Abstract
High sodium intake is a simple modifiable risk factor for hypertension. Although not confirmed, lower socioeconomic status may be a factor that increases sodium intake. We aimed to clarify the association between socioeconomic status and urinary sodium-to-potassium ratio by cross-sectional and longitudinal analyses. The study included 9410 community residents. Spot urine sodium-to-potassium ratios were measured twice with a 5-year interval. Socioeconomic status was investigated using a self-administered questionnaire. Cross-sectional analysis revealed that educational attainment was inversely associated with urinary sodium-to-potassium ratio (years of education ≤ 9: 3.0 ± 1.8, ≤ 12: 2.9 ± 1.6, ≥ 13: 2.8 ± 1.6; P < 0.001), whereas no significant association was observed with household income. Men, particularly individuals living alone, exhibited markedly high sodium-to-potassium ratios (3.6 ± 2.3). Although frequent intake of vegetables, fruits, and dairy products was also inversely associated with the ratio, the associations with educational attainment ( ≤ 9: reference, ≤ 12: β = −0.032, P = 0.026, ≥ 13: β = −0.059, P < 0.001), marital status (β = −0.040, P < 0.001), and sex*marital status interaction (β = 0.054, P = 0.001) were independent of these covariates. Educational attainment was also inversely associated with differences in the urinary sodium-to-potassium ratio during the follow-up period (odds ratio, 0.70; P < 0.001). Lower educational attainment was an independent determinant for urinary sodium-to-potassium ratio. Health literacy education, particularly in men living alone, may be a factor for reducing salt intake even in high-income countries where equal educational opportunity is assured.
Similar content being viewed by others
Introduction
Hypertension is a leading cause of cardiovascular events. High sodium intake is a simple modifiable risk factor for hypertension, as described previously, i.e., a positive association exists between urinary sodium excretion and blood pressure (BP) levels [1,2,3], particularly in individuals consuming high-sodium diets [4], as well as in the BP-lowering effect of sodium restriction interventions [5, 6]. Further, high sodium intake itself was suggested to increase the risk for cardiovascular events [7] and mortality [8], independently of BP levels. Therefore, determining factors that influence sodium intake may be helpful in preventing hypertension.
In addition to dietary factors, socioeconomic status (SES), namely, lower educational level and income, has been associated with higher sodium intake in various populations [9], including individuals in East Asian countries [10, 11] and Japan [12, 13], where the daily consumption of salt was higher than that in other high-income countries [14]. However, many of these studies investigated sodium intake using a questionnaire or by 24-h dietary recall, which may be less accurate than actual measurements. Furthermore, it is unclear whether SES influences sodium intake persistently beyond the intraindividual variations in sodium intake, although a nationwide study in Great Britain reported continued disparities in salt intake by SES even after the overall intake of salt declined by 0.9 g as a result of a national salt reduction program [15].
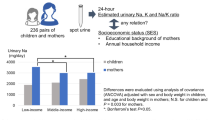
Daily salt intake can be most reliably estimated by measuring 24-h urinary sodium excretion. However, 24-h urine collection is inconvenient for participants and cannot be easily adapted for large-scale cohort studies. The sodium-to-potassium ratio (Na/K) of a urine sample is another index of salt loading. Given that the potassium excretion level is inversely associated with BP [4], the combined effect of lower potassium and higher sodium levels on BP appears to be greater than either alone [16, 17], as does the estimated daily salt intake by the Kawasaki [18] or Tanaka [19] formulas [2].
We aimed to clarify the associations between SES and urinary Na/K by cross-sectional and longitudinal settings using a dataset of the Nagahama Prospective Cohort for Comprehensive Human Bioscience (the Nagahama Study), a general population-based cohort study in Japan, where SES has not received as much attention as in Western countries, possibly because of equal educational opportunities in Japan [20].
Methods
Study participants
We analyzed the second visit dataset (follow-up measurement) describing participants in the Nagahama Study. Participants were recruited between 2008 and 2010 from the general population of Nagahama City, a rural city inhabited by 125,000 people located in central Japan. Community residents aged 30–74 years, living independently without any physical impairment or dysfunction, were eligible. Of the 9804 included participants, 14 withdrew consent and 26 were excluded because their genetic analysis demonstrated a different ethnic background. Among the remaining baseline population (n = 9764), 8289 participated in the second health survey performed 5 years after the baseline evaluation (2013–2015). By further recruiting 1561 participants meeting the inclusion criteria, the second visit dataset of the Nagahama Study comprised 9850 participants.
