Abstract
Adrenal venous sampling (AVS) is the gold standard test for distinguishing between unilateral and bilateral primary aldosteronism (PA); however, AVS requires advanced and time consuming technique. The needs for AVS have been increasing due to the increased utilization of screening for PA. An efficient selection of unilateral PA, such as aldosterone-producing adenoma (APA), before AVS is useful to avoid undesirable AVS in bilateral PA, such as idiopathic hyperaldosteronism. In this study, 40 patients who received all three confirmatory tests, including the captopril challenge test, furosemide upright test and adrenocorticotropin (ACTH) stimulation test (AST), and who were diagnosed as having PA by AVS were recruited. Subjects were diagnosed as having unilateral aldosterone excess (n = 22) or bilateral aldosterone excess (n = 18) by AVS. All patients with unilateral PA underwent an operation and were finally diagnosed with APA. Major differences were detected in serum potassium level, basal plasma aldosterone concentration (PAC), presence of adrenal tumor, and AST results between the two groups. The PAC/cortisol ratio at 120 min in the AST showed the highest diagnostic capability for distinguishing the subtypes of PA according to a receiver operating characteristic (ROC) curve analysis (area under the ROC curve was 0.956). At a cutoff value of 1.20 for the PAC/cortisol ratio at 120 min on the AST, the sensitivity was 95.5%, and the specificity was 88.9%. This sufficiently high sensitivity suggests that the PAC/cortisol ratio at 120 min in the AST could be useful for the screening of patients with PA who are suitable for AVS.
Similar content being viewed by others

Introduction
Primary aldosteronism (PA) is the most common cause of endocrine hypertension. The incidence of PA in hypertensive patients is high but ranges widely, from 3.2 to 21.7% [1]. Moreover, PA is associated with a higher risk of cardiovascular events and renal damage than essential hypertension [2,3,4]. Thus, early detection and treatment of PA is crucial. The diagnostic guidelines for PA from the Japanese Endocrine Society (JES) recommend the measurement of the plasma aldosterone concentration (PAC)/plasma renin activity (PRA) ratio (ARR) in patients who are initially diagnosed with hypertension [5]. Recently, the Task Force of the Endocrine Society, which is an international committee that includes the JES and the Japanese Society of Hypertension (JSH), recommended a screening test, namely, ARR, for high-risk groups of hypertensive patients and those with hypokalemia [6]. If the ARR is higher than 20 (the units of PAC are in ng/dL), the guidelines recommend referral to a specialized institution for a definitive diagnosis [5, 6]. Regardless of the criteria for target subjects, patient referrals have been increasing due to the increased dissemination and awareness of the ARR in Japan.
At least two of three confirmatory tests, including the captopril challenge test (CCT), furosemide upright test (FUT), and saline infusion test are recommended to reach a definitive diagnosis for referred patients [5]. The adrenocorticotropin (ACTH) stimulation test (AST) is not sufficient as a confirmatory test of PA [7], but the AST is useful for identifying aldosterone-producing adenoma (APA) [8,9,10]. We have been using the AST to confirm aldosterone hypersecretion in the basal state and normalization of aldosterone secretion after operation. Adrenal venous sampling (AVS) is recommended as a gold standard test for reaching a final diagnosis of the PA subtype [5, 6]. However, AVS requires advanced and time consuming technique, so the efficient selection of patients with unilateral PA such as APA before the AVS is useful to avoid undesirable AVS in patients with bilateral PA, such as idiopathic hyperaldosteronism (IHA). Recently, many efforts have been devoted to identifying alternative tests to substitute for the AVS or to provide a validation for patients who are undergoing elective AVS, but adequate tests with sufficient accuracy have not been identified [11]. The objective of this study was to identify a more useful marker for distinguishing the subtype of PA to reduce the number of patients undergoing unnecessary AVS.
