Abstract
Abnormalities in circadian blood pressure (BP) variation have been suggested to be associated with cardiovascular diseases and mortality. Factors affecting this variability need to be clarified to precisely evaluate the risk of circadian BP abnormalities. Given the seasonal differences in casual BP, it was hypothesized that nocturnal BP may also differ by season. Here, we aimed to clarify the seasonality of circadian BP variation, as well as the factors associated with this seasonality, in a large-scale general population (n = 4780). This is a cross-sectional study based on multiday BP values measured in the evening, during sleep, and in the morning. Measurements were taken at home using an automatic cuff-oscillometric device. The sleeping period was objectively defined by actigraphy. The nocturnal systolic BP fall was significantly less in individuals whose BP was measured during the summer season (summer, −5.8 ± 7.8%; middle (spring or autumn), −8.2 ± 7.5%; winter, −11.0 ± 7.7%; p < 0.001), resulting in higher frequencies of riser (summer, 19.9; middle, 12.8; winter, 7.8%) and non-dipper (summer, 51.4; middle, 46.3; winter, 37.0%) patterns in the summer season (p < 0.001). The results of linear regression analysis identified the middle (β = 0.154, p < 0.001) and summer season (β = 0.261, p < 0.001) as strong positive determinants for decreasing the nocturnal SBP fall. No seasonality was observed in day-to-day variability of the dipping pattern (Kendall’s coefficient: winter, 0.527; middle, 0.539; summer, 0.515). The nocturnal BP fall was largely different by season, with a higher frequency of riser and non-dipper patterns in the summer. The seasonality might not be due to the seasonal difference in day-to-day variability of nocturnal BP changes.
Similar content being viewed by others
Introduction
Abnormalities in circadian blood pressure (BP) variation, particularly the disappearance of the nocturnal BP fall (non-dipping) or rising of nocturnal BP vs. daytime BP, have been consistently reported to be associated with the incidence of cardiovascular diseases and subclinical organ damage independently of daytime average BP levels [1] in various populations [2,3,4,5,6]. It has been reported that a decrease in nocturnal BP fall was associated with total mortality [7, 8]. A known determinant for a rise in BP during sleep is obstructive sleep apnea and probably lower sleep quality; the mechanism for increasing sleep BP might be the activation of sympathetic neural tone by episodic hypoxia [9]. We also reported that increasing the oxygen desaturation index during sleep, as well as carotid arterial hypertrophy, was an independent determinant for the non-dipping pattern in a general population [10]. In addition to these known risk factors, we further clarified that the plasma level of B-type natriuretic peptide (BNP) was another independent determinant for nocturnal BP rising [10], which might represent excessive body fluid retention that increases sleep BP to facilitate sodium excretion and diuresis. However, given a low frequency of individuals showing high BNP levels in a general population, additional factors need to be clarified to further understand the mechanisms underlying circadian BP variations.
BP is regulated by both physiological and environmental factors, and the strongest environmental factor for BP is ambient temperature. It has been repeatedly reported that there is an apparent seasonal variation in BP levels, with lower BP levels in the hotter season [11]. Further, a recent longitudinal study in the Japanese population involving long-term repeated measurements of home BP reported clear periodic intra-individual seasonal BP variations [12]. Given these previous reports, it can be easily hypothesized that not only daytime BP but also sleep BP levels might be affected by temperature. However, the results of epidemiological studies regarding seasonal variations in nocturnal BP are limited in hypertensive patients [13,14,15,16,17]. The largest study based on approximately 8500 patients at a hypertension clinic reported a positive association between outdoor air temperature and nighttime BP, particularly in treated patients [13]. Fedecostante et al. reported higher night-time SBP levels and a more frequent non-dipper pattern in the summer season in approximately 1400 hypertensive individuals [14]. A similar association was observed in a small-scale study [15, 16], although conflicting results were reported [17].