Individuals who were excluded from the analysis included women whose urinary Na and K levels were not measured because of menstruation (n = 373) or pregnancy (n = 9), individuals receiving hemodialysis therapy (n = 6), individuals with severe renal functional decline (estimated glomerular filtration rate [eGFR] < 30 ml/min/1.73 m2; n = 16), and individuals with incomplete clinical values or responses to the questionnaire administered (n = 36). In total, 9410 participants were ultimately included in the analysis.
All study procedures were approved by the ethics committee of the Kyoto University Graduate School of Medicine and the Nagahama Municipal Review Board. Written informed consent was obtained from all the participants.
Longitudinal analysis
Among 9410 participants, 7929 participated in the first visit (baseline) measurement between 2008 and 2010, with a 5-year interval between the two measurements. Individuals who met the same criteria (n = 7603) were included in the longitudinal analysis.
BP measurement
BP was measured after few minutes of resting in a sitting position using a standard cuff-oscillometric device (HEM-9000AI, Omron healthcare, Kyoto, Japan). BP was measured twice and the mean values were used for the analysis. Hypertension was defined as systolic BP ≥ 140 mm Hg, diastolic BP ≥ 90 mm Hg, and/or prescribed antihypertensive drugs.
Spot urine sample
Spot urine samples were collected at the first visit (0900–1700 h) and the second visit (0800– 400 h); urinary Na, K, and creatinine (Cr) levels were measured on each day of sampling. Time since the last meal was recorded for each participant.
Estimation of daily salt intake
Daily salt intake was estimated from spot urine Na and Cr values using the following formula [19]: 21.98 × {Na (mEq/l) × predicted 24-h Cr excretion/[Cr (mg/dl) × 10]}0.392 × 0.0585, where 24-h Cr excretion was predicted using the following formula: body weight (kg) × 14.89 + body height (cm) × 16.14−age × 2.04−2444.45.
Frequency of food consumption
Intake frequency of vegetables, fruits, and dairy products was queried using a self-administered questionnaire with the following choices: none, 1–3 times per month, 1 or 2 times per week, 3 or 4 times per week, 5 or 6 times per week, once daily, twice daily, or three or more times daily, and expressed as times per week consumed. Vegetable choices included cabbage, pumpkin, carrots, broccoli, green and yellow vegetables (e.g., spinach, and colza), and other green and yellow vegetables (e.g., bell pepper and common beans). Fruit choices included citrus fruits (e.g., oranges and grapefruit) and other fruits (e.g., strawberries, kiwi, apples, and watermelons). Dairy product choices included milk and yogurt.
Basic clinical parameters
Basic clinical parameters (including plasma markers) used in this study were obtained at the first and the second visits. Renal function was assessed by eGFR, calculated using the following formula: 194 × Cr−1.094 × age−0.287 × 0.739 [if female] [21]. Years of education, household income, family members, and medication history were assessed using a structured self-administered questionnaire. Nine education years corresponded to a junior high school graduate, whereas 12 education years corresponded to a high school graduate.
Statistical analysis
Group differences in numeric variables were assessed using analysis of variance, whereas frequency differences were assessed using the chi-squared test. Factors independently associated with urinary electrolytes were analyzed using a linear regression or a logistic regression model. Statistical analyses were performed using the JMP version 13.1.0 software (SAS Institute, Cary, NC, USA). P < 0.05 was considered statistically significant.
Results
Clinical characteristics of the study participants are presented in Table 1. Spot urine Na/K was slightly lower at follow-up (−0.33 ± 2.15), possibly because of a higher frequency of fasting individuals ( ≥ 12 h; follow-up: 79.2%, baseline: 47.1%). A national trend toward decreasing salt intake, as well as increased frequency of participants taking antihypertensive drugs, which may enhance consciousness of salt restriction, might be another reason.
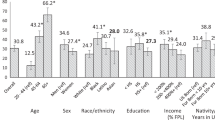
Associations between socioeconomic factors and spot urine Na/K
Differences in urinary Na/K based on educational attainment are indicated in Fig. 1. Urinary Na/K was inversely associated with years of education in both crude analysis (Fig. 1a) and major covariate-adjusted analysis (Fig. 1b). Although several factors differed significantly based on years of education (Table 2), educational attainment was identified as a significant inverse determinant for urinary Na/K after adjustment for the covariates, including brachial BP and use of antihypertensive drugs (Table 3). When regression analysis was performed separately by antihypertensive medication status, the inverse association was significant only in individuals not taking drugs ( ≥ 13 years: β = −0.067, P = 0.001, ≤ 12 years: β = −0.026, P = 0.152), but not in the treated hypertensives ( ≥ 13 years: β = −0.025, P = 0.332, ≤ 12 years: β = −0.028, P = 0.121). In this regression model, frequent intake of vegetables, fruits, and dairy products was also identified as an independent inverse determinant, whereas no significant association was observed with household income.