Methods
Study patients
We retrospectively analyzed the medical records of patients who were diagnosed with PA by confirmatory tests including AST and localization by AVS from July 2011 to March 2018. The saline infusion test has not been enforced due to its troublesome procedure. Forty patients who met all eligibility conditions were recruited. This study was a retrospective study without intervention and was approved by the Ethical Committees of the University of Miyazaki. All patients who were included in the study underwent contrast CT imaging.
Diagnostic procedure for PA
Patients with an ARR greater than 20 and who were expected to have surgery were admitted to our hospital. All patients were put on Ca-channel blocker(s) and/or an alpha-blocker before the examination. Oral potassium supplementation was administered as necessary. The patients were fed 10 g of sodium chloride per day in the hospital. All basal blood sampling for the confirmatory tests were carried out at 08:00 to 08:30 after an overnight fasting. Plasma concentrations of hormones were measured using a commercially available laboratory testing service (BML, Tokyo, Japan).
Captopril challenge test
Patients took 25 mg of captopril after 60 min of rest in a supine position. Blood samples were obtained before and after taking captopril. An ARR greater than 20 at 60 min after captopril administration was considered positive. The baseline PAC and PRA values in the CCT were used as basal values for this analysis.
Furosemide upright test
After 30 min resting in a supine position, patients were administered 1 mg/kg of furosemide (up to 60 mg) by an intravenous injection and maintained in a standing position for two hours. PRA values <2.0 ng/ml/h at 120 min after furosemide loading were considered positive.
ACTH stimulating test
After 30 min of rest in a supine position, patients were administered 250 μg of synthetic ACTH by an intravenous injection. Blood samples were obtained before and 30, 60 and 120 min after loading. A ratio of PAC to cortisol that was higher than 0.85 at the time of peak concentration of aldosterone (PACmax/cortisol) after the ACTH injection was considered to be positive.
Adrenal venous sampling
AVS was performed by expert radiologists. To confirm the correct localization of the microcatheter tip to the right adrenal vein, CT imaging was performed during the operation in all patients [12]. Following basal sampling from the bilateral adrenal veins, 250 μg of ACTH were administered by an intravenous injection. After 30 min of waiting, the second sampling was performed from the adrenal veins. According to the JES guidelines [5], an adrenal venous cortisol concentration greater than 200 μg/dL after the ACTH stimulation was considered to be evidence of an adequate catheterization for the AVS. An adrenal venous aldosterone concentration higher than 1400 ng/dL after the ACTH stimulation was considered to be evidence of aldosterone hypersecretion. The lateralization of the hypersecretion of adrenal vinous aldosterone was the primary criterion for the diagnosis of the bilateral or unilateral PA subtypes. Additionally, the lateralized ratio (comparison of aldosterone/cortisol ratio on both sides of the adrenal vein; higher/lower side <2.6) and contralateral ratio (comparison of aldosterone/cortisol ratio on the lower side of the adrenal vein/inferior vena cava; over 1.0) were used for the diagnosis of bilateral PA.
Statistical analysis
All statistical analyses were performed using SPSS Statistics, version 22 (IBM Japan, Tokyo, Japan). After the confirmation of normal distributions for all variables, the significance of the differences between unilateral PA and bilateral PA was evaluated by an unpaired t test or Χ2 test. The relationship between variables was analyzed using a simple correlation analysis. A receiver operating characteristic (ROC) curve was generated, and the area under the curve (AUC) was calculated to determine the best marker for detecting the subtype. Data are expressed as the means ± SD, and a value of P < 0.05 was the criterion for statistical significance.
Results
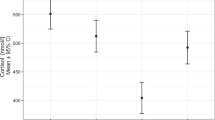
The final diagnosis of laterality was determined by obvious aldosterone hypersecretion in AVS. All patients who were diagnosed with unilateral PA underwent a laparoscopic adrenalectomy and were finally diagnosed as having APA based on the pathological diagnosis. In addition, all operated patients were postoperatively reexamined by the AST, and the normalization of aldosterone secretion was confirmed (Fig. 1). The baseline characteristics of the patients and a summary of the confirmatory tests are shown in Table 1. Patients with unilateral PA that were confirmed as having APA after their operation were accompanied with severe hypokalemia than patients with bilateral PA. The PAC, ARR, and incidence of adrenal tumor were significantly higher in the unilateral group, and the PRA after loading in the FUT was significantly lower in the unilateral group. The results for the AST, including the post operation values, are illustrated in Fig. 1. PAC and the PAC/cortisol ratio were significantly higher at every timepoint for the AST in the unilateral group. Consequently, the PACmax/cortisol ratio was significantly higher in the unilateral group (Table 1).
