Abstract
Arterial stiffness is an important risk factor for cardiovascular morbidity and mortality in patients with end-stage renal disease (ESRD). Arterial stiffness aggravates cardiovascular risk via multiple pathways, such as augmentation of aortic systolic pressure, subendocardial hypoperfusion, and excess pulsatile energy transmission from macro- to microcirculation. Pathogenesis of the arteriosclerotic process in ESRD is complex and not yet fully understood. Several factors unique to ESRD, such as mineral metabolism disturbances, vascular calcifications, formation of advanced glycation end-products, and acute and chronic volume overload, are proposed to play a particular role in the progression of arteriosclerosis in ESRD. As these and other mechanistic pathways of arterial stiffening in ESRD are elucidated, there is hope that this knowledge will be translated into novel therapeutic interventions targeting arterial stiffness. In the meantime, blood pressure (BP) lowering via strict volume control and appropriate use of antihypertensive drugs is a fundamental step in reversing accelerated arterial stiffening and modifying the cardiovascular risk profile of ESRD patients. In this article, we review the pathogenesis, clinical epidemiology, and therapies targeting arterial stiffness in ESRD, discussing recent advances and high-priority goals of future research in these important areas.
Similar content being viewed by others
Introduction
People with end-stage renal disease (ESRD) have one of the highest rates of cardiovascular morbidity and mortality [1, 2]. Although atherosclerotic arterial disease is undoubtedly involved in the causal pathway of excess cardiovascular risk, the spectrum of arterial remodeling in ESRD is broader, also including the long-term process of arteriosclerosis [3]. Arterial stiffening is another major contributor to the heightened cardiovascular risk in ESRD, causing hemodynamic alterations via multiple pathways. Arterial stiffness augments systolic pressure and pulse pressure (PP) in the ascending aorta, increases left ventricular (LV) afterload and promotes the adverse myocardial remodeling towards hypertrophy and fibrosis [4, 5]. Moreover, excessive pulsatile energy transmission from macro- to microcirculation as a result of the preferential stiffening of the aorta promotes microvascular damage in peripheral organs and tissues [4,5,6]. Therefore, it is not surprising that arterial stiffness is a powerful predictor of mortality [7, 8].
Arteriosclerosis is a pathophysiological continuum that occurs in early stage chronic kidney disease (CKD), and this process is progressively enhanced in parallel with renal function decline [9,10,11]. Although the mechanistic background of arterial stiffening is not yet fully clear, it seems likely that pathways closely related to ESRD, such as volume overload, mineral metabolism disturbances, vascular calcifications, formation of advanced glycation end-products (AGEs), inflammation and oxidative stress, are prominent mediators of arteriosclerosis [3, 12]. As ongoing research sheds more light on these complex mechanistic pathways, there is hope that this knowledge would be translated into novel therapeutic interventions targeting the regression of arteriosclerosis. In this article, we discuss the pathogenesis, clinical epidemiology, and treatment of arterial stiffness in ESRD, providing an overview of recent advances in these important areas and highlighting the aspects that should become high-priority goals of future research.
Pathogenesis of arterial stiffness in ESRD
The main roles of the aorta and large central arteries are (1) to dampen the high-pressure oscillations generated from the intermittent LV ejection and (2) to transform the cyclic blood flow in the aorta into a continuous capillary flow pattern required for the perfusion of organs and tissues [4, 13,14,15]. During systole, the stroke volume ejected by left ventricle interacts with elastic properties of the aorta to generate a pulse wave (incident or forward traveling) that is propagated at a pulse wave velocity (PWV) that progressively increases across the arterial tree. The structure of the arterial system is normally characterized by a progressive increase in arterial wall rigidity from the ascending aorta to the peripheral muscular-type arteries (i.e., stiffness gradient) [4, 13,14,15]. Impendence mismatches at the transition between these segments generate wave reflections. These reflected waves travel from the periphery back to the ascending aorta (backward-traveling reflected wave), opposing pulsatile energy transmission downstream to microcirculation. In young people with elastic arteries, this process is coupled with slower pulse wave propagation, and the overlap of the incident and reflected waves in the ascending aorta occurs in late systole or early diastole (Fig. 1). This phenomenon results in a rise of diastolic aortic pressure, favoring coronary perfusion during diastole. The arteriosclerotic process, however, preferentially affects the aortic wall, reversing the normal stiffness gradient. In clinical conditions of increased arterial stiffness, there is premature arrival of the reflected wave back to the ascending aorta during systole rather than diastole of the next cardiac cycle. This results in augmentation of central aortic systolic pressure, thereby increasing LV afterload and promoting adverse myocardial remodeling [4, 13,14,15]. In addition, excess pulsatile energy transmission from macro- to microcirculation promotes microvascular damage in peripheral vascular beds [4, 13,14,15].
Overlap of forward- and backward-traveling pulse waves in the ascending aorta. Under physiological conditions (i.e., in young subjects with elastic central arteries), the reflected pulse wave returns to the ascending aorta during late systole or diastole of the next cardiac cycle. In patients with stiff central arteries (i.e., in the elderly or in patients with end-stage renal disease), the reversal of the stiffness gradient between central and peripheral arterial segments and faster propagation of pulse waves results in premature arrival of the backward-traveling pulse wave during systole rather diastole, leading to augmentation of aortic systolic pressure
Arterial stiffening is a BP-dependent process. In essential hypertension, the severity of arterial stiffness is at least partially determined by the level of distending BP imposed on the arterial wall [13, 16]. In the long term, arterial remodeling in essential hypertension is principally characterized by arterial wall thickening. Alterations in the intrinsic arterial wall properties are also occurring in young hypertensives, but they are not the principal mode of remodeling [17]. The concept, however, is different in ESRD. Comparative case control studies have shown that ESRD patients have significantly higher aortic PWV levels than age-, sex- and BP-matched hypertensive controls with normal renal function [18, 19]. This accelerated arterial stiffening in ESRD is because in this setting, vascular remodeling is attributed to modification of the viscoelastic properties of the biomaterial constituting the arterial wall [18, 19]. In other words, arterial stiffness in ESRD is characterized by an increased incremental modulus of elasticity (Einc), a phenomenon that is diminished in essential hypertension [13, 16]. Structural alterations related to arterial stiffening in ESRD include fibroelastic intimal thickening, calcification of elastic lamellae, increased extracellular matrix deposition, elastynolysis, inflammation, increased collagen, and decreased elastic fiber content [10, 13].
