Abstract
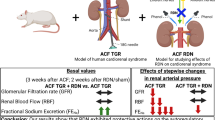
Basal calcium sensitization is decreased in spontaneously hypertensive rats, although their blood pressure (BP) response to acute Rho-kinase inhibition is enhanced. Using fasudil (Rho-kinase inhibitor) or nifedipine (L-VDCC blocker), we evaluated the contribution of calcium sensitization and calcium entry to BP maintenance in hypertensive transgenic Ren-2 rats (TGR) focusing on the influence of major vasoactive systems and/or baroreflex efficiency on BP responses to these two drugs. Homozygous TGR and normotensive Hannover Sprague-Dawley (HanSD) control rats aged 5, 11, or 22 weeks were used. The acute BP-lowering effects of fasudil or nifedipine were studied in intact rats, nitric oxide-deficient L-NAME-pretreated rats and rats subjected to combined blockade of the renin-angiotensin system (RAS), sympathetic nervous system (SNS) and nitric oxide synthase (NOS). Fasudil- or nifedipine-induced BP reduction increased during hypertension development in TGR. By contrast, the nifedipine-induced BP response decreased, whereas the fasudil-induced BP response increased with age in HanSD controls. Our data indicated a major contribution of nifedipine-sensitive calcium entry and relative attenuation of calcium sensitization in hypertensive rats compared with normotensive controls. The BP responses to fasudil or nifedipine were enhanced by NOS inhibition and combined blockade in normotensive HanSD rats but not in hypertensive TGR. In conclusion, calcium sensitization is attenuated by endogenous nitric oxide in normotensive HanSD rats but not in hypertensive TGR. Moreover, BP reduction elicited by acute Rho-kinase inhibition is partially compensated by enhanced sympathetic vasoconstriction. The decreased compensation in hypertensive rats with impaired baroreflex efficiency explains their greater BP response to fasudil than in normotensive animals.
Similar content being viewed by others
Introduction
Two important signaling pathways increase the level of phosphorylated myosin light chain (MLC), which is essential for the contraction of vascular smooth muscle (VSM) [1]. One pathway is based on the calcium/calmodulin activation of MLC kinase, leading to the increased formation of phosphorylated MLC. This pathway reflects calcium entry and/or calcium mobilization in VSM cells. The other pathway, called calcium sensitization, is based on the inhibition of MLC phosphatase, which attenuates MLC dephosphorylation through the activation of RhoA/Rho kinase and/or protein kinase C [2,3,4]. Although there are specific inhibitors of both pathways (calcium channel blockers and Rho kinase inhibitors), the evaluation of their particular contribution to VSM contraction and BP elevation under in vivo conditions is rather difficult [5].
The acute administration of drugs inhibiting either calcium entry through voltage-dependent calcium channels of the L type (L-VDCC) [6,7,8] or Rho kinase-based calcium sensitization [9,10,11,12,13,14] elicits a more pronounced BP reduction in hypertensive than in normotensive rats. However, it remains unclear whether greater BP reduction by the Rho kinase inhibitor fasudil is due to a reduction of enhanced calcium sensitization at normal calcium entry or a reduction of normal calcium sensitization at increased calcium entry. Of course, the same is also true for the enhanced BP response to the L-VDCC blocker nifedipine in hypertensive animals [5]. This was a reason why we determined basal calcium sensitization and calcium entry in conscious rats in which endogenous renin-angiotensin system (RAS) and sympathetic nervous system (SNS) were blocked [13]. Using this approach, reduced basal calcium sensitization together with increased basal calcium entry were demonstrated in spontaneously hypertensive rats (SHR), although the fasudil-induced BP decrease in intact SHR was augmented compared with their normotensive Wistar-Kyoto (WKY) controls [13]. Similar changes in calcium sensitization were also found in heterozygous Ren-2 transgenic rats with angiotensin II-dependent hypertension caused by the insertion of the murine renin gene [14].