To determine the best predictor for detecting the unilateral PA, an ROC curve analysis was conducted, and the AUCs were compared (Table 2). Serum potassium, presence of adrenal tumor and the recommended confirmatory tests such as CCT and FUT have a low ability to distinguish between the PA subtypes. In contrast, the AST showed a higher ability to distinguish between the PA subtypes. Several markers, including previously reported markers [8,9,10], are summarized in Table 2. In particular, the PAC/cortisol ratio at 120 min showed an extraordinarily high AUC (0.956) compared to the other markers. The ROC curves for each of the markers in the AST are illustrated in Fig. 2. The ROC curve for the PAC/cortisol ratio at 120 min surpassed that of the other markers at all points. Using the ROC curve analysis, a cutoff value of 1.20 was set for the PAC/cortisol ratio at 120 min in the AST. Among patients with unilateral PA, 21 of 22 patients had ratios above the 1.20 cutoff (sensitivity of 95.5%), and 16 of 18 patients with bilateral PA had ratios below 1.20 (specificity of 88.9%) (Fig. 3).
Discussion
The purpose of this study was to identify a predictor of unilateral PA for an efficient and desirable AVS that is connected to a curable operation. There have been some reports suggesting that the AST is useful for the determination of APA [8,9,10] but that its accuracy was insufficient [11]. We identified a more useful marker and cutoff value, namely, a PAC/cortisol ratio of 1.20 at 120 min in the AST, with sufficiently high sensitivity (95.5%) for the determination of APA. The AST is a convenient and safe test, so the use of the AST to select for patients with APA prior to the AVS is versatile and beneficial in clinical practice.
According to previous reports, APA showed a higher response to ACTH stimulation than IHA [8,9,10, 13]. Consistent with these findings, in our study the unilateral group showed a significantly higher response than the bilateral group (Fig. 1). Additionally, the unilateral group showed prolonged response to ACTH stimulation and maintained a high level of PAC at 120 min (mean difference between 0 min and 120 min was 22.0 ng/dL). In contrast, the bilateral group returned to near the basal level at 120 min (mean difference between 0 min and 120 min was 8.5 ng/dL). The serum concentration of cortisol was highest at 120 min and was slightly higher in the bilateral group than in the unilateral group (28.3 vs. 25.8 μg/dL. P = 0.076). Consequently, the PAC/cortisol ratio in the bilateral group was lowest at 120 min with the lowest dispersion (Fig. 1). Thus, the PAC/cortisol ratio at 120 min was chosen as the distinguishing marker for the subtype of PA. The PAC/cortisol ratio at 0 min also showed a high AUC in the ROC curve analysis (Table 2). However, there were many overlaps between the two groups and thus the ratio showed low specificity (sensitivity of 95.5%, specificity of 44.4%, at a cutoff value of 1.84).
PAC was suppressed more strongly by 1 mg dexamethasone in the APA group than in the non-PA and IHA groups [8, 14,15,16]. PAC has a circadian rhythm, with levels rising in the morning and declining at night. This circadian rhythm was prominent in the patients with APA [17] and the rhythm in the APA patients was depended on endogenous ACTH [15, 16]. These data indicate that aldosterone secretion is more dependent upon endogenous ACTH in the APA group than in the IHA group. Therefore, it is convincing that the APA group showed a greater reaction to exogenous ACTH stimulation than did the IHA group. Conversely, patients with a higher response to exogenous ACTH may secrete more aldosterone via endogenous ACTH and suffer from the adverse effects of excess aldosterone. Indeed, the PACmax/cortisol ratio in the AST showed a fairly strong association with hypokalemia in this study (Fig. 4). These data suggest that careful assessment and follow-up are needed for patients showing a high response in the AST.