Although the mechanisms behind these arterial wall alterations are still not well understood, accumulation of traditional cardiovascular risk factors only partially explain the accelerated arterial stiffening in ESRD [3, 12]. Studies exploring the interaction between the etiology of ESRD and the severity of arterial stiffness suggest that ESRD patients with diabetic nephropathy or hypertensive nephrosclerosis as the primary cause of renal failure have higher aortic PWV levels than those with other etiologies of ESRD [20, 21], possibly due to the long-term course of pre-existing CKD and accumulation of cardiovascular risk factors. However, the cross-sectional design of these studies and the absence of careful matching for several confounding factors cannot prove a cause-and-effect association between the etiology of ESRD and severity of arterial damage [20, 21]. Mechanistic pathways closely related to ESRD are suggested to play a particular role in the progression of arteriosclerosis among these patients. Recent advances in these ESRD-specific pathways are discussed further.
Volume overload
The severely impaired capacity of patients with advanced CKD to maintain the homeostasis of sodium and water as well as the inability of hemodialysis patients to reach “dry weight” are common problems that result in chronic volume overload [22]. Inadequate volume control is an important cause of uncontrolled hypertension and LV hypertrophy, whereas prospective observational studies associated volume excess with increased mortality risk among patients receiving hemodialysis [23]. Clinical studies using the bioelectrical impendence analysis (BIA) technique as a tool to determine body composition and fluid status showed that sub-clinical volume expansion, as indicated by an abnormally elevated extracellular-to-intracellular fluid ratio, is independently associated with higher internal diameter of the common carotid artery and higher aortic PWV [24,25,26].
Apart from the role of chronic volume overload, cyclic shifts in volume status that typically occur due to the intermittent nature of renal replacement therapy in patients receiving hemodialysis may acutely influence arterial cushioning function. In previous studies evaluating the intra- and interdialytic variation in wave reflection and arterial stiffness indices, the hemodialysis procedure was shown to acutely reduce the amount of the pulse wave reflected from the periphery without any change in aortic and brachial PWV [27]. The inverse phenomenon, i.e., an increase in wave reflection indices and central aortic pressures, occurred during the interdialytic intervals. Compared with a regular 2-day interdialytic interval, excess fluid accumulation during the long interdialytic interval resulted in a 30% higher elevation of central aortic PP and wave reflection indices [28]. These observations were confirmed in recent studies showing a significant elevation of 5/2.5 mmHg in 24-h aortic BP between the 3rd and 2nd day of the long interdialytic interval with the use ambulatory BP monitoring (ABPM) [29].
Mineral metabolism disturbances and vascular calcification
The severity of vascular calcifications is strongly associated with the progression of arteriosclerosis in ESRD [30] and represents an independent predictor of mortality [31]. Vascular calcification is a long-term process of osteo/chondrocytic transformation of vascular smooth muscle cells (VSMCs) in the media of the arterial wall. Mineral metabolism disturbances are directly involved in all steps of this process as hyperphosphatemia promotes the apoptosis and osteoblastic differentiation of VSMCs as well as inhibits the monocyte/macrophage transformation into osteoclastic-like cells [12]. Fibroblast growth factor (FGF)-23, a phosphaturic hormone that becomes elevated from the early stages of CKD to maintain phosphate homeostasis [32], was suggested to act as mediator of the calcification process in the context of experimental studies showing that FGF-23 is localized in the cytoplasm of VSMCs and enhances their phenotypic differentiation into osteoblastic-like cells [33, 34]. The entire concept of FGF-inducible vascular calcification was revised in view of recent experimental studies showing no expression of FGF-23 in cultured human VSMCs or in normal or calcified mouse aortic rings [35]. Additionally, exogenous FGF-23 is unable to increase phosphate uptake of cultured VSMCs or induce vascular calcification in vitro [35]. In line with these experimental data, a cross-sectional analysis of 1501 patients with stages 3 and 4 CKD participating in the Chronic Renal Insufficiency Cohort (CRIC) study showed no association between plasma FGF-23 levels and coronary artery and thoracic aorta calcium content [35]. Other studies in hemodialysis patients showed no association of FGF-23 with aortic PWV [36, 37].
Apart from factors promoting vascular calcification, this process is also regulated by factors opposing vascular calcification. In this regard, plasma constituents, such as fetuin A, osteoprotegerin, osteopontin and matrix Gla protein, act as endogenous inhibitors of vascular calcification [12]. The particular role of these constituents is to maintain minerals in a soluble form and inhibit their deposition in the media of the arterial wall. Vitamin K deficiency may affect carboxylation of matrix Gla protein and downregulate its inhibitory action of the calcification process. Longitudinal studies showed that correction of vitamin K deficiency and warfarin use may be associated with slower progression of aortic stiffness in hemodialysis patients [38]. Decreased levels of fetuin A and increased osteoprotegerin are associated with higher aortic PWV in hemodialysis patients [39, 40].
Advanced glycation end-products
In advanced CKD, accumulation of AGEs may be either due to reduced renal excretion or due to elevated formation mediated through cumulative carbonyl and oxidative stress [41]. The slow turn-over rate of structural proteins constituting the arterial wall, such as collagen and elastin, makes them particularly vulnerable to AGE cross-linking. Another mechanism through which AGEs may promote the arteriosclerotic process may be AGE-mediated inhibition of endothelial nitric oxide synthase after the linkage of AGEs with their cell membrane receptors, resulting in endothelial dysfunction and adverse vascular remodeling [42]. The link between tissue AGE accumulation and arterial stiffness is further supported by clinical studies associating skin autofluorescence with higher coronary artery calcium content in patients with stages 3–5 CKD [43]. Skin autofluorescence was found to correlate with aortic PWV independent of age and other traditional risk factors in 120 Japanese hemodialysis patients [44]. In a longitudinal study, in which 109 hemodialysis patients were prospectively followed for a mean period of 1.2 years, aortic PWV increased over time with an annual rate of 0.84 m/s [45]. The independent predictor of the progression of aortic stiffness after multivariate adjustment was the baseline levels of pentosidine, a well-characterized AGE.
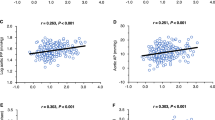
Angiopoietin-2
Angiopoietin-2 is a Tie-2 receptor that not only plays an important role in angiogenesis but also plays important regulatory roles in several pathophysiological processes, including vascular fibrosis and inflammation [46]. In an experimental model of 5/6 nephrectomized mice producing increased levels of angiopoietin-2, this molecule was shown to stimulate endothelial expression of chemokines and adhesion molecules for monocytes as well as to increase the expression of the profibrotic cytokine, TGF-β1, in aortic endothelial cells and to enhance the formation and deposition of collagen in the aortic wall [47]. In a clinical part of this study involving 416 patients with stages 3–5 CKD, plasma levels of angiopoietin-2 were independently associated with higher aortic PWV [47].