Differences in urinary Na/K at the follow-up measurement based on educational attainment and presence of a live-in spouse. Values are crude or adjusted means. Numbers of study participants in each subgroup are indicated in the column. Statistical significance was assessed by (a) analysis of variance; (b, d) linear regression model adjusted for age, sex, and body mass index; and (c) two-way analysis of variance
In the separate analysis for Na and K (Table 3), educational attainment exhibited an opposite association with Na/Cr and K/Cr. Other factors, namely, body mass index (BMI) and food consumption also exhibited the opposite association. The results of the regression analysis were thus clearer in the analysis for Na/K than for the separate components.
Absence of a live-in spouse was another factor that was strongly associated with urinary Na/K in men, but not in women (Fig. 1c and 1d) possibly because of the positive association with the K/Cr level (Table 3). The results of the multivariate model (Table 3) identified the absence of a live-in spouse and its interaction with sex as a significant determinant for Na/K independent of the major covariates, including food consumption frequency.
Association of educational attainment with estimated daily salt intake
Mean estimated daily salt intake at the follow-up investigation was 9.3 ± 2.1 g. Regression analysis adjusted for the same covariates listed in Table 3 failed to identify educational attainment as a significant determinant for the estimated daily salt intake ( ≥ 13 years: β = −0.012, P = 0.425, ≤ 12 years: β = 0.009, P = 0.546).
Associations among social factors, urinary Na/K, and BP
Spot urine Na/K was positively associated with systolic (β = 0.162, P < 0.001) and diastolic BP (β = 0.117, P < 0.001), even in an analysis adjusted for the major covariates, including age, sex, BMI, eGFR, antihypertensive medication, and fasting time. The odds ratio of one unit increase in Na/K for hypertension was 1.18 (95% CI, 1.15−1.22, P < 0.001) in the adjusted analysis. However, educational attainment (Table 2) and marital status (systolic: P = 0.295, diastolic: P = 0.114) were not directly associated with hypertension.
Changes in spot urine Na/K and educational attainment
When years of education obtained at the follow-up measurement was extrapolated to the baseline, the inverse association between educational attainment and urinary Na/K was replicated in the baseline dataset (age, sex, BMI, eGFR, and fasting time-adjusted model: ≤ 12 years: β = −0.046, P = 0.002, ≥ 13 years: β = −0.118, P < 0.001). Furthermore, educational attainment exhibited a significant inverse association with the differences in urinary Na/K during the follow-up period (Fig. 2), irrespective of the strong inverse association between baseline Na/K and the differences in follow-up Na/K (r = −0.668, P < 0.001).
Odds ratio for the highest quartiles of changes in urinary Na/K between baseline and follow-up values are adjusted odds ratios and 95% confidence intervals. Adjusted factors were sex, fasting time at the follow-up investigation, and the following parameters at baseline: age, body mass index, systolic blood pressure, use of antihypertensive drugs, fasting time, and urinary Na/K. Statistical significance was assessed by the logistic regression model. The number of study participants in each subgroup is indicated in parentheses
Discussion
In this large general population-based study, we determined that lower educational attainment was an independent positive determinant for spot urine Na/K even in a country where at least 9 years of education is compulsory and where the majority of the nation completes 12 years of school [20]. Older individuals are less likely to have attained higher educational levels, and the results of our previous descriptive epidemiology indicated an inverse association between age and urinary Na/K [2]. However, the association between educational attainment and Na/K was independent of age, suggesting the importance of health literacy education in addition to general education to maintain satisfactory salt intake.
We analyzed a spot urine Na/K that was susceptible to clinical and environmental factors, such as renal function and fasting conditions, as shown in our previous report [2]. However, the inverse association between education attainment and urinary Na/K was independent of these covariates and was replicated in the analysis using the baseline dataset. Furthermore, we also demonstrated an inverse association between educational attainment and 5-year longitudinal changes in Na/K, irrespective of the strong confounding of the regression to the mean effect, i.e., if the Na/K is high upon first measurement, it will tend to be closer to the average upon second measurement without any intervention. These results indicated that the present findings are not just an epiphenomenon caused by confounding of other relevant clinical factors and that the findings may represent the persistent effect of educational attainment on salt intake.
