Abstract
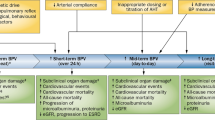
The definition of diurnal blood pressure changes varies widely, which can be confusing. Short-term blood pressure variability during a 24-h period and the dipping status of diurnal blood pressure can be captured by ambulatory blood pressure monitoring, and these metrics are reported to have prognostic significance for cardiovascular complications. Morning blood pressure surge also indicates this risk, but its effect may be limited to populations with specific conditions. Meanwhile, the combined use of conventional office blood pressure and out-of-office blood pressure allows us to identify people with white-coat and masked hypertension. Current home devices can measure nocturnal blood pressure during sleep more conveniently than ambulatory monitoring; however, we should pay attention to blood pressure measurement conditions regardless of whether they are in a home, ambulatory, or office setting. The relatively poor reproducibility of diurnal blood pressure changes, including the nocturnal fall of blood pressure, is another underestimated issue to be addressed. Although information on diurnal blood pressure changes is expected to be used more effectively in the future, we should also keep in mind that blood pressure levels have remained central to the primary and secondary prevention of blood pressure-related cardiovascular diseases in clinical practice.
Similar content being viewed by others
Introduction
Blood pressure changes consist of the frequency components of various cycles, from beat-to-beat changes measured by a continuous intraarterial approach to seasonal or yearly blood pressure changes captured based on a continual blood pressure measurement (Table 1). Of the several sorts of blood pressure measurements in clinical practice that can capture these variability components, ambulatory blood pressure monitoring at intervals of 10–30 min within 24 h typically allow us to evaluate diurnal blood pressure changes [1,2,3], whereas home blood pressure is a convenient and reliable measurement to capture morning and evening blood pressure levels for several days or more [4]. Recently, nighttime blood pressure during sleep can also be evaluated by self-intended home measurement under standardized conditions [5,6,7]. The usefulness of conventional office blood pressure should not be underestimated regarding the identification of white-coat and masked hypertension [8, 9]. In this review, we provide an overview of the impact of diurnal blood pressure changes on cardiovascular complications in relation to ambulatory, home, and conventional blood pressure measurements.
Short-term blood pressure variability during a 24-h period
The Ohasama research group investigated the prognostic significance of reading-to-reading blood pressure variability to cardiovascular mortality in a general population [1]. Based on daytime ambulatory blood pressure monitoring, the greater the SD of systolic blood pressure, the higher the risk of cardiovascular mortality with a significant linear trend (P = 0.03) [1]. Such a trend was not observed for nighttime ambulatory blood pressure (P = 0.40), whereas residents with the highest quintile of blood pressure variability had a significantly high risk of cardiovascular death compared with the lowest risk group (daytime: hazard ratio [HR], 2.51; 95% confidence interval [CI], 1.10–5.70.; nighttime: HR, 2.21; 95% CI, 1.11–4.43) [1]. In the International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO), which consists of participants from Europe, Asia, and Latin America, blood pressure variability represented by SD and average real variability (ARV) in 24-h ambulatory monitoring was also assessed [2]. The ARV averages the absolute differences of consecutive measurements [10], and therefore, we can account for the order in which blood pressure measurements are obtained by using ARV. When multivariable-adjusted Cox regression models were applied, systolic blood pressure variability did not predict cardiovascular mortality when represented by the SD of 24-h recordings (HR per 1-SD increment, 1.03; 95% CI, 0.93–1.03), SD of the daytime (HR, 1.05; 95% CI, 0.95–1.17), but it was predicted by ARV (HR, 1.17; 95% CI, 1.07–1.28) [2]. Although the predictive power of ARV for cardiovascular events was marginal (HR, 1.07; 95% CI, 1.00–1.14), ARV contributed only <1% to the prediction of cardiovascular risk [2].
Among 508 patients aged ≥65 years old in the Second Australian National Blood Pressure study, daytime and weighted 24-h blood pressure variability were significantly associated with total mortality regardless of systolic or diastolic blood pressure (P ≤ 0.04), but nighttime blood pressure variability was not (P ≥ 0.13) [11]. For cardiovascular death, only weighted systolic blood pressure variability was a significant but marginal predictor (HR, 1.09; 95% CI, 1.00–1.19) [11]. A large dataset of hypertensive patients, the Ambulatory Blood Pressure-International study (ABP-International) [12], reported that the SD of nighttime blood pressure was strongly associated with an increased risk of cardiovascular events (HR per 10-mmHg increments in SD, 1.48; 95% CI, 1.20–1.84), although the SD of daytime blood pressure was not (HR, 1.05, 95% CI, 0.84–1.33). When the SD of nighttime systolic/diastolic blood pressure variability was treated dichotomously, the SD of variabilities ≥12.2/≥7.9 mmHg was associated with a 41/48% greater risk of cardiovascular events (95% CI, 18–68/22–78%). As the ABP-International investigators concluded [12], the addition of blood pressure variability to survival models may improve the risk stratification of patients with hypertension defined by standard clinical and laboratory variables. However, this approach is not always applicable, such as the SD of daytime blood pressure in IDACO [2] and the ABP-International [12]. It is important to bear in mind that the 24-h blood pressure level is the main driver for risk assessment in clinical practice.