Recently, we studied the development of fasudil-induced and nifedipine-induced BP changes in SHR and WKY aged 3–42 weeks [8]. The BP responses to either fasudil or nifedipine rose with hypertension development in SHR. Nevertheless, BP reduction elicited by fasudil in SHR was always smaller than that induced by nifedipine, whereas the reverse was true in age-matched WKY rats. This finding confirmed that calcium entry through L-VDCC plays a more important role in the development of genetic hypertension [8].
Major vasoactive systems, such as the renin-angiotensin system (RAS), sympathetic nervous system (SNS), and nitric oxide (NO), are supposed to participate in BP control by the modulation of calcium sensitization and calcium entry. Nitric oxide has been repeatedly reported to lower calcium sensitization in VSM [15, 16], but the information on the activating effects of major vasoconstrictor systems (RAS or SNS) is rather scarce [17,18,19,20]. Our previous study [21] in normotensive Wistar rats subjected to acute or chronic NO synthase inhibition confirmed the attenuation of calcium sensitization by NO. Additionally, we demonstrated the attenuation of calcium sensitization by chronic RAS blockade, suggesting the enhancing effect of endogenous angiotensin II. This study also revealed that the hypotensive action of fasudil evoked baroreflex activation leading to an increased heart rate (HR) and sympathetic nerve activity, which masked considerably the extent of fasudil-induced BP reduction in intact normotensive rats [21]. It should be mentioned that the baroreflex efficiency is usually substantially reduced in hypertensive rats compared with that in normotensive controls [22,23,24,25,26,27,28]. Similarly, the baroreflex efficiency is also markedly reduced in Ren-2 transgenic rats [29, 30].
The aim of the present study was to evaluate calcium sensitization and calcium entry using BP responses to fasudil or nifedipine found in homozygous Ren-2 transgenic rats with severe hypertension. Our attention was also focused on the development of these BP responses during postnatal ontogenesis and/or hypertension development (from prehypertensive 5-week-old rats up to animals with established hypertension aged 11 or 22 weeks). We also considered the influence of major vasoactive systems (NO, RAS, and SNS) on fasudil- or nifedipine-induced BP changes, as well as the impact of baroreflex-mediated compensatory enhancement of the heart rate and sympathetic vasoconstriction on the extent of the above BP responses in normotensive and hypertensive animals.
Methods
Animals
Male normotensive Hannover Sprague-Dawley (HanSD, −/−) controls and hypertensive homozygous (mRen-2)27 transgenic rats (TGR, +/+) aged 5, 11, and 22 weeks were obtained from the breeding facility of the Institute of Clinical and Experimental Medicine in Prague. They were housed at 23 °C under a 12-h light/dark cycle, were fed the Altromin diet (0.45% NaCl) and were given tap water ad libitum.
All the procedures and experimental protocols were approved by the Ethical Committee of the Institute of Physiology, Czech Academy of Sciences, and conformed to the European Convention on Animal Protection and Guidelines on Research Animal Use.
Experiments
One day prior to the experiment, two polyethylene cannulas were implanted under isoflurane anesthesia (PE 50 for BP measurement in the carotid artery, PE 10 for the infusion of drugs to the jugular vein); the cannulas were exteriorized in the interscapular region. The blood pressure was recorded using a pressure transducer and a multichannel recorder (ADInstruments, Bella Vista, Australia) in conscious animals placed in small plastic cages between 08:00 and 11:30 to reduce the circadian variations in BP levels.
Experiment 1—Time course of BP changes after intravenous and oral fasudil administration
Fasudil was administered intravenously or by oral gavage (10 mg/kg i.v. or 30 mg/kg p.o.) to 22-week-old TGR and HanSD rats. MAP and HR were monitored for 160 min at 5-min intervals.