Chronic infectious diseases
Chronic infectious diseases may represent another pathway involved in the arteriosclerotic process. A recent study showed that among 215 non-diabetic, predialysis CKD patients, seropositivity for cytomegalovirus (CMV) infection was associated with higher aortic PWV and lower distensibility of the proximal and distal thoracic aorta [48]. This association between CMV seropositivity and arterial stiffness was consistent in all age subgroups and persisted after adjustment for multiple risk factors. The authors proposed that chronic CMV infection may influence large artery structure through modification of the function of VSMCs as well as promotion of inflammation and fibrosis in the media of the arterial wall. Excessive activation of inflammatory and fibrotic pathways was also suggested as the underlying mechanism of accelerated arterial stiffening that is evident in hemodialysis patients with chronic hepatitis C infection [49, 50].
Arterial stiffness assessment
The determination of PWV in the carotid-femoral axis (i.e., aortic PWV) is considered the “gold standard” measure of arterial stiffness in hemodialysis patients [14, 49]. From a pathophysiological standpoint, the aortic and aorto-iliac axis represents the main capacitive segment of the arterial tree. Consequently, the rigidity of the aorta is the principle determinant of the hemodynamic alterations inducible by arterial stiffening. From an epidemiological standpoint, prospective observational studies showed that among hemodialysis patients, aortic PWV was an independent predictor of cardiovascular and all-cause mortality. In contrast, PWV measured in the brachial artery or in the femoro-tibial axis (i.e., in peripheral and muscular-type arterial segments) was of limited prognostic value [51]. Most of the commercially available devices derive their measure of PWV from peripherally recorded pressure waveforms using the validated technique of applanation tonometry. This method is easily applied and exhibits excellent intra- and inter-observer reproducibility [52, 53].
Complementary information on large artery structure and function is obtained via radial or carotid artery applanation tonometry that enables the estimation of the augmentation index (AIx) and central aortic pressures [14, 49]. It has to be noted, however, that AIx is only an indirect marker of arterial stiffness. AIx is an indicator of the reflecting properties of peripheral vascular beds and is determined by the reflection coefficient of microcirculation, velocity of the pulse wave transfer, distance to the reflecting points as well as the duration and pattern of LV ejection [14, 49].
Newly introduced and commercially available devices using the oscillometric technique enable the determination of PWV and wave reflection indices under ambulatory conditions [54]. This method provides comparable estimates of PWV and AIx with those obtained using the widely applied tonometric techniques in hemodialysis patients [55].
Clinical epidemiology
Association of arterial stiffness with interdialytic blood pressure
Studies conducted in non-ESRD populations provided evidence that arterial stiffness determines the blood pressure (BP) response to the antihypertensive drug therapy [56]. The hypothesis that arterial stiffness determines the patterns and rhythms of interdialytic ambulatory BP was explored in a study analyzing 11,833 interdialytic BP measurements obtained from 125 hemodialysis patients with the use of a generalized cosinor model. This analysis showed that each 1-log increase in aortic PWV was associated with a rise of 18.8/7.08 mmHg in the intercept of systolic/diastolic BP and with an increase of 11.7 mmHg in the intercept of PP [57]. Increasing aortic PWV tended also to blunt the circadian amplitude of systolic BP (SBP) and PP [57]. In a post hoc analysis of the Hypertension in Hemodialysis treated with Atenolol or Lisinopril (HDPAL) trial, it was shown that increasing aortic PWV at baseline was an independent determinant of 44-h ambulatory SBP and PP [58]. After adjustment for several confounding factors, each 1 m/s higher baseline PWV was associated with a 1.34 mmHg higher baseline SBP and 1.02 mmHg higher PP. However, aortic PWV at baseline was unable to predict the treatment-induced reduction in 44-h ambulatory BP at 3, 6, and 12 months of follow-up [58]. The latter suggests that among patients on hemodialysis, arterial stiffness does not make hypertension more resistant to the BP-lowering therapy.
Association of arterial stiffness with LV hypertrophy
As mentioned above, aortic SBP augmentation as a result of the premature arrival of the reflected wave from the periphery back to the ascending aorta is the principal mechanism linking arterial stiffness with increased cardiac afterload and LV hypertrophy [4]. This cardiac and arterial interaction is supported by cross-sectional studies showing that aortic PWV is determinant of LV mass index (LVMI) and LV function in hemodialysis patients [59, 60]. Because these cross-sectional data cannot provide cause-and-effect associations, a secondary analysis of the HDPAL trial aimed to explore the relative importance of aortic stiffness and volume as predictors of the treatment-induced improvement in LVMI in hypertensive hemodialysis patients with echocardiographic-documented LV hypertrophy [61]. Aortic PWV was neither determinant of LVMI at baseline nor predictor of its improvement with therapy during the 12-month follow-up of the trial [61]. In contrast, volume emerged as a strong predictor of the treatment-induced reduction in LVMI for the following two reasons: (1) improvement in LV hypertrophy was mediated predominantly through reduction in the cavitary component of the left ventricle instead of improvement in LV wall thickness; (2) adjustment for the change in 44-h interdialytic SBP (a proxy for dry-weight achievement) or inferior vena cava diameter (a proxy for intravascular volume) mitigated the treatment-induced reduction in LVMI [61].