Daytime and nighttime blood pressure—dipper and non-dipper
The highest blood pressures are commonly seen during morning hours, whereas the lowest are seen during sleep; however, some patients have elevated blood pressure throughout the night [13, 14]. In 1988, O’Brien and colleagues reported for the first time that an abnormal circadian blood pressure profile, which is the blood pressure difference between mean daytime and nighttime measurements, was <10/<5 mmHg, and these individuals had a more frequent history of stroke;[14] these individuals were named non-dippers [14]. The current generally accepted definition is that an individual with a nocturnal blood pressure drop of below 10% compared with daytime blood pressure is called a non-dipper, whereas an individual with a nocturnal blood pressure drop of >10% is called a dipper [15, 16]. Furthermore, patients with a nocturnal blood pressure drop ≥20% are called extreme dippers, whereas those with a higher nocturnal blood pressure than a daytime blood pressure (night-to-day blood pressure ratio value of ≥1) are called reverse dippers (also called inverted dippers or risers) [15, 16]. Both systolic and diastolic blood pressure components should be referenced to define the dipping pattern [17]. The term “non-dipper” has therefore two meanings, that is, it refers to people with a nocturnal blood pressure drop of 0–10% and those with a drop ≤10%, including the riser pattern, in its limited and broad definition, respectively.
The pathophysiological aspects of the dipping pattern of diurnal blood pressure have been investigated. Briefly, Imai and colleagues first reported that nocturnal blood pressures did not fall nor rise in comparison with daytime blood pressure levels in patients with Cushing’s syndrome [18], and more widely, among patients receiving glucocorticoid therapy [19]. This impairment persisted after remission following surgery for hypercortisolism and was partially ameliorated after 3 years of follow-up [20]. Circadian blood pressure variation is mediated by the hypothalamo–pituitary–adrenal axis through its action on the autonomic nervous system [19], which is also the case in insular cortex atrophy [21]. Melatonin also influences the dipping pattern of blood pressure [22, 23], which might be mediated by rhythmic secretion from the pineal gland. The clinical factors that are associated with non-dippers or risers are aging [24,25,26], smoking habits [26], diabetes mellitus [27], antihypertensive drug treatment [24], low kidney function [28, 29], previous renal [30], or cardiac [27] transplantation, and obstructive sleep apnea syndrome [13, 31, 32].
Independent of blood pressure levels, the dipping pattern has a prognostic ability for cardiovascular complications. In the Ohasama study, a 5% or more drop in nocturnal blood pressure compared with daytime blood pressure was associated with an 18% (95% CI, 7–28%) greater risk of cardiovascular mortality [33]. The updated Ohasama report indicated that residents with a riser pattern in which daytime and nighttime intervals were defined by diary cards had a higher risk of cardiovascular mortality than those who were dippers (people with a nocturnal blood pressure drop of 10–19%) over a median follow-up period of 18.3 years (HR, 2.31; 95% CI, 1.47–3.62) [34]. The IDACO investigators reported that participants with the riser pattern of diurnal blood pressure were older, had a history of diabetes mellitus and previous cardiovascular complications more frequently than those without a riser pattern [24]. In regard to prognostic significance, riser participants had significantly higher risks of cardiovascular mortality (HR, 1.45; 95% CI, 1.02–2.02) and composite cardiovascular events (HR, 1.30; 95% CI, 1.04–1.62), but these risks were not significant in non-dippers based on the limited meaning (nocturnal blood pressure fall of 0–10%) nor in extreme dippers [24]. When the night-to-day blood pressure difference was represented as a ratio, the ratios were inconsistent predictors of the combined fatal and nonfatal cardiovascular outcomes in multivariable-adjusted models, including 24-h blood pressure levels (HR per 1-SD systolic blood pressure ratio increase, 1.05; 95% CI, 0.98–1.11, and HR on diastolic pressure, 1.07; 95% CI, 1.00–1.13), although the ratios were consistent predictors of total mortality (P < 0.001) [24]. Part of this association might reflect reverse causality; for instance, daytime physical inactivity might result in a comparably weak nocturnal blood pressure fall [35]. An insufficient duration of action of antihypertensive drug agents may result in inadequate blood pressure control, particularly during the night, which also leads to less pronounced nocturnal blood pressure dipping. To reach the same conclusion as that stated in the “short-term blood pressure variability” section, an assessment of blood pressure during the whole day should be standard in clinical practice [35, 36].