Against this background, we aimed to clarify seasonal variations in nocturnal BP fall, as well as factors associated with this seasonality, in a general population living in Japan; a large seasonal temperature variation occurs in this location, which will further clarify the seasonal effect on circadian BP variation. Furthermore, previous studies involving seasonal variation [13, 14] were based on nocturnal BP measured on a given day, and the reproducibility of nocturnal BP measurement was not considered. We therefore further investigated the association between day-to-day nocturnal BP variability and seasonality by analyzing multiday BP values measured during the night. Seasonality in nocturnal BP fall might be an important factor in epidemiological studies, particularly in studies aiming to evaluate the prognostic and diagnostic significance of circadian BP abnormalities.
Methods
Study participants
This is a cross-sectional study using a dataset describing participants in the Nagahama Prospective Cohort for Comprehensive Human Bioscience (the Nagahama Study). Participants in this community-based prospective cohort study were recruited between 2008 and 2010 from the general population of Nagahama City, a rural city of 125,000 inhabitants located in central Japan. Community residents aged 30–74 years, living independently, and without physical impairment or dysfunction were eligible. Of the 9804 included participants, 14 withdrew consent to participate, and 26 were excluded based on genetic analysis demonstrating a differing ethnic background. Thus, the total number of cohort participants was 9764.
Participants in the Nagahama cohort were invited to a follow-up assessment conducted 5 years after baseline evaluations (2013–2015), and 8289 of the original 9764 cohort members participated. After excluding 137 individuals who died and 279 who had moved away from Nagahama City, the follow-up rate was 88.7%. Among the 8289 participants in the follow-up investigation, individuals who met the following criteria were excluded from the analysis: pregnant women (n = 24), pacemaker implantation (n = 12), hemodialysis therapy (n = 5), obstructive sleep apnea therapy by continuous positive airway pressure (n = 36) or oral appliance (n = 9), severe renal functional decline (estimated glomerular filtration rate [eGFR] <45 ml/min/1.73 m2 or urinary albumin ≥300 mg/day, n = 453), incomplete or wide deviation of clinical values required for the present study (n = 16), and no measurement of home BP (n = 1711). Participants who were considered shift workers (n = 15) according to home BP monitoring time were also excluded.
All study procedures were approved by the ethics committee of Kyoto University Graduate School of Medicine and by the Nagahama Municipal Review Board. Written informed consent was obtained from all participants.
Home and sleep BP monitoring
BP monitoring at home was provided as an optional examination upon request. An automatic cuff-oscillometric device (HEM-7080IC, Omron Healthcare, Kyoto, Japan) was provided to participants who intended to undergo home BP monitoring. Participants were required to measure home BP (morning and evening BP) for 7 days and sleep BP for the last 5 nights (day 3 to day 7) according to the following procedures: [home BP]: measure BP by themselves in a sitting position within 1 h after awakening (morning BP) or just before going to bed (evening BP), before taking antihypertensive drugs (morning BP measurement), after urination, and after a few minutes of rest in a sitting position; [sleep BP]: sleep while wearing a cuff on the upper arm. The BP monitor was programmed to automatically measure BP at midnight, 2 am, and 4 am. All BP and heart rate (HR) values were recorded in the built-in memory of the device.
The daily sleeping period was defined using an actigraphy device (Actiwatch 2, Philips Respironics, Murrysville, PA, USA). This device can measure physical activity and illuminance using a built-in three-dimensional accelerometer and silicon photodiode, respectively. Well-trained technicians defined the individual’s daily sleeping period using computed actigraphy (Actiware, Philips Respironics) and a self-reported sleep diary. BP values measured during the sleeping period, within 1 h after awakening, and within 1 h before sleeping were considered as sleep, morning, and evening BP, respectively. If there were multiple readings in each slot, the mean value was calculated as a representative value.
Individuals whose evening, sleep, and morning BP values for a given day were available (n = 4780) were included in the final analysis. Home BP monitoring was performed from June to February.
Nocturnal BP dipping
The daily nocturnal BP dipping level was calculated as a percent change of sleep BP to awakening BP (average of morning and evening BPs); [(sleep BP–awake BP)/awake BP] × 100. The nocturnal dipping pattern was defined by the mean of daily nocturnal SBP change as follows: extreme-dipper, nocturnal SBP change ≤−20%; dipper, >−20% to ≤−10%; non-dipper, >−10%; and riser, increase in sleep SBP compared with awakening SBP.
