sorensen K, Engholm DH, Jepsen MR, Morch MG, Weyer K, Hefting LL. et al. Papp-a2 modulates development of cranial cartilage and angiogenesis in zebrafish embryos. J Cell Sci. 2014;127(Pt 23):5027–37.
Oxvig C. The role of PAPP-A in the IGF system: location, location, location. J Cell Commun Signal. 2015;9:177–87.
Yan X, Baxter RC, Firth SM. Involvement of pregnancy-associated plasma protein-A2 in insulin-like growth factor (IGF) binding protein-5 proteolysis during pregnancy: a potential mechanism for increasing IGF bioavailability. J Clin Endocrinol Metab. 2010;95:1412–20.
Chasen ST, Wasden S. Sequential testing for Down syndrome: the impact on estimated risk. Prenat Diagn. 2012;32:138–41.
Nishizawa H, Pryor-Koishi K, Suzuki M, Kato T, Kogo H, Sekiya T, Kurahashi H, Udagawa Y. Increased levels of pregnancy-associated plasma protein-A2 in the serum of pre-eclamptic patients. Mol Hum Reprod. 2008;14:595–602.
Kramer AW, Lamale-Smith LM, Winn VD. Differential expression of human placental PAPP-A2 over gestation and in preeclampsia. Placenta. 2016;37:19–25.
Várkonyi T1, Nagy B, Füle T, Tarca AL, Karászi K, Schönléber J, Hupuczi P, Mihalik N, Kovalszky I, Rigó J Jr, Meiri H, Papp Z, Romero R, Than NG. Microarray profiling reveals that placental transcriptomes of early-onset HELLP syndrome and preeclampsia are similar. Placenta. 2011;32:Suppl:S21–29.
Whitehead CL, Walker SP, Ye L, Mendis S, Kaitu’u-Lino TJ, Lappas M, Tong S. Placental specific mRNA in the maternal circulation are globally dysregulated in pregnancies complicated by fetal growth restriction. J Clin Endocrinol Metab. 2013;98:E429–436.
Crosley EJ, Dunk CE, Beristain AG, Christians JK. IGFBP-4 and -5 are expressed in first-trimester villi and differentially regulate the migration of HTR-8/SVneo cells. Reprod Biol Endocrinol: RBamp;E. 2014;12:123.
Amiri N, Christians JK. PAPP-A2 expression by osteoblasts is required for normal postnatal growth in mice. Growth Horm IGF Res. 2015;25:274–80.
Christians JK, Hoeflich A, Keightley PD. PAPPA2, an enzyme that cleaves an insulin-like growth-factor-binding protein, is a candidate gene for a quantitative trait locus affecting body size in mice. Genetics. 2006;173:1547–53.
Christians JK, de Zwaan DR, Fung SH. Pregnancy associated plasma protein A2 (PAPP-A2) affects bone size and shape and contributes to natural variation in postnatal growth in mice. PLoS One. 2013;8:e56260.
Argente J, Chowen JA, Perez-Jurado LA, Frystyk J, Oxvig C. One level up: abnormal proteolytic regulation of IGF activity plays a role in human pathophysiology. EMBO Mol Med. 2017;9:1338–45.
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000;183:S1–s22.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003;102:181–92.
Brown MA, Hague WM, Higgins J, Lowe S, McCowan L, Oats J. et al. The detection, investigation and management of hypertension in pregnancy: executive summary. Aust & NZ J Obstet & Gynaecol. 2000;40:133–8.
Waugh JJ, Clark TJ, Divakaran TG, Khan KS, Kilby MD. Accuracy of urinalysis dipstick techniques in predicting significant proteinuria in pregnancy. Obstet Gynecol. 2004;103:769–77.
von Dadelszen P, Magee LA, Roberts JM. Subclassification of preeclampsia. Hypertens Pregnancy. 2003;22:143–8.
Xiao J, Feng Y, Li X, Li W, Fan L, Liu J. et al. Expression of ADAMTS13 in normal and abnormal placentae and its potential role in angiogenesis and placenta development. Arterioscler Thromb Vasc Biol. 2017;37:1748–56.
Su S, Liu Q, Chen J, Chen J, Chen F, He C. et al. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis. Cancer Cell. 2014;25:605–20.