Morning blood pressure surge
Although the incidence of cardiovascular disease increases in the morning [37], the risk of morning blood pressure surge based on 24-h ambulatory monitoring has been a matter of discussion [3, 38, 39]. Based on magnetic resonance imaging, Kario and colleagues assessed the impact on morning surge for silent cerebral infarction among 529 elderly patients with hypertension (mean age, 72 years; 64% women) and reported that patients in the top tenth of the sleep-trough (morning systolic blood pressure minus the lowest pressure during the night) morning surge distribution had a higher baseline prevalence of multiple infarcts and stroke incidence compared with the remaining 90% of patients (57% vs 33% and 19% vs 7.3%, respectively; P ≤ 0.004) [3]. A 10-mmHg increase in sleep-trough morning surge increased stroke risk by 22% (P = 0.008), and the corresponding increase in pre-awakening (morning minus preawake blood pressure) morning blood pressure surge resulted in a 14% stroke risk increment with marginal significance (P = 0.07) [3]. Among 507 untreated patients with hypertension in a Bordeaux cohort (mean age, 49 years; 36% women), the estimated risk increase of cardiovascular complications per 1-mmHg increase in pre-awakening morning blood pressure surge was 3.3% (95% CI, 0.8–5.8%) [40]. In the Ohasama study (n = 1430; mean age, 61 years; 64% women; 27% with antihypertensive drug treatment) [38], the predictive power of pre-awakening morning surge in systolic blood pressure was marginal for cerebral hemorrhage (HR per 1-SD increase [+13.8 mmHg], 1.34; 95% CI, 0.95–1.89), and not for ischemic stroke (HR, 0.97; 95% CI, 0.79–1.19). In a categorical analysis when the lowest risk group was set as a reference, a significantly high risk of intracerebral hemorrhage was observed in the top quintile of the pre-awakening morning surge group with a wide CI ( ≥25 mmHg of the systolic blood pressure change; HR, 3.97; 95% CI, 1.08–14.63) and in the top quintile of the sleep-trough morning surge group (≥40 mmHg; HR, 8.88; 95% CI, 1.14–69.2). Risk of total stroke, including cerebral infarction, was not associated with any sort of morning surge in this population [38]. In the IDACO population (mean age, 53 years; 54% women), the HRs expressing the risk of total mortality and cardiovascular events in the top tenth of the sleep-trough morning surge distribution (≥37.0 mmHg) amounted to 1.32 (95% CI, 1.09–1.59) and 1.30 (95% CI, 1.06–1.60), respectively, compared with the overall risk in the whole study population [41]. The corresponding HRs for risk of total mortality and cardiovascular events in the top tenth of the pre-awakening morning surge (≥28.0 mmHg) were 1.23 (95% CI, 1.00–1.51) and 1.45 (1.17–1.80), respectively [41]. Among the 2051 participants of the Pressioni Arteriose Monitorate E Loro Associazioni (PAMELA) study (mean age, 51 years; 50% women; 19% with antihypertensive drug treatment) [42], cardiovascular mortality showed no significant relation to sleep-trough and pre-awakening morning systolic blood pressure surge (HR, 0.93 and 0.87, respectively; P ≥ 0.16), and no differences in the risks of total and cardiovascular mortality were observed when the bottom versus top deciles of the distributions of the sleep-trough and pre-awakening morning systolic blood pressure were compared (P ≥ 0.39).
The Progetto Ipertensione Umbria Monitoraggio Ambulatoriale (PIUMA) study [39] offers a key to understanding the controversy regarding morning blood pressure surge. In this Italian population with untreated hypertension (mean age, 51 years; 46% women), neither patients with a high sleep-trough (>36.0 mmHg; the highest quartile) nor those with a high pre-awakening (>27.5 mmHg) systolic blood pressure had increased risks of death and cardiovascular events [39]. In contrast, both a blunted sleep-trough (≤19.5 mmHg; the lowest quartile) and a blunted pre-awakening (≤9.5 mmHg) blood pressure surge were significantly associated with cardiovascular events (HRs, 1.66 and 1.71, respectively; P ≤ 0.013) [39]. This finding can be partly explained by the relationship between dipping pattern and morning surge in individuals; the reduction in systolic blood pressure from day to night, representing the dipping pattern, showed a statistically significant direct association with the sleep-trough and pre-awakening systolic blood pressure surge (Fig. 1; P < 0.0001). Although the relationship differs from person to person, the risk of non-dipper or riser and that of morning surge are mutually incompatible according to Fig. 1. Because the aforementioned evidence supports the essentially high risk among people with the riser blood pressure pattern, it is no exaggeration to state that morning blood pressure surge is not a dominant risk factor in general; it can be a risk among those with exaggerated morning surge, that is, the top quintile [38] or decile [41], for specific population characteristics [3] or in assessing limited outcomes [38]. It may be worth pointing out, in passing, that the risk of morning blood pressure surge cannot be substituted with morning hypertension, particularly hypertension in the morning based on self-measured home blood pressure [4, 43, 44]. Although this topic is irrelevant to the main subject of this review, we would like to emphasize the essential risk of morning hypertension.
Direct association between the reduction in systolic blood pressure from day to night, which denotes the dipping pattern, with the sleep-trough (left panel) and pre-awakening (right panel) morning blood pressure surge. The solid lines denote the 95% confidence ellipse. Reproduced from Verdecchia et al. [39]
Use of conventional blood pressure in diurnal blood pressure
Although increased attention is being paid to out-of-office blood pressure readings [45] and despite that the reliability of the prognostic significance of out-of-office blood pressures has been steadily confirmed [4, 8, 46], clinical decision making is still mainly based on conventional office blood pressure. Unlike treatments based on out-of-office blood pressure, we have extensive evidence on the beneficial effect of conventional blood pressure lowering treatments for cardiovascular diseases [47]. Nevertheless, as proposed by recent guidelines [15, 45], we should actively use ambulatory and home blood pressures because the exclusive use of conventional blood pressure would result in failure to recognize white-coat hypertension, which should be carefully monitored [8, 48,49,50], and more importantly, it would result in failure to identify masked hypertension, which should be considered to be associated with a similar degree of risk as sustained hypertension [8, 49, 51, 52].