Two of the 18 patients with bilateral PA showed a PAC/cortisol ratio at 120 min that was above the cutoff value in the AST (Fig. 3). These patients had no adrenal nodules and seemed to have IHA, but they may have harbored bilateral microadenomas or a unilateral microadenoma with contralateral hyperplasia. Considering the balance between very high sensitivity and adequate specificity, the cutoff value for the PAC/cortisol at 120 min seems to be superior to other parameters for distinguishing the PA subtype using the AST [8,9,10,11]. Recently, Umakoshi et al. reported that the combination of a unilateral nodule on a CT and hypokalemia were useful indicators for the selection of preferable patients for AVS [18]. However, individual AUCs of adrenal nodules (AUC 0.782) or hypokalemia (AUC 0.764) were relatively low and the AUC of the combination of an adrenal nodule and hypokalemia was also insufficient in our cohort (AUC 0.813). Moreover, the AST can distinguish between unilateral and bilateral disease in patients with normokalemia without obvious adrenal nodules (PAC/cortisol at 120 min was 1.3 and serum potassium was 4.0 mEq/L), although this was demonstrated in one patient. Only 1 of 22 patients with APA that was confirmed by a pathological examination showed a value below the cutoff. This patient showed a low basal PAC (13 ng/dL) and marginal responses to confirmatory tests (PAC/PRA at 60 min in the CCT, 18; PRA at 120 min in the FUT, 1.5 ng/ml/h). The patient also had normokalemia (potassium level, 4.0 mEq/L) and showed only a limited improvement in blood pressure after operation. A higher body mass index (BMI) and lower contralateral index in the AVS after ACTH stimulation are reported as predictors for poor blood pressure response after operation [19]. This patient had a relatively high BMI (24.0) but a relatively low contralateral index (0.3). This may suggest that a low responder in the AST can be observed without an operation. However, the repeated use of the AST would be necessary for low responders to avoid overlooking latent APA.
There are several limitations in this study. We considered performing AVS even if the patients showed positive response in only the AST. Such patients may be diagnosed with essential hypertension at other facilities. The final diagnosis was dependent upon obvious aldosterone hypersecretion in the AVS. The guidelines for PA are still evolving, and the details for this diagnosis are not unified among academic societies such as the JES and JSH. As a result, the patient population may be heterogeneous among facilities. The number of the patients was relatively small in the present study, and it was performed at a single facility. A study with a larger number of patients and at multiple facilities is warranted in the future. Finally, pathological examinations were not applied for bilateral lesions, so the diagnosis of IHA may not be correct in some cases.
In conclusion, patients who were suspected to have PA and who had PAC/cortisol ratios of 1.20 or less at 120 min in the AST can be excluded from the AVS because they are most possible to be bilateral PA. The use of this parameter for patient selection would be useful for minimizing the use of the AVS in cases where it would be unnecessary and/or undesirable.
References
Nishikawa T, Saito J, Omura M. Prevalence of primary aldosteronism: should we screen for primary aldosteronism before treating hypertensive patients with medication? Endocr J. 2007;54:487–95.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Born-Frontsberg E, Reincke M, Rump LC, Hahner S, Diederich S, Lorenz R, Participants of the German Conn’s Registry. et al. Cardiovascular and cerebrovascular comorbidities of hypokalemic and normokalemic primary aldosteronism: results of the German Conn’s Registry. J Clin Endocrinol Metab. 2009;94:1125–30.
Rossi GP, Bernini G, Desideri G, Fabris B, Ferri C, Giacchetti G, PAPY Study Participants. et al. Renal damage in primary aldosteronism: results of the PAPY Study. Hypertension. 2006;48:232–8.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, Tanabe A, Task Force Committee on Primary Aldosteronism, The Japan Endocrine Society. Guidelines for the diagnosis and treatment of primary aldosteronism--the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Terui K, Kageyama K, Nigawara T, Moriyama T, Sakihara S, Takayasu S, et al. Evaluation of the (1-24) adrenocorticotropin stimulation test for the diagnosis of primary aldosteronism. J Renin Angiotensin Aldosterone Syst. 2016;17:1470320315625703.