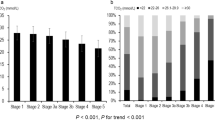
Association of arterial stiffness with clinical outcomes and mortality
In the general population, increased arterial stiffness is a strong and independent risk factor for future cardiovascular events and all-cause mortality. In a meta-analysis of 17 longitudinal studies (incorporating data from 15,877 patients with a mean follow-up of 7.7 years), an increase in aortic PWV by one standard deviation (SD) was associated with increases of 47% and 42% in the risks of cardiovascular and all-cause mortality, respectively [8]. Similar to the general population, prospective observational studies showed that arterial stiffness has a strong prognostic association with clinical outcomes and mortality in ESRD (Table 1). In a historical cohort of 241 hemodialysis patients prospectively followed for 6 years, Blacher et al. showed that the fully adjusted odds ratio (OR) for aortic PWV > 12.0 versus PWV < 9.4 m/s was 5.9 (95% CI: 2.3–15.5) for cardiovascular mortality and 5.4 (95% CI: 2.4–11.9) for all-cause mortality [62]. Notably, the predictive value of aortic PWV is independent of BP and other cardiovascular risk factors. Thus, this observation may be explained by the fact that aortic stiffness represents an intermediate vascular phenotype in hemodialysis, reflecting the cumulative impact of pre-existing hypertension, dialysis vintage, co-morbid conditions and ESRD-specific risk factors [50]. This notion is strongly supported by a recent cohort study of 170 hemodialysis patients prospectively followed for a mean follow-up of 28.1 months [63]. BP load in this analysis was assessed by performing 48-h brachial and aortic ABPM. The hazard ratio (HR) for all-cause and cardiovascular mortality was comparable across quartiles of 48-h brachial and aortic SBP, whereas increasing quartiles of ambulatory PWV were associated with higher mortality hazard in univariate analysis. After multivariate adjustment, the only vascular parameter independently associated with excess mortality hazard was ambulatory PWV (HR: 1.579; 95% CI: 1.187–2.102 for each 1 m/s higher PWV) [63]. Additional cohort studies showed that aortic PWV is a BP-independent predictor of cardiovascular morbidity and mortality in patients receiving peritoneal dialysis and in renal transplant recipients [64, 65], proving the strong prognostic implications of arterial stiffness in the entire spectrum of ESRD.
Recent studies advanced our knowledge showing that the preferential stiffening of the aortic wall and the disappearance of the normal stiffness gradient between central and peripheral arterial segments is another factor closely associated with excess mortality. In a cohort study of 310 hemodialysis patients prospectively followed for a mean period of 29 months, each 1-SD increase in the ratio of the carotid-femoral PWV divided by carotid-radial PWV (a marker of the stiffness mismatch) was associated with 43% higher risk of all-cause mortality (HR: 1.43; 95% CI: 1.24–1.64) [66]. After adjustment for several risk factors, the PWV ratio remained an independent predictor of mortality (HR: 1.23; 95% CI: 1.02–1.49), whereas carotid-femoral PWV and carotid-radial PWV alone had no prognostic association with mortality. Other studies showed that the longitudinal change in aortic PWV is of superior prognostic significance relative to the PWV assessed in a single time-point [67]. Importantly, the absence of reduction in aortic PWV in response to BP lowering was associated with 2.5-fold higher risk of all-cause and cardiovascular mortality in a French cohort of 153 hemodialysis patients [68]. This observation supports the notion that aortic stiffness is not simply a predictor of risk but a true and potentially reversible cardiovascular risk factor in ESRD.
Therapies to regress arterial stiffness
Given the strong prognostic association of arterial stiffness with mortality, regression of arteriosclerotic process is anticipated to confer benefits toward cardiovascular risk reduction in patients with ESRD. The principal therapeutic approach to regress arterial stiffness is to adequately control BP [3, 7]. In addition to BP lowering, the reversion of the ESRD-specific pathways involved in pathogenesis and progression of arteriosclerosis may represent novel treatment paradigms towards arterial stiffness attenuation.
BP lowering and antihypertensive medications
Experimental studies suggested that agents blocking the renin–angiotensin–aldosterone system (RAAS) may exert pleiotropic effects on vasculature, including inhibition of the proliferative actions of angiotensin II, downregulation of fibrosis and collagen deposition and rearrangement of arterial wall biomaterials [69, 70]. On this basis, earlier observational [68] and interventional studies suggested that among patients with ESRD, RAAS blockers may be superior to other antihypertensive drug classes in delaying the progression of arteriosclerosis (Table 2) [71,72,73]. This notion, however, was not confirmed in a recent secondary analysis of the HDPAL trial. In the unadjusted models, 6-month-long therapy with an atenolol-based antihypertensive regimen was associated with a 14.8% higher reduction of aortic PWV in comparison with a therapy based on the angiotensin-converting-enzyme (ACE)-inhibitor, lisinopril [74]. The difference between drugs persisted after adjustment for several cardiovascular risk factors but disappeared after additional adjustment for the treatment-induced reduction in 44 h ambulatory SBP (difference between drugs: 11.8; 95% CI: 22.3, 25.9%; P = 0.10) [74]. Similarly, in the Saving Residual Renal Function Among Hemodialysis Patients Receiving Irbesartan (SAFIR) study, 12-month-long treatment with the angiotensin-receptor-blocker (ARB), irbesartan, was not superior to placebo in reducing aortic PWV (ΔPlacebo vs ΔARB: 0.4 m/s; 95% CI: −0.7, 1.5, P = 0.49) [75]. Once again, irbesartan-induced reduction in aortic PWV was strongly associated with the change in pre-dialysis SBP [75]. Accordingly, it remains unclear whether the beneficial effect of RAAS-blockade on arterial stiffness is BP-mediated or BP-independent [76].
Volume control
Achievement of adequate volume control is the principal therapeutic approach of hypertension management in patients on hemodialysis [22]. In the Dry-weight Reduction in Hemodialysis Patients (DRIP) trial, probing of dry weight over a 2-month-long follow-up culminated in a significant reduction of 6.6/3.1 mmHg in 44-h ambulatory BP [77]. This BP-lowering effect of dry-weight reduction was associated with a parallel regression of LVMI in a sub-analysis of the DRIP trial [78]. The volume-mediated regression of target organ damage is further supported by two subsequent randomized trials showing that the use of BIA as a tool to guide the management of hydration status in hemodialysis better regresses the arteriosclerotic process. Hur et al. [79] randomized 156 hemodialysis patients to BIA-guided or conventional management of dry weight. Over a 12-month-long follow-up, 44-h ambulatory BP and arterial stiffness parameters were decreased in those patients assigned to the BIA-guided management of hydration status but remained unchanged in the control group [79]. In a subsequent study, 131 hemodialysis patients were randomly assigned to BIA-guided or clinical-guided management of volume for a mean follow-up of 2.5 years. Strict volume control achieved through BIA-guided management of dry weight culminated in a significantly higher reduction of aortic PWV during follow-up (difference between groups: −2.78 m/s; 95% CI: −3.75 to −1.80 m/s, P < 0.001) [80]. This volume-mediated regression of aortic stiffness was accompanied by a parallel improvement in all-cause mortality. These promising results need to be confirmed in larger randomized trials.
Phosphate binders
Randomized studies showed that sevelamer was superior to calcium carbonate in causing regression of coronary artery and thoracic aorta calcifications [81, 82]. Other studies showed a long-term increase in brachial–ankle PWV in hemodialysis patients randomly assigned to 2-year-long therapy with calcium carbonate, whereas PWV remained unchanged in patients assigned to lanthanum carbonate [83, 84]. Accordingly, the avoidance of calcium-containing phosphate binders may be another therapeutic avenue for treating arterial stiffness in ESRD.