Vast evidence supports the view that masked hypertension carries a cardiovascular risk comparable to or at least only slightly lower than sustained hypertension in which both office and out-of-office blood pressures are high [9, 49, 51]. Even among individuals with an optimal or normal office blood pressure, those with masked hypertension, irrespective of an ambulatory-based [52] or home-based [8] diagnosis, have a ≈2-fold increase in the risk of cardiovascular complications. Recently, the Ohasama study group classified their study participants as to whether they had office, home, and/or 24-h ambulatory hypertension (Table 2) [9]. When multivariable-adjusted models were applied, home hypertension without 24-h ambulatory hypertension and 24-h ambulatory hypertension without home hypertension were significantly associated with a higher risk of stroke than that found in the sustained normotension group (Fig. 2; P ≤ 0.04). This finding expands on the IDACO report by showing that masked hypertension represents a constantly high risk during any part of the “out-of-office” measurement period, that is, daytime, nighttime, and 24-h periods and a combination of these time periods (Fig. 3; HR between 1.76–2.03; P ≤ 0.0001) [49]. Antihypertensive treatment aimed at normalizing conventional office blood pressure while ignoring out-of-office blood pressure may increase the percentage of patients with masked uncontrolled hypertension [53, 54]. We need to capture out-of-office blood pressure in individuals, specifically, both home and 24-h ambulatory blood pressure measurements [9], to evaluate cardiovascular risk more accurately.
Adjusted hazard ratios among groups according to home hypertension and 24-h ambulatory hypertension. Filled squares express hazard ratios for stroke and are sized in proportion to the number of events observed among hypertension groups. The covariates were sex, age, body mass index, current smoking, alcohol consumption, diabetes mellitus, total cholesterol, history of cardiovascular disease, and the use of antihypertensive drugs. The thresholds for the cross-classification of blood pressure are summarized in Table 2. The + mark indicates hypertension. *P < 0.05, †P < 0.0001 versus the sustained normal blood pressure (SNBP) group. MHT masked hypertension, SHT sustained hypertension, WCHT white-coat hypertension. Reproduced from Satoh et al. [9]
Risk of a cardiovascular end point associated with white-coat and masked hypertension vs stringently defined normotension as defined by various intervals of ambulatory monitoring. In this analysis, the most stringent definition of normotension was applied as a unique reference in which the conventional blood pressure was normal and the ambulatory blood pressure was within normal limits for 24 h plus daytime and nighttime periods. Hazard ratios express the risk compared with normotension and were adjusted for sex, age, body mass index, smoking, drinking, total cholesterol, diabetes mellitus, history of cardiovascular disease, and cohort. Horizontal bars denote the 95% confidence interval of the hazard ratios. Reproduced from Asayama et al. [49]
In contrast to the constantly high risk of masked hypertension, whether white-coat hypertension is a dominant risk factor for cardiovascular diseases is still under debate [55,56,57,58]. Because white-coat hypertension is a heterogeneous condition [59], extracting the genuine effect of white-coat hypertension from various confounding factors is mandatory for assessing risk. For instance, the prevalence of white-coat hypertension exponentially increased across increasing age groups, ranging from 2.2% for ages 18–30 to 19.5% for individuals aged ≥70 years, with little sex differences [60]. The duration of the follow-up period also affects risk estimation—the HRs associated with white-coat hypertension in IDACO participants were 1.08 (P = 0.79), 1.20 (P = 0.29), and 1.30 (P = 0.043) for follow-up periods censored at 6, 9, and 12 years, respectively [51]. Moreover, part of the ambulatory measurement period affects the risk of white-coat hypertension, which is different from masked hypertension as aforementioned [49]; in IDACO, HRs associated with white-coat hypertension progressively weakened (Fig. 3) from daytime and nighttime only (1.38 and 1.43, respectively; P ≤ 0.033) to 24 h plus daytime and nighttime (1.16; P = 0.41) [49]. This finding endorses the importance of full 24-h recordings of ambulatory blood pressure in the identification of white-coat hypertension. To the best of our knowledge, there is no randomized controlled trial comparing the outcome between patients with white-coat hypertension and those with normotension, and whether patients with white-coat hypertension would benefit from antihypertensive treatment also remains unclear [61]. Although current insights are mainly based on observational studies, we again emphasize the importance of capturing blood pressure information in various settings. Individuals who are normotensive based on whole in-office and out-of-office blood pressures are associated with the lowest cardiovascular risk.