Experiment 2—Ontogenetic changes in fasudil and nifedipine BP effects in intact animals
Following the 30-min stabilization period, cumulative doses of fasudil (Rho kinase inhibitor; 1, 2; 4 and again 4 mg/kg) or nifedipine (L-VDCC inhibitor; 0.05, 0.1, 0.2, and 0.4 mg/kg) were administered intravenously to control HanSD and homozygous TGR aged 5, 11, or 22 weeks. Thereafter, a single dose of nifedipine (0.75 mg/kg) in animals that had undergone fasudil dose-response administration or fasudil (10 mg/kg) in animals pretreated with nifedipine was administered. We also evaluated the fraction of BP reduction elicited by fasudil or nifedipine (given as the first drug) on the total BP change induced by the combination of both drugs to reveal the contribution of calcium sensitization and calcium entry to BP maintenance in TGR and their normotensive HanSD controls.
Experiment 3—Effects of major endogenous vasoactive systems on the contribution of calcium sensitization and calcium entry to BP maintenance
The blockade of major vasoconstrictor and vasodilator systems was performed in conscious animals according to the modified protocol of Minami et al. [31] that is regularly used in our laboratory [32, 33]. Briefly, after a 30-min stabilization period, the baseline levels of MAP and HR were recorded for 15 min. Next, the rats were subjected to either a separate blockade of NO synthase with L-NAME (30 mg/kg) or a combined blockade consisting of angiotensin converting enzyme inhibition (10 mg/kg captopril), ganglionic blockade (5 mg/kg pentolinium), and NO synthase inhibition (30 mg/kg L-NAME). Thereafter, the fasudil dose-response curve or nifedipine dose-response curve was determined (for concentrations of both drugs, see Experiment 2).
Drugs
All the drugs were obtained from Sigma, except for fasudil (HA-1077; LC Laboratories, Woburn, MA), and were usually dissolved in saline (nifedipine in 10 % DMSO) and administered as intravenous bolus injections (1 ml/kg).
Statistics
The data are presented as the means ± SEM. Two-way ANOVA was used to analyze the BP and HR responses to cumulative doses of fasudil or nifedipine with the grouping factor of strain or group treatment and factor of drug dose. The differences were considered significant at p < 0.05.
Results
First, we studied the time course and magnitude of the BP effects induced by fasudil administered by oral gavage or intravenous injection to adult homozygous TGR and HanSD rats aged 22 weeks (Fig. 1). TGR had a considerably higher mean arterial pressure (MAP) than HanSD rats (166 ± 7 vs. 114 ± 3 mmHg, p < 0.001). It is evident that the BP reduction elicited by fasudil was always greater in TGR than in HanSD controls, irrespective of route of fasudil administration (Fig. 1a, b). Although fasudil-induced BP change was substantially greater in TGR than in HanSD rats, HR acceleration was not proportional to the magnitude of the BP decrease in TGR (Fig. 1c, d).
Second, we compared the BP changes induced by acute Rho kinase inhibition or acute L-VDCC blockade in intact conscious rats aged 5, 11, and 22 weeks. Table 1 shows that MAP was similar in young TGR and HanSD rats aged 5 weeks, whereas hypertension was observed in adult homozygous TGR aged 11 or 22 weeks. The heart rate was significantly elevated in 5-week-old animals compared with that in the older groups, and prehypertensive TGR showed higher HR than age-matched HanSD rats (Table 1). The BP reduction elicited by acute administration of either fasudil or nifedipine (Fig. 2) was moderately enhanced already in prehypertensive TGR aged 5 weeks compared with that in age-matched HanSD controls. The BP changes induced by Rho kinase inhibition or L-VDCC blockade were augmented with increasing age and/or hypertension development in TGR, whereas only a moderate age-dependent increase in these BP changes was observed in normotensive HanSD rats (Fig. 2). The addition of nifedipine after the last fasudil dose elicited further BP reduction that was similar in both strains at all ages studied (Table 1). Fasudil given after nifedipine also caused further BP lowering that gradually increased with the age in both strains, being significantly enhanced in 22-week-old TGR (Table 1).