The inverse association between education attainment and urinary Na/K was also independent of brachial BP and antihypertensive medication. As several antihypertensive drugs such as diuretics and blockers of renin–angiotensin system might influence urinary Na/K, we further performed a separate analysis and found the inverse association only in individuals not taking antihypertensive drugs. However, this result should be carefully considered because the treated individuals were older and thus more likely to have fewer years of education. The results of the regression analysis in the treated individuals might be therefore somewhat underestimated. Another reason for the possible underestimation might be insufficient statistical power due to the relatively small number of participants taking antihypertensive drugs. Further studies in hypertensive patients are needed to clarify this issue.
A clear association was not observed between educational attainment and estimated daily salt intake. As years of education was inversely associated with Na/Cr and positively associated with K/Cr, Na/K might be a more susceptible marker of salt loading in relation to the educational attainment. Inaccuracy in estimation of salt intake might be another reason.
Consumption of foods containing large amounts of potassium, namely, vegetables, fruits, and dairy products, was inversely associated with urinary Na/K, similar to previous findings [22] even in the analysis based on frequency data rather than amount data. Interestingly, consumption of these foods was also associated with educational attainment independent of the major covariates. Educational attainment may be associated with urinary Na/K by directly influencing sodium intake and indirectly modulating dietary habits.
Several studies have investigated differences in salt intake based on marital status. A population-based study in Italy [23] as well as a nationwide study in Japan [13] reported significantly lower sodium intake in individuals living alone, though a British study reported a lack of association [24]. In our study, we found higher urinary Na/K in men, particularly in those without a live-in spouse. An explanation for the inconsistent results may be that using Na/K as an index of salt intake in this study was different compared with previous studies, which estimated sodium intake by urinary Na level. The results of our regression analysis that demonstrated a positive association between marital status and K/Cr, but not Na/K support this consideration. Given the present findings, as well as a known relevant association between lower potassium intake and hypertension, living alone may be an overlooked risk factor for hypertension when salt intake is assessed by urinary Na alone. However, we did not consider occupational status or type of job, which has been previously suggested as a reason for higher salt intake [10, 23, 24]. As solitary eating has also been suggested as a factor for unfavorable eating behavior [25], further investigations considering these cofounding factors will help clarify reasons for the differences in urinary Na/K based on sex and marital status and provide a hint for reducing salt intake in men.
In contrast, no significant association was observed based on household income. Although the reasons for inconsistency are unclear, previous studies reported lower salt intake [12] and higher potassium intake [26] in individuals with higher incomes. A possible reason may be the difference in study settings, i.e., the present study is based on individuals who live in a specific geographic area. A large study including various populations may identify an inequality of urinary Na/K based on household income.
An advantage of this study is the large population size with repeated measurements of urinary Na/K after 5 years. This clarifies the persistent association between educational attainment and urinary Na/K. There are several limitations that require mentioning. First, spot urine samples may not always represent the daily salt intake of the study participants. Second, several samples were obtained under nonfasting conditions, although a previous study reported a diurnal variation in urinary Na/K [27]. We therefore adjusted the fasting time in the regression analyses. Third, we investigated socioeconomic factors using a questionnaire, which may contain potential misclassification. However, any misreporting occurs independently of the urinary Na/K and thus will not cause serious bias. Fourth, we did not consider changes in SES during the follow-up period in the longitudinal analysis, although there might be some changes in the household income and family members, changes in educational attainment are unlikely. There may be confounding of potential changes in SES, particularly changes in the family members, in the results of the longitudinal analysis.
In conclusion, we clarified that lower educational attainment was independently associated with spot urine Na/K. The present results support the importance of health literacy education, particularly in men without a spouse, even in high-income countries where educational opportunity is assured.
References
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. BMJ. 1988;297:319–28.
Tabara Y, Takahashi Y, Kumagai K, Setoh K, Kawaguchi T, Takahashi M, et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: the Nagahama study. J Hypertens. 2015;33:2407–13.
Han W, Han X, Sun N, Chen Y, Jiang S, Li M. Relationships between urinary electrolytes excretion and central hemodynamics, and arterial stiffness in hypertensive patients. Hypertens Res. 2017;40:746–51.
Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–11.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomized trials. BMJ. 2013;346:f1325.
O’Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–38.