Nocturnal blood pressure measurement by home devices
Recent advances in technology have enabled the measurement of nocturnal blood pressures with home devices [62]. Although nocturnal blood pressures during sleep cannot be self-measured in a narrow sense, the measurement of nocturnal home blood pressure is based on the agreement of participants themselves to undergo automatic blood pressure measurements during sleep, regardless of them being asleep or awake at the time of measurement, by home devices that can self-measure blood pressure during the daytime. Our research group initially reported the first data based on a home blood pressure device. The device was equipped with a timer that automatically measured blood pressure at 0200 h and stored the reading on its memory chip [5]. The average nocturnal systolic blood pressure of patients increased in proportion to the degree of the three-graded sleep disturbance, that is, from “no sleep disturbance and no awareness of measurement”, “mild sleep disturbance with an awareness of measurement”, to “serious sleep disturbance” (from 116.1 ± 10.9 mmHg to 121.7 ± 15.5 mmHg; P < 0.001) [5]. Cumulative evidence has suggested that nocturnal home blood pressure levels were associated with indices of preclinical target organ damage (i.e., left ventricular mass index [6, 63, 64] and common carotid intima-media thickness [63, 64]), which is similar to associations in nocturnal ambulatory monitoring. Although only two studies [6, 63] were combined in this recent meta-analysis, the study further reported that nocturnal home blood pressure was superior to nocturnal ambulatory blood pressure in its relationship to urinary albumin excretion (P < 0.01 for comparison) [7]. As stated in a recent review, cost-effective, adequate control of nocturnal blood pressure during sleep is of marked clinical relevance [65]. Compared with ambulatory blood pressure monitoring, which has been limited by various practical and economic concerns [66], the measurement of home nocturnal blood pressures could be an advance for clinical practice. Nocturnal home blood pressures might represent a new chapter in the search for reliable and consistent blood pressure measurements and recordings of diurnal blood pressure changes.
Perspectives
Sheng and colleagues reported that environmental factors, such as the combination of daily temperature and season, explain ≈8% and ≈3%, respectively, of the dipping status and morning blood pressure surge, whereas genetic cues explain only ≈1% of these diurnal changes in models [67]. As they concluded, environmental factors are substantially strong drivers of diurnal blood pressure rhythmicity [67]. We emphasize the importance of capturing information on measurement conditions, such as the use of a diary, a thermo-logger or actigraphy, to record body position and physical activity. It should be, furthermore, noted that the reproducibility of diurnal blood pressure changes, including the nocturnal fall of blood pressure, is comparably poor [68,69,70,71,72], and this inconvenient truth is also applicable to home blood pressure measurements [5, 73]. For instance, we reported that the correlation of nocturnal home blood pressures between two sessions with an average interval of 5.9 days was modest (r = 0.67/0.55 in systolic/diastolic blood pressure), and the SD of the difference was large (≥13.6/≥9.3 mmHg), even after taking into account the degree of sleep disturbance [73]. Although self-measurement of home blood pressure is highly reproducible [62], further improvements are needed to perform automatic blood pressure measurements during sleep by home devices.
Although wide variations in the definition of diurnal blood pressure changes may be confusing, we can conclude that blood pressure levels remain central to the primary and secondary prevention of blood pressure-related cardiovascular diseases. Regardless of time periods and blood pressure measurement information, such as daytime or nighttime periods and ambulatory, home, or conventional office measurements, respectively, controlling blood pressure levels within a normal range is a top-priority issue in clinical practice. Chronotherapy of blood pressure [74], which can be used to adjust the administration of antihypertensive drugs according to diurnal blood pressure changes, may be an effective approach once blood pressure control is adequately achieved [75, 76]. However, as the Monitorización Ambulatoria para Predicción de Eventos Cardiovasculares (MAPEC) study failed to demonstrate the significance of the therapeutic effect of controlling SD in 24-h (48-h) ambulatory recordings [77] and morning blood pressure surges [65, 77], there is little evidence supporting the efficacy of chronotherapy for blood pressure in terms of cardiovascular outcomes [24]. We call for additional large, international population studies and randomized clinical trials with hard endpoints to define the potential application of diurnal blood pressure changes.
References
Kikuya M, Hozawa A, Ohkubo T, Tsuji I, Michimata M, Matsubara M, Ota M, Nagai K, Araki T, Satoh H, Ito S, Hisamichi S, Imai Y. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000;36:901–6.
Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. Prognostic value of reading-to-reading blood pressure variability over 24 h in 8938 subjects from 11 populations. Hypertension. 2010;55:1049–57.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–10.
Chonan K, Kikuya M, Araki T, Fujiwara T, Suzuki M, Michimata M, Hashimoto J, Ohkubo T, Hozawa A, Yamamoto N, Miyawaki Y, Matsubara M, Imai Y. Device for the self-measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit. 2001;6:203–5.
Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K, Japan Morning Surge-Home Blood Pressure Study Investigators G. Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension. 2012;60:921–8.
Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens. 2017;35:442–52.
Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, Aparicio LS, Hara A, Johansson JK, Ohkubo T, Tzourio C, Stergiou GS, Sandoya E, Tsuji I, Jula AM, Imai Y, Staessen JA. International Database of Home Blood Pressure in Relation to Cardiovascular Outcome investigators. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med. 2014;11:e1001591.
Satoh M, Asayama K, Kikuya M, Inoue R, Metoki H, Hosaka M, Tsubota-Utsugi M, Obara T, Ishiguro A, Murakami K, Matsuda A, Yasui D, Murakami T, Mano N, Imai Y, Ohkubo T. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension. 2016;67:48–55.