Kliman HJ, Nestler JE, Sermasi E, Sanger JM, Strauss JF, 3rd. Purification, characterization, and in vitro differentiation of cytotrophoblasts from human term placentae. Endocrinology. 1986;118:1567–82.
Hu Y, Tan R, MacCalman CD, Eastabrook G, Park SH, Dutz JP. et al. IFN-gamma-mediated extravillous trophoblast outgrowth inhibition in first trimester explant culture: a role for insulin-like growth factors. Mol Hum Reprod. 2008;14:281–9.
Shen L, Diao Z, Sun HX, Yan GJ, Wang Z, Li RT. et al. Up-regulation of CD81 inhibits cytotrophoblast invasion and mediates maternal endothelial cell dysfunction in preeclampsia. Proc Natl Acad Sci USA. 2017;114:1940–5.
Brosens I, Robertson WB, Dixon HG. The physiological response of the vessels of the placental bed to normal pregnancy. J Pathol Bacteriol. 1967;93:569–79.
Winship AL, Koga K, Menkhorst E, Van Sinderen M, Rainczuk K, NagaiM et al. Interleukin-11 alters placentation and causes preeclampsia features in mice. Proc Natl Acad Sci USA. 2015;112:15928–33.
Macintire K, Tuohey L, Ye L, Palmer K, Gantier M, Tong S. et al. PAPPA2 is increased in severe early onset pre-eclampsia and upregulated with hypoxia. Reprod Fertil Dev. 2014;26:351–7.
Kloverpris S, Gaidamauskas E, Rasmussen LC, Overgaard MT, Kronborg C, Knudsen UB. et al. A robust immunoassay for pregnancy-associated plasma protein-A2 based on analysis of circulating antigen: establishment of normal ranges in pregnancy. Mol Hum Reprod. 2013;19:756–63.
Yilmaz M, Christofori G. EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastas Rev. 2009;28:15–33.
Du L, Kuang L, He F, Tang W, Sun W, Chen D. Mesenchymal-to-epithelial transition in the placental tissues of patients with preeclampsia. Hypertens Res. 2017;40:67–72.
Holtan SG, Creedon DJ, Haluska P, Markovic SN. Cancer and pregnancy: parallels in growth, invasion, and immune modulation and implications for cancer therapeutic agents. Mayo Clin Proc. 2009;84:985–1000.
Voulgari A, Pintzas A. Epithelial-mesenchymal transition in cancer metastasis: mechanisms, markers and strategies to overcome drug resistance in the clinic. Biochim Biophys Acta. 2009;1796:75–90.
Zhang Y, Zhang Y. Forkhead box C2 promotes the invasion ability of human trophoblast cells through Hedgehog (Hh) signaling pathway. Cell Biol Int. 2018;42:859–66.
Lum L, Beachy PA. The Hedgehog response network: sensors, switches, and routers. Science. 2004;304:1755–9.
Tang C, Mei L, Pan L, Xiong W, Zhu H, Ruan H. et al. Hedgehog signaling through GLI1 and GLI2 is required for epithelial-mesenchymal transition in human trophoblasts. Biochim Biophys Acta. 2015;1850:1438–48.
Kurrey NK, K A, Bapat SA. Snail and Slug are major determinants of ovarian cancer invasiveness at the transcription level. Gynecol Oncol. 2005;97:155–65.
Acknowledgements
This work was supported by the grants from National Natural Science Foundation of China (30672243, 81701476, 81200354), and Applied Basic Research Plan of Wuhan (2015060101010037 to S. Chen). We are grateful to Xue Zeng and Rui Wei for their advice in experiment design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, X., Chen, K., Feng, Y. et al. The potential role of pregnancy-associated plasma protein-A2 in angiogenesis and development of preeclampsia. Hypertens Res 42, 970–980 (2019). https://doi.org/10.1038/s41440-019-0224-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0224-8
This article is cited by
-
Alpha-2-macroglobulin is involved in the occurrence of early-onset pre-eclampsia via its negative impact on uterine spiral artery remodeling and placental angiogenesis
BMC Medicine (2023)
-
RNA profiles reveal signatures of future health and disease in pregnancy
Nature (2022)
-
Dysfunction of Shh signaling activates autophagy to inhibit trophoblast motility in recurrent miscarriage
Experimental & Molecular Medicine (2021)
-
Uteroplacental Ischemia Is Associated with Increased PAPP-A2
Reproductive Sciences (2020)