Statins
The antiinflammatory, antifibrotic and antiproliferative actions of statins on vasculature may also be translated into a beneficial effect on arterial stiffness [85]. In CKD patients not yet on dialysis, low-dose atorvastatin treatment for 36 months significantly lowered the rate of change in aortic PWV relative to placebo [86]. Improvement in arterial stiffness after 6-month fluvastatin therapy was also observed in another small study enrolling 22 diabetic hemodialysis patients with normal serum lipid profiles [87].
Dialysis treatment optimization
Enhanced clearance of middle-to-high molecular weight solutes by combining convective and diffusive transport through hemodiafiltration and the associated benefits on microvascular endothelial function have generated the hypothesis that convective dialytic modalities may be advantageous in improving large artery stiffness. This notion is supported by some clinical studies showing that switching ESRD patients from low-flux hemodialysis to high-efficiency on-line hemodiafiltration was associated with slower long-term progression of the arteriosclerotic process [88, 89]. This benefit, however, was not confirmed in a recent sub-analysis of the CONvective TRAnsport STudy (CONTRAST) trial [90].
Renal transplantation
Observational studies showed reduction in aortic PWV after living donor transplantation and short-term improvement in wave reflection indices after cadaveric engraftment [91, 92]. However, it remains unclear whether these benefits persist in the long-term post-transplant period. Aortic stiffness in cadaveric kidney transplant recipients is influenced by the donor characteristics (i.e., lower post-transplant PWV in recipients of young donors and higher PWV with more rapid deterioration in those receiving kidneys from older donors) [93]. Arterial stiffness after successful renal transplantation may also be influenced by several other parameters, including incomplete restoration of renal function, chronic allograft nephropathy, new-onset diabetes after renal transplantation, and use of cyclosporine and other immune-suppressant agents [94].
Conclusion
Accelerated arterial stiffening is the typical feature of vascular remodeling and represents a strong and independent predictor of cardiovascular morbidity and mortality in ESRD [95, 96]. The accumulation of traditional risk factors only partially explains the severity of arterial damage, and it seems likely that ESRD-specific pathways, such as acute and chronic volume overload, elevated calcium-phosphate products, vascular calcifications, and accumulation of AGEs, play a prominent role in pathogenesis of the arteriosclerotic process. As these and other mechanistic pathways leading to arterial stiffening in ESRD are clarified, novel interventions targeting arterial stiffness attenuation may advance our therapeutic regimens. In the meantime, achievement of adequate BP control via strict volume management and appropriate use of antihypertensive medications appear to be the most effective tools to delay the progression of arteriosclerosis and modify the cardiovascular risk profile of ESRD patients.
References
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, McAlister F, Garg AX. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17:2034–47.
Taal MW. Arterial stiffness in chronic kidney disease: an update. Curr Opin Nephrol Hypertens. 2014;23:169–73.
London G, Covic A, Goldsmith D, Wiecek A, Suleymanlar G, Ortiz A, Massy Z, Lindholm B, Martinez-Castelao A, Fliser D, Agarwal R, Jager KJ, Dekker FW, Blankestijn PJ1, Zoccali C, for EUropean REnal and CArdiovascular Medicine working group of the European Renal Association–European Dialysis and Transplant Association (ERA–EDTA). Arterial aging and arterial disease: interplay between central hemodynamics, cardiac work, and organ flow-implications for CKD and cardiovascular disease. Kidney Int Suppl. 2011;1:10–2.
O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005;46:200–4.
Chirinos JA, Townsend RR. Reducing arterial stiffness in CKD: revising the paradigms. Clin J Am Soc Nephrol. 2015;10:547–50.
Georgianos PI, Sarafidis PA, Lasaridis AN. Arterial stiffness: a novel cardiovascular risk factor in kidney disease patients. Curr Vasc Pharmacol. 2015;13:229–38.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27.
van Varik BJ, Vossen LM, Rennenberg RJ, Stoffers HE, Kessels AG, de Leeuw PW, Kroon AA. Arterial stiffness and decline of renal function in a primary care population. Hypertens Res. 2017;40:73–8.
Georgianos PI, Sarafidis PA, Liakopoulos V. Arterial stiffness: a novel risk factor for kidney injury progression? Am J Hypertens. 2015;28:958–65.
Laszlo A, Reusz G, Nemcsik J. Ambulatory arterial stiffness in chronic kidney disease: a methodological review. Hypertens Res. 2016;39:192–8.
Briet M, Burns KD. Chronic kidney disease and vascular remodelling: molecular mechanisms and clinical implications. Clin Sci. 2012;123:399–416.
Briet M, Boutouyrie P, Laurent S, London GM. Arterial stiffness and pulse pressure in CKD and ESRD. Kidney Int. 2012;82:388–400.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H. European network for non-invasive investigation of large arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
O’Rourke MF. Wave travel and reflection in the arterial system. J Hypertens Suppl. 1999;17:S45–S47.
Guerin AP, Pannier B, Metivier F, Marchais SJ, London GM. Assessment and significance of arterial stiffness in patients with chronic kidney disease. Curr Opin Nephrol Hypertens. 2008;17:635–41.
Laurent S, Girerd X, Mourad JJ, Lacolley P, Beck L, Boutouyrie P, Mignot JP, Safar M. Elastic modulus of the radial artery wall material is not increased in patients with essential hypertension. Arterioscler Thromb. 1994;14:1223–31.
Mourad JJ, Girerd X, Boutouyrie P, Laurent S, Safar M, London G. Increased stiffness of radial artery wall material in end-stage renal disease. Hypertension. 1997;30:1425–30.
Verbeke FH, Agharazii M, Boutouyrie P, Pannier B, Guerin AP, London GM. Local shear stress and brachial artery functions in end-stage renal disease. J Am Soc Nephrol. 2007;18:621–8.
El GB, Daaboul Y, Korjian S, El Alam A, Mansour A, Hariri E, Samad S, Salameh P, Dahdah G, Blacher J, Safar ME, Aoun Bahous S. Etiology of end-stage renal disease and arterial stiffness among hemodialysis patients. Biomed Res Int. 2017;2017:2543262.
Kesoi I, Sagi B, Toth OI, Vas T, Fazekas A, Kovács T, Pintér T, Wittmann I, Nagy J. Different effect of IgA nephropathy and polycystic kidney disease on arterial stiffness. Kidney Blood Press Res. 2011;34:158–66.