Mena L, Pintos S, Queipo NV, Aizpurua JA, Maestre G, Sulbaran T. A reliable index for the prognostic significance of blood pressure variability. J Hypertens. 2005;23:505–11.
Chowdhury EK, Wing LMH, Jennings GLR, Beilin LJ, Reid CM, Committee AM. Visit-to-visit (long-term) and ambulatory (short-term) blood pressure variability to predict mortality in an elderly hypertensive population. J Hypertens. 2017;36:1059–67. https://doi.org/10.1097/HJH.0000000000001652.
Palatini P, Reboldi G, Beilin LJ, Casiglia E, Eguchi K, Imai Y, Kario K, Ohkubo T, Pierdomenico SD, Schwartz JE, Wing L, Verdecchia P. Added predictive value of night-time blood pressure variability for cardiovascular events and mortality: the ambulatory blood pressure-international study. Hypertension. 2014;64:487–93.
Pickering TG. The clinical significance of diurnal blood pressure variations. Dippers and nondippers. Circulation. 1990;81:700–2.
O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2:397.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y, European Society of Hypertension Working Group on Blood Pressure M. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
O’Brien E, Parati G, Stergiou G. Response to: nocturnal blood pressure dipping: systolic, diastolic or both? J Hypertens. 2014;32:700–1.
Imai Y, Abe K, Sasaki S, Minami N, Nihei M, Munakata M, Murakami O, Matsue K, Sekino H, Miura Y, Yoshinaga K. Altered circadian blood pressure rhythm in patients with Cushing’s syndrome. Hypertension. 1988;12:11–19.
Imai Y, Abe K, Sasaki S, Minami N, Munakata M, Nihei M, Sekino H, Yoshinaga K. Exogenous glucocorticoid eliminates or reverses circadian blood pressure variations. J Hypertens. 1989;7:113–20.
Pecori Giraldi F, Toja PM, De Martin M, Maronati A, Scacchi M, Omboni S, Cavagnini F, Parati G. Circadian blood pressure profile in patients with active Cushing’s disease and after long-term cure. Horm Metab Res. 2007;39:908–14.
Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K. Insular cortex atrophy as an independent determinant of disrupted diurnal rhythm of ambulatory blood pressure in elderly hypertension. Am J Hypertens. 2009;22:723–9.
Grossman E, Laudon M, Zisapel N. Effect of melatonin on nocturnal blood pressure: meta-analysis of randomized controlled trials. Vasc Health Risk Manag. 2011;7:577–84.
Zeman M, Dulkova K, Bada V, Herichova I. Plasma melatonin concentrations in hypertensive patients with the dipping and non-dipping blood pressure profile. Life Sci. 2005;76:1795–803.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Wang J, Sandoya E, O’Brien E, Staessen JA. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Kobrin I, Oigman W, Kumar A, Ventura HO, Messerli FH, Frohlich ED, Dunn FG. Diurnal variation of blood pressure in elderly patients with essential hypertension. J Am Geriatr Soc. 1984;32:896–9.
Cai A, Zhong Q, Liu C, Zhou D, Li X, Zhang Y, Feng Y, Zhou Y. Associations of systolic and diastolic blood pressure night-to-day ratios with atherosclerotic cardiovascular diseases. Hypertens Res. 2016;39:874–8.
Reeves RA, Shapiro AP, Thompson ME, Johnsen AM. Loss of nocturnal decline in blood pressure after cardiac transplantation. Circulation. 1986;73:401–8.
Nakai K, Fujii H, Watanabe K, Watanabe S, Awata R, Kono K, Yonekura Y, Goto S, Nishi S. Riser pattern is a predictor of kidney mortality among patients with chronic kidney disease. Clin Exp Hypertens. 2016;38:476–81.
Wang C, Zhang J, Liu X, Li C, Ye Z, Peng H, Chen Z, Lou T. Reversed dipper blood-pressure pattern is closely related to severe renal and cardiovascular damage in patients with chronic kidney disease. PLoS ONE. 2013;8:e55419.
Azancot MA, Ramos N, Moreso FJ, Ibernon M, Espinel E, Torres IB, Fort J, Seron D. Hypertension in chronic kidney disease: the influence of renal transplantation. Transplantation. 2014;98:537–42.
Stergiou GS, Triantafyllidou E, Cholidou K, Kollias A, Destounis A, Nasothimiou EG, Markozannes E, Alchanatis M. Asleep home blood pressure monitoring in obstructive sleep apnea: a pilot study. Blood Press Monit. 2013;18:21–26.
Kario K. Obstructive sleep apnea syndrome and hypertension: ambulatory blood pressure. Hypertens Res. 2009;32:428–32.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Satoh M, Asayama K, Kikuya M, Inoue R, Tsubota-Utsugi M, Obara T, Murakami K, Matsuda A, Murakami T, Nomura K, Metoki H, Imai Y, Ohkubo T. Nocturnal blood pressure decline based on different time intervals and long-term cardiovascular risk: the Ohasama Study. Clin Exp Hypertens. 2018;40:1–7.