O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–23.
de Mestral C, Mayén AL, Petrovic D, Marques-Vidal P, Bochud M, Stringhini S. Socioeconomic determinants of sodium intake in adult populations of high-income countries: a systematic review and meta-analysis. Am J Public Health. 2017;107:e1–e12.
Hong JW, Noh JH, Kim DJ. Factors associated with high sodium intake based on estimated 24-hour urinary sodium excretion: the 2009–11 Korea national health and nutrition examination survey. Medicine. 2016;95:e2864.
Chien KL, Hsu HC, Chen PC, Su TC, Chang WT, Chen MF, et al. Urinary sodium and potassium excretion and risk of hypertension in Chinese: report from a community-based cohort study in Taiwan. J Hypertens. 2008;26:1750–6.
Miyaki K, Song Y, Taneichi S, Tsutsumi A, Hashimoto H, Kawakami N, et al. Socioeconomic status is significantly associated with dietary salt intakes and blood pressure in Japanese workers (J-HOPE Study). Int J Environ Res Public Health. 2013;10:980–93.
Uechi K, Asakura K, Masayasu S, Sasaki S. Within-country variation of salt intake assessed via urinary excretion in Japan: a multilevel analysis in all 47 prefectures. Hypertens Res. 2017;40:598–605.
Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813.
Ji C, Cappuccio FP. Socioeconomic inequality in salt intake in Britain 10 years after a national salt reduction programme. BMJ Open. 2014;4:e005683.
Morris RC Jr, Sebastian A, Forman A, Tanaka M, Schmidlin O. Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension. 1999;33:18–23.
Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356:1966–78.
Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20:7–14.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Jayaweera S. Gender and access to education in Asia. Int Rev Educ. 1987;33:455–66.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Taylor EN, Stampfer MJ, Mount DB, Curhan GC. DASH-style diet and 24-hour urine composition. Clin J Am Soc Nephrol. 2010;5:2315–22.
Cappuccio FP, Ji C, Donfrancesco C, Palmieri L, Ippolito R, Vanuzzo D, et al. Geographic and socioeconomic variation of sodium and potassium intake in Italy: results from the MINISAL-GIRCSI programme. BMJ Open. 2015;5:e007467.
Ji C, Kandala NB, Cappuccio FP. Spatial variation of salt intake in Britain and association with socioeconomic status. BMJ Open. 2013;3:e002246.
Tani Y, Kondo N, Takagi D, Saito M, Hikichi H, Ojima T, et al. Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: results of the JAGES. Appetite. 2015;95:1–8.
Si Hassen W, Castetbon K, Cardon P, Enaux C, Nicolaou M, Lien N, et al. Socioeconomic indicators are independently associated with nutrient intake in French adults: a DEDIPAC study. Nutrients. 2016;8:158.
Iwahori T, Ueshima H, Torii S, Saito Y, Kondo K, Tanaka-Mizuno S, et al. Diurnal variation of urinary sodium-to-potassium ratio in free-living Japanese individuals. Hypertens Res. 2017;40:658–64.
Acknowledgements
We are extremely grateful to the Nagahama City Office and the nonprofit organization Zeroji Club for their support in performing the Nagahama Study. The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
The study was supported by a university grant, The Center of Innovation Program, The Global University Project, and a Grant-in-Aid for Scientific Research (25293141, 26670313) from the Ministry of Education, Culture, Sports, Science & Technology in Japan, the Practical Research Project for Rare/Intractable Diseases (ek0109070, ek0109196), the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D (dk0207006), the Program for an Integrated Database of Clinical and Genomic Information (kk0205008) from Japan Agency for Medical Research and Development (AMED), and the Takeda Medical Research Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yamashita, M., Tabara, Y., Higo, Y. et al. Association between socioeconomic factors and urinary sodium-to-potassium ratio: the Nagahama Study. Hypertens Res 41, 973–980 (2018). https://doi.org/10.1038/s41440-018-0101-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0101-x
Keywords
This article is cited by
-
Sodium-to-potassium ratio and renal functional decline
Hypertension Research (2024)
-
The spot urine sodium-to-potassium ratio as a marker of hypertension risk
Hypertension Research (2022)
-
Parental educational status independently predicts the risk of prevalent hypertension in young adults
Scientific Reports (2021)
-
Sodium/potassium ratio change was associated with blood pressure change: possibility of population approach for sodium/potassium ratio reduction in health checkup
Hypertension Research (2021)
-
Urinary sodium/potassium ratio as a screening tool for hyperaldosteronism in men with hypertension
Hypertension Research (2021)