Sonoyama T, Sone M, Miyashita K, Tamura N, Yamahara K, Park K, et al. Significance of adrenocorticotropin stimulation test in the diagnosis of an aldosterone-producing adenoma. J Clin Endocrinol Metab. 2011;96:2771–8.
Jiang Y, Zhang C, Wang W, Su T, Zhou W, Jiang L, et al. Diagnostic value of ACTH stimulation test in determining the subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2015;100:1837–44.
Moriya A, Yamamoto M, Kobayashi S, Nagamine T, Takeichi-Hattori N, Nagao M, et al. ACTH stimulation test and computed tomography are useful for differentiating the subtype of primary aldosteronism. Endocr J. 2017;64:65–73.
Buffolo F, Monticone S, Williams TA, Rossato D, Burrello J, Tetti M, et al. Subtype diagnosis of primary aldosteronism: is adrenal vein sampling always necessary? Int J Mol Sci. 2017;18:E848.
Onozawa S, Murata S, Tajima H, Yamaguchi H, Mine T, Ishizaki A, et al. Evaluation of right adrenal vein cannulation by computed tomography angiography in 140 consecutive patients undergoing adrenal venous sampling. Eur J Endocrinol. 2014;170:601–8.
Stowasser M, Klemm SA, Tunny TJ, Gordon RD. Plasma aldosterone response to ACTH in subtypes of primary aldosteronism. Clin Exp Pharmacol Physiol. 1995;22:460–2.
Newton MA, Laragh JH. Effects of glucocorticoid administration on aldosterone excretion and plasma renin in normal subjects, in essential hypertension and in primary aldosteronism. J Clin Endocrinol Metab. 1968;28:1014–22.
Kem DC, Weinberger MH, Gomez-Sanchez C, Kramer NJ, Lerman R, Furuyama S, et al. Circadian rhythm of plasma aldosterone concentration in patients with primary aldosteronism. J Clin Invest. 1973;52:2272–7.
Sonoyama T, Sone M, Tamura N, Honda K, Taura D, Kojima K, et al. Role of endogenous ACTH on circadian aldosterone rhythm in patients with primary aldosteronism. Endocr Connect. 2014;3:173–9.
Kobayashi H, Haketa A, Ueno T, Suzuki R, Aoi N, Ikeda Y, et al. Subtype prediction in primary aldosteronism: measurement of circadian variation of adrenocortical hormones and 24-h urinary aldosterone. Clin Endocrinol (Oxf). 2016;84:814–21.
Umakoshi H, Tsuiki M, Takeda Y, Kurihara I, Itoh H, Katabami T, JPAS Study Group. et al. Significance of computed tomography and serum potassium in predicting subtype diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2018;103:900–8.
Bokuda K, Yatabe M, Mizuguchi Y, Niiyama M, Seki Y, Watanabe D, et al. Body mass index and contralateral ratio predict outcome following unilateral adrenalectomy in primary aldosteronism. Hypertens Res. 2017;40:988–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kita, T., Furukoji, E., Sakae, T. et al. Efficient screening of patients with aldosterone-producing adenoma using the ACTH stimulation test. Hypertens Res 42, 801–806 (2019). https://doi.org/10.1038/s41440-018-0191-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0191-5
Keywords
This article is cited by
-
Urinary sodium/potassium ratio as a screening tool for hyperaldosteronism in men with hypertension
Hypertension Research (2021)
-
Cosyntropin stimulation in adrenal vein sampling improves the judgment of successful adrenal vein catheterization and outcome prediction for primary aldosteronism
Hypertension Research (2020)
-
Comparison of the shortened and standard saline infusion tests for primary aldosteronism diagnostics
Hypertension Research (2020)