Georgianos PI, Agarwal R. Epidemiology, diagnosis and management of hypertension among patients on chronic dialysis. Nat Rev Nephrol. 2016;12:636–47.
Agarwal R. Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension. 2010;56:512–7.
Chen CH, Lin YP, Yu WC, Yang WC, Ding YA. Volume status and blood pressure during long-term hemodialysis: role of ventricular stiffness. Hypertension. 2003;42:257–62.
Lin YP, Yu WC, Hsu TL, Ding PY, Yang WC, Chen CH. The extracellular fluid-to-intracellular fluid volume ratio is associated with large-artery structure and function in hemodialysis patients. Am J Kidney Dis. 2003;42:990–9.
Zheng D, Cheng LT, Zhuang Z, Gu Y, Tang LJ, Wang T. Correlation between pulse wave velocity and fluid distribution in hemodialysis patients. Blood Purif. 2009;27:248–52.
Georgianos PI, Sarafidis PA, Malindretos P, Nikolaidis P, Lasaridis AN. Hemodialysis reduces augmentation index but not aortic or brachial pulse wave velocity in dialysis-requiring patients. Am J Nephrol. 2011;34:407–14.
Georgianos PI, Sarafidis PA, Haidich AB, Karpetas A, Stamatiadis D, Nikolaidis P, Lasaridis AN. Diverse effects of interdialytic intervals on central wave augmentation in haemodialysis patients. Nephrol Dial Transplant. 2013;28:2160–9.
Koutroumbas G, Georgianos PI, Sarafidis PA, Protogerou A, Karpetas A, Vakianis P, Raptis V, Liakopoulos V, Panagoutsos S, Syrganis C, Passadakis P. Ambulatory aortic blood pressure, wave reflections and pulse wave velocity are elevated during the third in comparison to the second interdialytic day of the long interval in chronic haemodialysis patients. Nephrol Dial Transplant. 2015;30:2046–53.
Haydar AA, Covic A, Colhoun H, Rubens M, Goldsmith DJ. Coronary artery calcification and aortic pulse wave velocity in chronic kidney disease patients. Kidney Int. 2004;65:1790–4.
London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–40.
Larsson T, Nisbeth U, Ljunggren O, Juppner H, Jonsson KB. Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int. 2003;64:2272–9.
Silswal N, Touchberry CD, Daniel DR, McCarthy DL, Zhang S, Andresen J, Stubbs JR, Wacker MJ. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am J Physiol Endocrinol Metab. 2014;307:E426–E436.
Voigt M, Fischer DC, Rimpau M, Schareck W, Haffner D. Fibroblast growth factor (FGF)-23 and fetuin-A in calcified carotid atheroma. Histopathology. 2010;56:775–88.
Scialla JJ, Lau WL, Reilly MP, Isakova T, Yang HY, Crouthamel MH, Chavkin NW, Rahman M, Wahl P, Amaral AP, Hamano T, Master SR, Nessel L, Chai B, Xie D, Kallem RR, Chen J, Lash JP, Kusek JW, Budoff MJ, Giachelli CM, Wolf M, Chronic Renal Insufficiency Cohort Study Investigators Fibroblast growth factor 23 is not associated with and does not induce arterial calcification. Kidney Int. 2013;83:1159–68.
Desjardins L, Liabeuf S, Massy ZA. Lack of predictive value of FGF23 levels on pulse wave velocity. Osteoporos Int. 2013;24:1137.
Houston J, Smith K, Isakova T, Sowden N, Wolf M, Gutierrez OM. Associations of dietary phosphorus intake, urinary phosphate excretion, and fibroblast growth factor 23 with vascular stiffness in chronic kidney disease. J Ren Nutr. 2013;23:12–20.
Mac-Way F, Poulin A, Utescu MS, De Serres SA, Marquis K, Douville P, Desmeules S, Larivière R, Lebel M, Agharazii M. The impact of warfarin on the rate of progression of aortic stiffness in hemodialysis patients: a longitudinal study. Nephrol Dial Transplant. 2014;29:2113–20.
Hermans MM, Brandenburg V, Ketteler M, Kooman JP, van der Sande FM, Gladziwa U, Rensma PL, Bartelet K, Konings CJ, Hoeks AP, Floege J, Leunissen KM. Study on the relationship of serum fetuin-A concentration with aortic stiffness in patients on dialysis. Nephrol Dial Transplant. 2006;21:1293–9.
Pateinakis P, Papagianni A, Douma S, Efstratiadis G, Memmos D. Associations of fetuin-A and osteoprotegerin with arterial stiffness and early atherosclerosis in chronic hemodialysis patients. BMC Nephrol. 2013;14:122.
McIntyre NJ, Fluck RJ, McIntyre CW, Taal MW. Skin autofluorescence and the association with renal and cardiovascular risk factors in chronic kidney disease stage 3. Clin J Am Soc Nephrol. 2011;6:2356–63.
Linden E, Cai W, He JC, Xue C, Li Z, Winston J, Vlassara H, Uribarri J. Endothelial dysfunction in patients with chronic kidney disease results from advanced glycation end products (AGE)-mediated inhibition of endothelial nitric oxide synthase through RAGE activation. Clin J Am Soc Nephrol. 2008;3:691–8.
Wang AY, Wong CK, Yau YY, Wong S, Chan IH, Lam CW. Skin autofluorescence associates with vascular calcification in chronic kidney disease. Arterioscler Thromb Vasc Biol. 2014;34:1784–90.
Ueno H, Koyama H, Tanaka S, Fukumoto S, Shinohara K, Shoji T, Emoto M, Tahara H, Kakiya R, Tabata T, Miyata T, Nishizawa Y. Skin autofluorescence, a marker for advanced glycation end product accumulation, is associated with arterial stiffness in patients with end-stage renal disease. Metabolism. 2008;57:1452–7.
Utescu MS, Couture V, Mac-Way F, De Serres SA, Marquis K, Larivière R, Desmeules S, Lebel M, Boutouyrie P, Agharazii M. Determinants of progression of aortic stiffness in hemodialysis patients: a prospective longitudinal study. Hypertension. 2013;62:154–60.
Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, Gale NW, Witzenrath M, Rosseau S, Suttorp N, Sobke A, Herrmann M, Preissner KT, Vajkoczy P, Augustin HG. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med. 2006;12:235–9.