Day-to-day variability
Day-to-day variability of BP values (mmHg) and nocturnal BP dipping (%) were assessed using the coefficient of variation (CV; standard deviation/mean). The CV was calculated for individuals whose home BP readings were available for more than 3 days (n = 3475).
Clinical parameters
Other clinical parameters used in this study were obtained from a personal record of measurements taken at the follow-up investigation. Details regarding alcohol consumption and medical treatment, including antihypertensive drug use and sleep apnea therapy, were obtained using a structured self-reporting questionnaire. Alcohol consumption was calculated by multiplying the amount consumed in a single day and the number of drinking days per week and was described in Japanese traditional units of alcohol (Go), where 1 Go corresponds to 22 g of ethanol.
Temperature data
Daily maximum, minimum, and mean temperatures in Nagahama city were obtained from a database of the Japan Meteorological Agency.
Statistical analysis
Group differences in numeric variables were assessed using analysis of variance, and frequency differences were assessed using the chi-squared test. Multiple linear regression was used to identify factors that were independently associated with nocturnal SBP dipping. Multinomial logistic regression analysis with extreme-dipper as a reference was used to identify factors for dipper, non-dipper, and riser. Reproducibility of that nocturnal BP dipping pattern was assessed using κ statistics, while the intra-individual concordance ratio of the dipping pattern during the latest three nights was assessed using Kendall’s coefficient of concordance.
Statistical analyses were performed using statistical software (JMP ver. 12.2.0; SAS Institute, Cary, NC, USA). Kendall’s coefficient of concordance was calculated using R software and the Kendall command packaged in the irr library. A p-value of <0.05 was considered to be statistically significant.
Results
The clinical characteristics of the study subjects are summarized in Table 1. Sleep BP values were slightly lower than evening and morning BP values, and mean systolic and diastolic BP differences between sleeping and awakening were −10.8 ± 10.5 and −7.5 ± 7.3 mmHg, respectively. Home BP monitoring was performed for 1–7 days by the participants.
Seasonal variation in nocturnal BP changes
The frequencies of extreme-dipper, dipper, non-dipper, and riser patterns were 6.5, 34.7, 45.2, and 13.6%, respectively. Differences in clinical parameters according to dipping pattern are summarized in Table 2. In addition to the awakening BP, serum BNP levels were significantly different by dipping pattern, with higher levels occurring in risers. Although there was an inverse association between BNP levels and eGFR (log-normalized BNP; r = −0.175, p < 0.001), differences in BNP levels by dipping pattern were independent of eGFR (analysis of covariance for log-normalized BNP; dipping pattern: p = 10.0, p < 0.001; eGFR: p = 114.6, p < 0.001, dipping pattern*eGFR interaction: F = 1.4, p = 0.255)
.
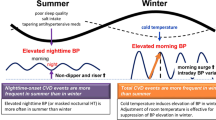
Seasonal variations in various BP parameters related to nocturnal BP change are depicted in Fig. 1. In contrast to morning and evening SBPs that showed lower levels in the summer season, sleep SBP tended to be high in the summer (Fig. 1a). The nocturnal SBP fall was therefore different by season (Fig. 1b), and the seasonal variation was symmetrical to that of the mean temperature of the study site. Similar results were also observed in the sub-analysis according to antihypertensive medication status (Supplementary Figures 1 and 2). The mean nocturnal SBP fall in each season was as follows: summer [July and August], −5.8 ± 7.8%; middle [April–June, September, and October], −8.2 ± 7.5%; winter [November–March], −11.0 ± 7.7%; p < 0.001. When the ambient temperature of a first-measurement day of each participant was compared with the mean nocturnal SBP dipping level individually, the maximum (r = 0.242, p < 0.001), minimum (r = 0.253, p < 0.001), and mean (r = 0.253, p < 0.001) temperature values showed a significant association with nocturnal dipping level. The nocturnal decline of DBP was greater in the winter season: summer, −7.0 ± 9.0%; middle, −9.7 ± 9.0%; winter, −11.9 ± 9.3%; p < 0.001. Figure 1c shows the frequency differences in the dipping pattern. The frequencies of the riser (summer, 19.9; middle, 12.8; winter, 7.8) and non-dipper (summer, 51.4; middle, 46.3; winter, 37.0) patterns were higher in the summer season in contrast to the higher frequency of dippers (summer 26.3; middle, 35.4; winter, 43.1) and extreme-dippers (summer, 2.4; middle, 5.5; winter, 12.1) (p < 0.001) in the winter season.