Development of the absolute MAP response to acute dose-dependent intravenous administration of fasudil (upper panels) or nifedipine (lower panels) to HanSD (−/−) rats and TGR (+/+) aged 5, 11, or 22 weeks. The data are expressed as the means ± SEM. N = 6–8 per group. Significant differences (p < 0.05) are indicated by x (HanSD vs. TGR)
To highlight the contribution of calcium sensitization or calcium entry to BP maintenance, we also expressed acute fasudil-induced and nifedipine-induced BP changes (ΔFAS, ΔNIF) in the percentage of the total BP response to both drugs administered to the same animal (ΔFAS + ΔNIF). The importance of calcium sensitization was increased with the age of HanSD rats, whereas the contribution of calcium entry was decreased in this rat strain (Table 1). By contrast, no such significant age-dependent changes in the contribution of calcium sensitization or calcium entry were observed in TGR. Thus, we observed a clear difference in the contribution of calcium sensitization or calcium entry to BP maintenance between normotensive and hypertensive rats. These rats differ especially in the role of calcium entry, which decreases with age in normotensive but not in hypertensive animals (Table 1).
Figures 3 and 4 show the influence of endogenous vasoactive systems on fasudil- or nifedipine-induced changes in BP and HR in 11-week-old rats (see Table 2 for basal MAP and HR values recorded prior to Rho kinase inhibition or L-VDCC blockade). Because the acute blockade of major vasoactive systems modified the BP and HR of both HanSD and TGR animals, we presented our results as relative BP and HR changes (in percentages of basal MAP and HR values recorded before the administration of fasudil or nifedipine). The acute inhibition of NO synthase by L-NAME increased BP and decreased HR in both strains (Table 2). Furthermore, NO synthase inhibition augmented substantially BP reduction induced by fasudil or nifedipine in HanSD rats but not in TGR (Fig. 3). However, HanSD rats are characterized by better baroreflex HR control than TGR animals because greater fasudil-induced BP reduction in TGR was accompanied by a smaller HR increase (Fig. 1). This was true both in the presence and absence of NO synthesis (Table 2). Therefore, the augmented fasudil-induced BP reduction in HanSD rats pretreated with L-NAME was accompanied by the enhanced HR increase compared with that in intact HanSD animals. Such changes were absent in TGR (Figs. 3 and 4). Thus, our data indicate that endogenous NO attenuates calcium sensitization and/or calcium entry in normotensive rats.
Influence of the acute blockade of NO synthase by L-NAME or the combined blockade of major vasoactive systems (RAS by captopril, SNS by pentolinium and NOS by L-NAME) on the relative MAP responses of TGR (+/+) and HanSD (−/−) rats to fasudil (left panels) or nifedipine (right panels) administration. The data are expressed as the means ± SEM. N = 7–9 per group. Significant differences (p < 0.05) are indicated by x (intact vs. NOS blockade), # (intact vs. complete blockade), and * (NOS blockade vs. complete blockade)
Influence of the acute blockade of NO synthase by L-NAME or the combined blockade of major vasoactive systems (RAS by captopril, SNS by pentolinium and NOS by L-NAME) on the relative HR responses of TGR (+/+) and HanSD (−/−) rats to fasudil (left panels) or nifedipine (right panels) administration. The data are expressed as the means ± SEM. N = 7–9 per group. Significant differences (p < 0.05) are indicated by x (intact vs. NOS blockade), # (intact vs. complete blockade), and * (NOS blockade vs. complete blockade)
If NO synthase inhibition was combined with acute blockade of RAS and SNS, the BP of HanSD rats became elevated, whereas that of TGR was decreased compared with that of intact animals of the respective rat strain (Table 2). The BP responses to fasudil or nifedipine in TGR subjected to combined blockade were similar to those seen in intact rats (Fig. 3), although they were not accompanied by a significant HR rise (Fig. 4). On the other hand, the combined blockade of RAS, SNS and NOS in HanSD rats caused further enhancement of fasudil-induced BP reduction but no significant changes in nifedipine-induced BP reductions (Fig. 3). The combined blockade (involving ganglionic blockade of the sympathetic and parasympathetic nervous systems) also caused substantial reduction in the efficacy of baroreflex HR control in HanSD rats (Fig. 4).