Chang FC, Chiang WC, Tsai MH, Chou YH, Pan SY, Chang YT, Yeh PY, Chen YT, Chiang CK, Chen YM, Chu TS, Wu KD, Lin SL. Angiopoietin-2-induced arterial stiffness in CKD. J Am Soc Nephrol. 2014;25:1198–209.
Wall NA, Chue CD, Edwards NC, Pankhurst T, Harper L, Steeds RP, Lauder S, Townend JN, Moss P, Ferro CJ. Cytomegalovirus seropositivity is associated with increased arterial stiffness in patients with chronic kidney disease. PLoS ONE. 2013;8:e55686.
DeLoach SS, Townsend RR. Vascular stiffness: its measurement and significance for epidemiologic and outcome studies. Clin J Am Soc Nephrol. 2008;3:184–92.
Oyake N, Shimada T, Murakami Y, Ishibashi Y, Satoh H, Suzuki K, Matsumory A, Oda T. Hepatitis C virus infection as a risk factor for increased aortic stiffness and cardiovascular events in dialysis patients. J Nephrol. 2008;21:345–53.
Shoji T, Emoto M, Shinohara K, Kakiya R, Tsujimoto Y, Kishimoto H, Ishimura E, Tabata T, Nishizawa Y. Diabetes mellitus, aortic stiffness, and cardiovascular mortality in end-stage renal disease. J Am Soc Nephrol. 2001;12:2117–24.
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL, Kass DA. Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Valid Gen Transf Funct Circ. 1997;95:1827–36.
Wilkinson IB, Fuchs SA, Jansen IM, Spratt JC, Murray GD, Cockcroft JR, Webb DJ. Reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens. 1998;16:2079–84.
Weber T, Wassertheurer S, Rammer M, Maurer E, Hametner B, Mayer CC, Kropf J, Eber B. Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension. 2011;58:825–32.
Sarafidis PA, Georgianos PI, Karpetas A, Bikos A, Korelidou L, Tersi M, Divanis D, Tzanis G, Mavromatidis K, Liakopoulos V, Zebekakis PE, Lasaridis A, Protogerou AD. Evaluation of a novel brachial cuff-based oscillometric method for estimating central systolic pressure in hemodialysis patients. Am J Nephrol. 2014;40:242–50.
Protogerou A, Blacher J, Stergiou GS, Achimastos A, Safar ME. Blood pressure response under chronic antihypertensive drug therapy: the role of aortic stiffness in the REASON (Preterax in Regression of Arterial Stiffness in a Controlled Double-Blind) study. J Am Coll Cardiol. 2009;53:445–51.
Agarwal R, Light RP. Arterial stiffness and interdialytic weight gain influence ambulatory blood pressure patterns in hemodialysis patients. Am J Physiol Ren Physiol. 2008;294:F303–8.
Georgianos PI, Agarwal R. Aortic Stiffness, Ambulatory Blood Pressure, and Predictors of Response to Antihypertensive Therapy in Hemodialysis. Am J Kidney Dis. 2015;66:305–12.
London GM, Guerin AP, Marchais SJ, Pannier B, Safar ME, Day M, Metivier F. Cardiac and arterial interactions in end-stage renal disease. Kidney Int. 1996;50:600–8.
Nitta K, Akiba T, Uchida K, Otsubo S, Otsubo Y, Takei T, Ogawa T, Yumura W, Kabaya T, Nihei H. Left ventricular hypertrophy is associated with arterial stiffness and vascular calcification in hemodialysis patients. Hypertens Res. 2004;27:47–52.
Georgianos PI, Agarwal R. Relative importance of aortic stiffness and volume as predictors of treatment-induced improvement in left ventricular mass index in dialysis. PLoS ONE. 2015;10:e0135457.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999;99:2434–9.
Sarafidis PA, Loutradis C, Karpetas A, Tzanis G, Piperidou A, Koutroumpas G, Raptis V, Syrgkanis C, Liakopoulos V, Efstratiadis G, London G, Zoccali C. Ambulatory pulse wave velocity is a stronger predictor of cardiovascular events and all-cause mortality than office and ambulatory blood pressure in hemodialysis patients. Hypertension. 2017;70:148–57.
Szeto CC, Kwan BC, Chow KM, Leung CB, Law MC, Li PK. Prognostic value of arterial pulse wave velocity in peritoneal dialysis patients. Am J Nephrol. 2012;35:127–33.
Verbeke F, Marechal C, Van Laecke S, Van Biesen W, Devuyst O, Van Bortel LM, Jadoul M, Vanholder R. Aortic stiffness and central wave reflections predict outcome in renal transplant recipients. Hypertension. 2011;58:833–8.
Fortier C, Mac-Way F, Desmeules S, Marquis K, De Serres SA, Lebel M, Boutouyrie P, Agharazii M. Aortic-brachial stiffness mismatch and mortality in dialysis population. Hypertension. 2015;65:378–84.
Korjian S, Daaboul Y, El-Ghoul B, Samad S, Salameh P, Dahdah G, Hariri E, Mansour A, Spielman K, Blacher J, Safar ME, Bahous SA. Change in pulse wave velocity and short-term development of cardiovascular events in the hemodialysis population. J Clin Hypertens. 2016;18:857–63.
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation. 2001;103:987–92.
Ng K, Hildreth CM, Avolio AP, Phillips JK. Angiotensin-converting enzyme inhibitor limits pulse-wave velocity and aortic calcification in a rat model of cystic renal disease. Am J Physiol Ren Physiol. 2011;301:F959–66.
Touyz RM. Molecular and cellular mechanisms in vascular injury in hypertension: role of angiotensin II. Curr Opin Nephrol Hypertens. 2005;14:125–31.
Ichihara A, Hayashi M, Kaneshiro Y, Takemitsu T, Homma K, Kanno Y, Yoshizawa M, Furukawa T, Takenaka T, Saruta T. Low doses of losartan and trandolapril improve arterial stiffness in hemodialysis patients. Am J Kidney Dis. 2005;45:866–74.
London GM, Pannier B, Guerin AP, Marchais SJ, Safar ME, Cuche JL. Cardiac hypertrophy, aortic compliance, peripheral resistance, and wave reflection in end-stage renal disease. Comparative effects of ACE inhibition and calcium channel blockade. Circulation. 1994;90:2786–96.
Mitsuhashi H, Tamura K, Yamauchi J, Ozawa M, Yanagi M, Dejima T, Wakui H, Masuda S, Azuma K, Kanaoka T, Ohsawa M, Maeda A, Tsurumi-Ikeya Y, Okano Y, Ishigami T, Toya Y, Tokita Y, Ohnishi T, Umemura S. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis. 2009;207:186–90.