Stolarz-Skrzypek K, Thijs L, Richart T, Li Y, Hansen TW, Boggia J, Kuznetsova T, Kikuya M, Kawecka-Jaszcz K, Staessen JA. Blood pressure variability in relation to outcome in the International Database of Ambulatory blood pressure in relation to Cardiovascular Outcome. Hypertens Res. 2010;33:757–66.
Asayama K, Wei FF, Hara A, Hansen TW, Li Y, Staessen JA. Prognosis in relation to blood pressure variability: con side of the argument. Hypertension. 2015;65:1170–9.
Muller JE, Stone PH, Turi ZG, Rutherford JD, Czeisler CA, Parker C, Poole WK, Passamani E, Roberts R, Robertson T, Sobel BE, Willerson JT, Braunwald E. The Multicenter Investigation of the Limitation of Infarct Size (MILIS) Study Group. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313:1315–22.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006;47:149–54.
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, Ambrosio G, Reboldi G. Day-night dip and early-morning surge in blood pressure in hypertension: prognostic implications. Hypertension. 2012;60:34–42.
Gosse P, Lasserre R, Minifie C, Lemetayer P, Clementy J. Blood pressure surge on rising. J Hypertens. 2004;22:1113–8.
Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, Metoki H, Ohkubo T, Torp-Pedersen C, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Sandoya E, Kawecka-Jaszcz K, Ibsen H, Imai Y, Wang J, Staessen JA. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8.
Bombelli M, Fodri D, Toso E, Macchiarulo M, Cairo M, Facchetti R, Dell’Oro R, Grassi G, Mancia G. Relationship among morning blood pressure surge, 24-hour blood pressure variability, and cardiovascular outcomes in a white population. Hypertension. 2014;64:943–50.
Asayama K, Ohkubo T, Kikuya M, Obara T, Metoki H, Inoue R, Hara A, Hirose T, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y. Prediction of stroke by home “morning” versus “evening” blood pressure values: the Ohasama study. Hypertension. 2006;48:737–43.
Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, Kobayashi F, Shimada K. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–96.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr., Williamson JD, Wright JT Jr.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71:1269–324. https://doi.org/10.1161/HYP.0000000000000065.
Kikuya M, Hansen TW, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10-year cardiovascular risk. Circulation. 2007;115:2145–52.
Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–15.
Franklin SS, Thijs L, Hansen TW, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59:564–71.
Asayama K, Thijs L, Li Y, Gu YM, Hara A, Liu YP, Zhang Z, Wei FF, Lujambio I, Mena LJ, Boggia J, Hansen TW, Bjorklund-Bodegard K, Nomura K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Stolarz-Skrzypek K, Malyutina S, Casiglia E, Nikitin Y, Lind L, Luzardo L, Kawecka-Jaszcz K, Sandoya E, Filipovsky J, Maestre GE, Wang J, Imai Y, Franklin SS, O’Brien E, Staessen JA, International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension. 2014;64:935–42.
Ugajin T, Hozawa A, Ohkubo T, Asayama K, Kikuya M, Obara T, Metoki H, Hoshi H, Hashimoto J, Totsune K, Satoh H, Tsuji I, Imai Y. White-coat hypertension as a risk factor for the development of home hypertension: the Ohasama study. Arch Intern Med. 2005;165:1541–6.
Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7030 individuals. J Hypertens. 2007;25:1554–64.
Brguljan-Hitij J, Thijs L, Li Y, Hansen TW, Boggia J, Liu YP, Asayama K, Wei FF, Bjorklund-Bodegard K, Gu YM, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Katarzyna SS, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang J, O’Brien E, Staessen JA. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcome Investigators. Risk stratification by ambulatory blood pressure monitoring across JNC classes of conventional blood pressure. Am J Hypertens. 2014;27:956–65.
Franklin SS, O’Brien E, Staessen JA. Masked hypertension: understanding its complexity. Eur Heart J. 2017;38:1112–8.
Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, Asayama K, Bjorklund-Bodegard K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. International Database on Ambulatory blood pressure in Relation to Cardiovascular Outcomes Investigators. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61:964–71.
Asayama K, Li Y, Franklin SS, Thijs L, O’Brien E, Staessen JA. Cardiovascular risk associated with white-coat hypertension: con side of the argument. Hypertension. 2017;70:676–82.
Mancia G, Bombelli M, Cuspidi C, Facchetti R, Grassi G. Cardiovascular risk associated with white-coat hypertension: pro side of the argument. Hypertension. 2017;70:668–75.
Huang Y, Huang W, Hu Y. Is white-coat hypertension associated with risk of cardiovascular diseases? J Am Coll Cardiol. 2017;69:2880.
Franklin SS, Thijs L, Staessen JA. Reply: is white-coat hypertension associated with risk of cardiovascular diseases? J Am Coll Cardiol. 2017;69:2880–1.
Mancia G, Grassi G. The heterogeneous nature of white-coat hypertension. J Am Coll Cardiol. 2016;68:2044–6.
Conen D, Aeschbacher S, Thijs L, Li Y, Boggia J, Asayama K, Hansen TW, Kikuya M, Bjorklund-Bodegard K, Ohkubo T, Jeppesen J, Gu YM, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Schoen T, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Mena L, Maestre GE, Filipovsky J, Imai Y, O’Brien E, Wang JG, Risch L, Staessen JA. Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension. 2014;64:1073–9.
Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, Huang H, Zeng J, Hu Y, Xu D. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35:677–88.
Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, Tsuchihashi T, Ohkubo T, Kuwajima I, Miyakawa M. The Japanese Society of Hypertension guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res. 2012;35:777–95.
Andreadis EA, Agaliotis G, Kollias A, Kolyvas G, Achimastos A, Stergiou GS. Night-time home versus ambulatory blood pressure in determining target organ damage. J Hypertens. 2016;34:438–44.
Lindroos AS, Johansson JK, Puukka PJ, Kantola I, Salomaa V, Juhanoja EP, Siven SS, Jousilahti P, Jula AM, Niiranen TJ. The association between home vs. ambulatory night-time blood pressure and end-organ damage in the general population. J Hypertens. 2016;34:1730–7.
Hermida RC, Ayala DE, Smolensky MH, Fernandez JR, Mojon A, Portaluppi F. Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks. Hypertens Res. 2016;39:277–92.
Head GA. The importance and prognostic value of nocturnal blood pressure assessments using inexpensive domestic devices. J Hypertens. 2017;35:463–5.
Sheng CS, Cheng YB, Wei FF, Yang WY, Guo QH, Li FK, Huang QF, Thijs L, Staessen JA, Wang JG, Li Y. Diurnal blood pressure rhythmicity in relation to environmental and genetic cues in untreated referred patients. Hypertension. 2017;69:128–35.
Omboni S, Parati G, Palatini P, Vanasia A, Muiesan ML, Cuspidi C, Mancia G. Reproducibility and clinical value of nocturnal hypotension: prospective evidence from the SAMPLE study. Study on ambulatory monitoring of pressure and lisinopril evaluation. J Hypertens. 1998;16:733–8.
Thijs L, Amery A, Clement D, Cox J, de Cort P, Fagard R, Fowler G, Guo C, Mancia G, Marin R, O’Brien E, O’Malley K, Palatini P, Parati G, Petrie J, Ravogli A, Rosenfeld J, Staessen J, Webster J. Ambulatory blood pressure monitoring in elderly patients with isolated systolic hypertension. J Hypertens. 1992;10:693–9.
Hinderliter AL, Routledge FS, Blumenthal JA, Koch G, Hussey MA, Wohlgemuth WK, Sherwood A. Reproducibility of blood pressure dipping: relation to day-to-day variability in sleep quality. J Am Soc Hypertens. 2013;7:432–9.
Palatini P, Mormino P, Canali C, Santonastaso M, De Venuto G, Zanata G, Pessina AC. Factors affecting ambulatory blood pressure reproducibility. Results of the HARVEST Trial. Hypertension and Ambulatory Recording Venetia Study. Hypertension. 1994;23:211–6.
Mochizuki Y, Okutani M, Donfeng Y, Iwasaki H, Takusagawa M, Kohno I, Mochizuki S, Umetani K, Ishii H, Ijiri H, Komori S, Tamura K. Limited reproducibility of circadian variation in blood pressure dippers and nondippers. Am J Hypertens. 1998;11:403–9.
Hosohata K, Kikuya M, Ohkubo T, Metoki H, Asayama K, Inoue R, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Reproducibility of nocturnal blood pressure assessed by self-measurement of blood pressure at home. Hypertens Res. 2007;30:707–12.
Scarpelli PT, Gallo M, Chiari G. Chronobiology of blood pressure. J Nephrol. 2000;13:197–204.
Hermida RC, Ayala DE, Fernandez JR, Mojon A, Smolensky MH. Hypertension: new perspective on its definition and clinical management by bedtime therapy substantially reduces cardiovascular disease risk. Eur J Clin Invest. 2018;48:e12909 https://doi.org/10.1111/eci.12909.
Roush GC, Fapohunda J, Kostis JB. Evening dosing of antihypertensive therapy to reduce cardiovascular events: a third type of evidence based on a systematic review and meta-analysis of randomized trials. J Clin Hypertens (Greenwich). 2014;16:561–8.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011;58:1165–73.
Acknowledgements
We acknowledge the Editorial Board of Hypertension Research for giving the authors the opportunity to publish this article.
Funding
KA received research support from Omron Healthcare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Asayama, K., Satoh, M. & Kikuya, M. Diurnal blood pressure changes. Hypertens Res 41, 669–678 (2018). https://doi.org/10.1038/s41440-018-0054-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0054-0
This article is cited by
-
Self-measured home blood pressure highlights cardiovascular risk in women: the HOMED-BP study
Hypertension Research (2023)
-
Impacts of the urinary sodium-to-potassium ratio, sleep efficiency, and conventional risk factors on home hypertension in a general Japanese population
Hypertension Research (2021)
-
Effects of white-coat, masked and sustained hypertension on coronary artery stenosis and cardiac arrhythmia
Hypertension Research (2020)
-
The dawning of the digital era in the management of hypertension
Hypertension Research (2020)
-
White-coat and masked hypertension and coronary artery disease: are they related or not?
Hypertension Research (2020)