The most interesting finding was obtained by the comparison of absolute BP responses to fasudil (Fig. 5) or nifedipine (Fig. 6) in intact rats and rats subjected to combined blockade of major vasoactive systems (RAS, SNS and NOS) (see Table 2 for basal MAP and HR values). In intact rats, fasudil induced a much greater BP reduction in hypertensive TGR than in normotensive HanSD. This effect was accompanied by a steeper compensatory HR acceleration in HanSD than in TGR. On the other hand, in rats subjected to combined blockade, there was a major augmentation of the BP response to fasudil in HanSD, but not in TGR animals; thus, the BP reduction seen in HanSD rats surpassed that found in TGR (Fig. 5). The BP effects of nifedipine were also greater in intact TGR than in HanSD rats, but nifedipine-induced BP effects recorded after the combined blockade of major vasoactive systems were similar in both strains due to moderate enhancement of the BP response in HanSD rats (Fig. 6). Under the conditions of combined blockade of RAS, SNS, and NOS, the HR responses to fasudil or nifedipine administration were always substantially suppressed compared with those in intact animals (Table 2; Figs. 5 and 6).
Absolute MAP and HR changes induced by fasudil in intact HanSD (−/−) rats and TGR (+/+) and in rats subjected to combined blockade of major vasoactive systems (RAS, SNS, and NOS). The data are expressed as the means ± SEM. N = 7–9 per group. Significant differences (p < 0.05) are indicated by x (HanSD vs. TGR)
Absolute MAP and HR changes induced by nifedipine in intact HanSD (−/−) rats and TGR (+/+) and in rats subjected to the combined blockade of major vasoactive systems (RAS, SNS, and NOS). The data are expressed as the means ± SEM. N = 7–9 per group. Significant differences (p < 0.05) are indicated by x (HanSD vs. TGR)
Discussion
Our present study carried out in intact conscious rats revealed an exaggerated BP response to both the Rho kinase inhibitor fasudil and L-VDCC blocker nifedipine in hypertensive homozygous TGR compared with their normotensive HanSD controls. We also demonstrated that the augmentation of BP reduction induced by acute administration of either of these two drugs appeared in parallel with hypertension development. In normotensive HanSD rats, fasudil-induced BP reduction was greater than nifedipine-induced BP reduction, whereas such differences were not seen in TGR. Moreover, the fractional contribution of calcium entry to BP maintenance (%ΔNIF/(ΔNIF+ΔFAS) decreased with age in HanSD but not in TGR animals. Thus, our data suggest that hypertension development in TGR is associated with high calcium entry rather than with enhanced calcium sensitization. These findings resemble observations that we have made in the developing SHR in which the enhancement of calcium entry and attenuation of calcium sensitization were demonstrated compared with age-matched WKY rats [8]. Our present findings in hypertensive homozygous TGR agree with the increased calcium entry (through L-VDCC) and reduced Rho kinase-based calcium sensitization disclosed in heterozygous TGR or in SHR [13, 14].
We also tried to evaluate the influence of some endogenous vasoactive systems on calcium sensitization (BP response to fasudil) or calcium entry (BP response to nifedipine). It is evident that the acute blockade of NO synthase by L-NAME augmented the BP responses to fasudil or nifedipine, but this effect was significant only in HanSD rats. The attenuation of calcium sensitization and/or calcium entry by endogenous NO is in good agreement with our previous findings on the effects of acute or chronic NOS blockade on calcium sensitization in normotensive Wistar rats [21]. Greater attenuation of calcium sensitization and/or calcium entry by endogenous NO might be one of the explanations why the BP response to fasudil or nifedipine is smaller in intact normotensive HanSD rats than in hypertensive TGR. Indeed, Vaněčková et al. [34] reported a relative NO deficiency in TGR compared with that in HanSD rats, a finding that was also demonstrated in the present study (L-NAME-induced MAP increase—TGR +26 ± 2% vs. HanSD +36 ± 2%, p < 0.01).