Georgianos PI, Agarwal R. Effect of lisinopril and atenolol on aortic stiffness in patients on hemodialysis. Clin J Am Soc Nephrol. 2015;10:639–45.
Peters CD, Kjaergaard KD, Jensen JD, Christensen KL, Strandhave C, Tietze IN, Novosel MK, Bibby BM, Jensen LT, Sloth E, Jespersen B. No significant effect of angiotensin II receptor blockade on intermediate cardiovascular end points in hemodialysis patients. Kidney Int. 2014;86:625–37.
Zoccali C, Mallamaci F. Pleiotropic effects of angiotensin II blockers in hemodialysis patients: myth or reality? Kidney Int. 2014;86:469–71.
Agarwal R, Alborzi P, Satyan S, Light RP. Dry-weight reduction in hypertensive hemodialysis patients (DRIP): a randomized, controlled trial. Hypertension. 2009;53:500–7.
Agarwal R, Bouldin JM, Light RP, Garg A. Probing dry-weight improves left ventricular mass index. Am J Nephrol. 2011;33:373–80.
Hur E, Usta M, Toz H, Wabel P, Kahvecioglu S, Kayikcioglu M, Demirci MS, Ozkahya M, Duman S, Ok E. Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis. 2013;61:957–65.
Onofriescu M, Hogas S, Voroneanu L, Apetrii M, Nistor I, Kanbay M, Covic AC. Bioimpedance-guided fluid management in maintenance hemodialysis: a pilot randomized controlled trial. Am J Kidney Dis. 2014;64:111–8.
Block GA, Spiegel DM, Ehrlich J, Mehta R, Lindbergh J, Dreisbach A, Raggi P. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815–24.
Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52.
Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: a pilot randomized controlled trial. Nephrology. 2011;16:290–8.
Wada K, Wada Y, Uchida HA, Tsuruoka S. Effects of lanthanum carbonate versus calcium carbonate on vascular stiffness and bone mineral metabolism in hemodialysis patients with type 2 diabetes mellitus: a randomized controlled trial. Int J Nephrol Renov Dis. 2015;8:111–8.
Rizos EC, Agouridis AP, Elisaf MS. The effect of statin therapy on arterial stiffness by measuring pulse wave velocity: a systematic review. Curr Vasc Pharmacol. 2010;8:638–44.
Fassett RG, Robertson IK, Ball MJ, Geraghty DP, Sharman JE, Coombes JS. Effects of atorvastatin on arterial stiffness in chronic kidney disease: a randomised controlled trial. J Atheroscler Thromb. 2010;17:235–41.
Ichihara A, Hayashi M, Ryuzaki M, Handa M, Furukawa T, Saruta T. Fluvastatin prevents development of arterial stiffness in haemodialysis patients with type 2 diabetes mellitus. Nephrol Dial Transplant. 2002;17:1513–7.
Bellien J, Freguin-Bouilland C, Joannides R, Hanoy M, Rémy-Jouet I, Monteil C, Iacob M, Martin L, Renet S, Vendeville C, Godin M, Thuillez C, Le Roy F. High-efficiency on-line haemodiafiltration improves conduit artery endothelial function compared with high-flux haemodialysis in end-stage renal disease patients. Nephrol Dial Transplant. 2014;29:414–22.
Li PK, Cheng YL, Leung CB, Szeto CC, Chow KM, Kwan BC, Ng ES, Fok QW, Poon YL, Yu AW. Effect of membrane permeability on inflammation and arterial stiffness: a randomized trial. Clin J Am Soc Nephrol. 2010;5:652–8.
Mostovaya IM, Bots ML, van den Dorpel MA, Grooteman MP, Kamp O, Levesque R, Ter Wee PM, Nubé MJ, Blankestijn PJ. A randomized trial of hemodiafiltration and change in cardiovascular parameters. Clin J Am Soc Nephrol. 2014;9:520–6.
Kaur M, Lal C, Bhowmik D, Jaryal AK, Deepak KK, Agarwal SK. Reduction in augmentation index after successful renal transplantation. Clin Exp Nephrol. 2012;17:134–9.
Kovacs D, Szabo L, Fedor R, Laczik R, Soltész P, Locsey L, Asztalos L. Prospective study of changes in arterial stiffness among kidney-transplanted patients. Transplant Proc. 2011;43:1252–3.
Delahousse M, Chaignon M, Mesnard L, Boutouyrie P, Safar ME, Lebret T, Pastural-Thaunat M, Tricot L, Kolko-Labadens A, Karras A, Haymann JP. Aortic stiffness of kidney transplant recipients correlates with donor age. J Am Soc Nephrol. 2008;19:798–805.
Verbeke F, Van Biesen W, Peeters P, Van Bortel LM, Vanholder RC. Arterial stiffness and wave reflections in renal transplant recipients. Nephrol Dial Transplant. 2007;22:3021–7.
Verbeke F, Van Biesen W, Honkanen E, Wikström B, Jensen PB, Krzesinski JM, Rasmussen M, Vanholder R, Rensma PL, CORD Study Investigators Prognostic value of aortic stiffness and calcification for cardiovascular events and mortality in dialysis patients: outcome of the calcification outcome in renal disease (CORD) study. Clin J Am Soc Nephrol. 2011;6:153–9.
London GM, Safar ME, Pannier B. Aortic aging in ESRD: structural, hemodynamic, and mortality implications. J Am Soc Nephrol. 2016;27:1837–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Georgianos, P.I., Pikilidou, M.I., Liakopoulos, V. et al. Arterial stiffness in end-stage renal disease—pathogenesis, clinical epidemiology, and therapeutic potentials. Hypertens Res 41, 309–319 (2018). https://doi.org/10.1038/s41440-018-0025-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0025-5
This article is cited by
-
A comparative analysis of ambulatory BP profile and arterial stiffness between CAPD and APD
Journal of Human Hypertension (2022)
-
Fiber connectivity density mapping in end-stage renal disease patients: a preliminary study
Brain Imaging and Behavior (2022)
-
Serum biomarkers, skin autofluorescence and other methods. Which parameter better illustrates the relationship between advanced glycation end products and arterial stiffness in the general population?
Hypertension Research (2021)
-
Snapshot photoacoustic topography through an ergodic relay for high-throughput imaging of optical absorption
Nature Photonics (2020)
-
Postdialysis blood pressure is a better predictor of mortality than predialysis blood pressure in Japanese hemodialysis patients: the Japan Dialysis Outcomes and Practice Patterns Study
Hypertension Research (2020)