The additional blockade of endogenous vasoconstrictor systems (SNS and RAS) in rats with suppressed NOS did not modify the BP response to fasudil in TGR, but it greatly enhanced this response in HanSD rats. Our previous results obtained in normotensive Wistar rats indicated that the acute ganglionic blockade by pentolinium, but not the acute inhibition of angiotensin converting enzyme by captopril, resulted in a major enhancement of the hypotensive effects of fasudil [21]. Fasudil- or nifedipine-induced BP decrease in intact normotensive rats activates baroreflex, leading to the increased heart rate and/or sympathetic vasoconstriction. It is well known that baroreflex efficiency is decreased in rats with various forms of experimental hypertension [22,23,24,25,26,27,28], including TGR [29, 30]. A lower baroreflex efficiency was also evident in our TGR animals. The heart rate increase in TGR following fasudil administration was similar to that seen in HanSD rats, although the magnitude of the fasudil-induced BP reduction was two fold greater in TGR compared with that in HanSD rats (Fig. 1). Thus, the enhanced MAP response to fasudil in normotensive HanSD rats subjected to ganglionic blockade offers another explanation for the different fasudil-induced BP responses of intact HanSD and TGR animals. A more efficient baroreflex control of the heart rate and/or sympathetic vasoconstriction in HanSD rats might compensate for a greater part of the elicited BP reduction in normotensive than in hypertensive rats (Figs. 3 and 4). Both suggested explanations of the smaller BP response to Rho kinase inhibition or L-VDCC blockade in normotensive rats seem to be plausible because simultaneous NOS inhibition together with substantial attenuation of the baroreflex operation by ganglionic blockade augmented fasudil- or nifedipine-induced BP responses of HanSD rats to the extent seen in hypertensive TGR (Figs. 5 and 6).
Conclusions
Both calcium entry and calcium sensitization play important roles in vascular contractility and blood pressure control. The augmented BP reduction elicited by the acute administration of either the Rho kinase inhibitor fasudil or L-VDCC blocker nifedipine, which appeared during hypertension development in TGR animals, might suggest the enhanced contribution of both calcium entry and calcium sensitization to high BP maintenance. However, the BP response of normotensive rats to fasudil was considerably higher than that elicited by nifedipine, whereas this finding was not seen in hypertensive rats. These findings indicate the important role of calcium entry and the relatively reduced importance of calcium sensitization in TGR compared with HanSD rats. The apparent discrepancy between the reduced calcium sensitization and enhanced BP response of hypertensive rats to fasudil might be ascribed to the minimal attenuation of calcium sensitization by endogenous NO and a lower baroreflex efficiency in TGR. By contrast, the BP response of normotensive HanSD rats to fasudil can be augmented substantially not only by acute NOS inhibition but also by ganglionic blockade, which abolishes the baroreflex-mediated enhancement of sympathetic vasoconstriction, compensating for fasudil-induced BP reduction. Thus, the observed differences in the BP responses to the acute Rho kinase inhibition or L-VDCC blockade between normotensive and hypertensive animals result from the different influences of endogenous NO as well as from the different efficiencies of baroreflex control of blood pressure. This might be of interest for clinical investigators because the same principles are probably true, even for human hypertension.
References
Himpens B, Matthijs G, Somlyo AV, Butler TM, Somlyo AP. Cytoplasmic free calcium, myosin light chain phosphorylation, and force in phasic and tonic smooth muscle. J Gen Physiol. 1988;92:713–29.
Somlyo AP, Somlyo AV. Signal transduction by G-proteins, rho-kinase and protein phosphatase to smooth muscle and non-muscle myosin II. J Physiol. 2000;522:177–85.
Loirand G, Sauzeau V, Pacaud P. Small G proteins in the cardiovascular system: physiological and pathological aspects. Physiol Rev. 2013;93:1659–720.
Loirand G. Rho kinases in health and disease: from basic science to translational research. Pharmacol Rev. 2015;67:1074–95.
Zicha J, Behuliak M, Pintérová M, Bencze M, Kuneš J, Vaněčková I. The interaction of calcium entry and calcium sensitization in the control of vascular tone and blood pressure of normotensive and hypertensive rats. Physiol Res. 2014;63:S19–27. Suppl 1
Takata Y, Howes LG, Hutchinson JS. Antihypertensive effect of diltiazem in young or adult rats of genetically hypertensive strains. Clin Exp Hypertens A. 1983;5:455–68.
Zicha J, Dobešová Z, Behuliak M, Pintérová M, Kuneš J, Vaněčková I. Nifedipine-sensitive blood pressure component in hypertensive models characterized by high activity of either sympathetic nervous system or renin-angiotensin system. Physiol Res. 2014;63:13–26.
Behuliak M, Vavřínová A, Bencze M, Polgárová K, Ergang P, Kuneš J, et al. Ontogenetic changes in contribution of calcium sensitization and calcium entry to blood pressure maintenance of Wistar-Kyoto and spontaneously hypertensive rats. J Hypertens. 2015;33:2443–54.
Uehata M, Ishizaki T, Satoh H, Ono T, Kawahara T, Morishita T, et al. Calcium sensitization of smooth muscle mediated by a Rho-associated protein kinase in hypertension. Nature. 1997;389:990–4.
Mukai Y, Shimokawa H, Matoba T, Kandabashi T, Satoh S, Hiroki J, et al. Involvement of Rho-kinase in hypertensive vascular disease: a novel therapeutic target in hypertension. FASEB J. 2001;15:1062–4.
Löhn M, Steioff K, Bleich M, Busch AE, Ivashchenko Y. Inhibition of Rho-kinase stimulates nitric oxide-independent vasorelaxation. Eur J Pharmacol. 2005;507:179–86.
Dhaliwal JS, Casey DB, Greco AJ, Badejo AM Jr, Gallen TB, Murthy SN, et al. Rho kinase and Ca2+ entry mediate increased pulmonary and systemic vascular resistance in L-NAME-treated rats. Am J Physiol Lung Cell Mol Physiol. 2007;293:L1306–13.
Behuliak M, Pintérová M, Bencze M, Petrová M, Líšková S, Karen P, et al. Ca2+ sensitization and Ca2+ entry in the control of blood pressure and adrenergic vasoconstriction in conscious Wistar-Kyoto and spontaneously hypertensive rats. J Hypertens. 2013;31:2025–35.
Behuliak M, Bencze M, Vaněčková I, Kuneš J, Zicha J. Basal and activated calcium sensitization mediated by RhoA/Rho kinase pathway in rats with genetic and salt hypertension. BioMed Res Int. 2017; Article ID80259728: 2017.
Sauzeau V, Le Jeune H, Cario-Toumaniantz C, Smolenski A, Lohmann SM, Bertoglio J, et al. Cyclic GMP-dependent protein kinase signaling pathway inhibits RhoA-induced Ca2+ sensitization of contraction in vascular smooth muscle. J Biol Chem. 2000;275:21722–9.
Chitaley K, Webb RC. Nitric oxide induces dilation of rat aorta via inhibition of Rho-kinase signaling. Hypertension. 2002;39:438–42.
Somlyo AP, Somlyo AV. Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev. 2003;83:1325–58.
Tsai MH, Jiang MJ. Rho-kinase-mediated regulation of receptor-agonist-stimulated smooth muscle contraction. Pflug Arch. 2006;453:223–32.
Jin L, Ying Z, Hilgers RH, Yin J, Zhao X, Imig JD, et al. Increased RhoA/Rho-kinase signaling mediates spontaneous tone in aorta from angiotensin II-induced hypertensive rats. J Pharmacol Exp Ther. 2006;318:288–95.
Hilgers RH, Todd J Jr, Webb RC. Increased PDZ-RhoGEF/RhoA/Rho kinase signaling in small mesenteric arteries of angiotensin II-induced hypertensive rats. J Hypertens. 2007;25:1687–97.
Brunová A, Bencze M, Behuliak M, Zicha J. Acute and chronic role of nitric oxide, renin-angiotensin system and sympathetic nervous system in the modulation of calcium sensitization in Wistar rats. Physiol Res. 2015;64:447–57.
Su DF, Cerutti C, Barrès C, Vincent M, Sassard J. Blood pressure and baroreflex sensitivity in conscious hypertensive rats of Lyon strain. Am J Physiol. 1986;251:H1111–7.
Nedvídek J, Zicha J. Age-dependent changes of baroreflex efficiency in Dahl rats: effects of high salt intake. Physiol Res. 1993;42:209–12.
Head GA. Baroreflexes and cardiovascular regulation in hypertension. J Cardiovasc Pharmacol. 1995;26:S7–16. Suppl 2
Lantelme P, Cerutti C, Lo M, Paultre CZ, Ducher M. Mechanisms of spontaneous baroreflex impairment in lyon hypertensive rats. Am J Physiol. 1998;275:R920–5.
Su DF, Miao CY. Arterial baroreflex function in conscious rats. Acta Pharmacol Sin. 2002;23:673–9.
Paton JF, Waki H, Abdala AP, Dickinson J, Kasparov S. Vascular-brain signaling in hypertension: role of angiotensin II and nitric oxide. Curr Hypertens Rep. 2007;9:242–7.
Mengal V, Silva PH, Tiradentes RV, Santuzzi CH, de Almeida SA, Sena GC, et al. Aliskiren and l-arginine treatments restore depressed baroreflex sensitivity and decrease oxidative stress in renovascular hypertension rats. Hypertens Res. 2016;39:769–76.
Borgonio A, Pummer S, Witte K, Lemmer B. Reduced baroreflex sensitivity and blunted endogenous nitric oxide synthesis precede the development of hypertension in TGR(mREN2)27 rats. Chronobiol Int. 2001;18:215–26.
Johnson MS, DeMarco VG, Heesch CM, Whaley-Connell AT, Schneider RI, Rehmer NT, et al. Sex differences in baroreflex sensitivity, heart rate variability, and end organ damage in the TGR(mRen2)27 rat. Am J Physiol Heart Circ Physiol. 2011;301:H1540–50.
Minami N, Imai Y, Hashimoto J, Abe K. Contribution of vascular nitric oxide to basal blood pressure in conscious spontaneously hypertensive rats and normotensive Wistar Kyoto rats. Clin Sci (Lond). 1995;89:177–82.
Kuneš J, Dobešová Z, Zicha J. Altered balance of main vasopressor and vasodepressor systems in rats with genetic hypertension and hypertriglyceridaemia. Clin Sci. 2002;102:269–77.
Vaněčková I, Dobešová Z, Kuneš J, Zicha J. The effects of repeated delivery of angiotensin II AT1 receptor antisense on distinct vasoactive systems in Ren-2 transgenic rats: young vs. adult animals. Hypertens Res. 2012;35:761–8.
Vaněčková I, Dobešová Z, Kuneš J, Vernerová Z, Zicha J. Endothelin A receptor blocker atrasentan lowers blood pressure by the reduction of nifedipine-sensitive calcium influx in Ren-2 transgenic rats fed a high-salt diet. J Hypertens. 2015;33:161–9.
Acknowledgements
This work was supported by a research grant of the Ministry of Health of the Czech Republic (15–25396A) and institutional support (RVO: 67985823).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vaněčková, I., Behuliak, M., Hojná, S. et al. Exaggerated blood pressure response to fasudil or nifedipine in hypertensive Ren-2 transgenic rats: role of altered baroreflex. Hypertens Res 42, 145–154 (2019). https://doi.org/10.1038/s41440-018-0146-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0146-x