Seasonal effects on nocturnal BP changes. a The mean SBP in the morning, evening, and during sleeping by month are shown. BP monitoring at home was performed from June to February. The dotted lines are quadratic regression lines (morning SBP, p = 0.027; evening SBP, p = 0.027; sleep SBP, p < 0.001). b The percentage decline in sleep SBP [(sleep SBP−awake SBP) × 100/awake SBP] and mean temperature at Nagahama city during investigation (2013–2015) obtained from a database of the Japan Meteorological Agency are shown. The number of subjects in each subgroup is shown in columns. c Frequency differences in nocturnal dipping patterns; extreme-dipper, nocturnal SBP change ≤−20%; dipper, >−20% to ≤−10%; non-dipper, >−10%; and riser, increase in sleeping SBP compared with awakening SBP
Multivariate analysis for nocturnal BP change
Several characteristics were significantly different among the subgroups according to measurement season (Table 3). The distinct characteristics of the winter-measured subgroup were younger age, lower frequency of antihypertensive treatment, and lower circulating BNP levels, while no substantial group differences were observed in BMI and sex ratio. However, the results of linear regression analysis identified measurement season as a positive determinant for sleep SBP (middle: coefficient = 1.409, β = 0.045, p = 0.003; summer: coefficient = 1.825, β = 0.055, p < 0.001), an inverse determinant for awakening SBP (middle: coefficient = −2.484, β = −0.074, p < 0.001; summer: coefficient = −5.221, β = −0.148, p < 0.001), and consequently, a positive determinant for nocturnal SBP dipping levels (Table 4); these results were independent of the all covariates listed in Table 4. A similar relationship was observed in the analysis for DBP (middle: coefficient = 1.775, β = 0.093, p < 0.001; summer: coefficient = 3.970, β = 0.199, p < 0.001). In a separate analysis by age group, the effect of season on nocturnal SBP dipping (coefficient; ≥65 years: middle = 2.006, summer = 4.319; < 65 years: middle = 2.834, summer = 4.421) and DBP dipping (coefficient; ≥65 years: middle = 1.029, summer = 3.261; <65 years: middle = 2.135, summer = 4.298) were slightly stronger in the younger subgroup.
In the multinomial logistic regression analysis, seasonal effect was identified as an independent determinant for the nocturnal dipping pattern (Table 4), and when the extreme-dipper pattern was considered as a reference, the seasonal effect was greater for the riser pattern, followed by the non-dipper and dipper patterns (Table 4). Although serum BNP levels were also significantly different by season, the seasonal variation in nocturnal BP changes was independent of BNP level.
When sleep duration (Supplementary Table 1) or midpoint of sleep (Supplementary Table 2) was further included in the regression models, the results did not change substantially.
Day-to-day variability of nocturnal BP change
Seasonal differences in day-to-day BP variability (CV) in individuals whose home BP was available for more than 3 days (n = 3475) are shown in Fig. 2. Although the CVs of evening BP and sleep DBP values were lower in the summer season, day-to-day BP variability was not identified as an independent determinant for nocturnal SBP dipping level (evening SBP variability, p = 0.585; sleeping SBP variability, p = 0.973) and DBP dipping level (evening DBP variability, p = 0.071, sleeping DBP variability, p = 0.425) when the variability was additionally included in the regression model for BP dipping level as shown in Table 4. Although reproducibility of the dipping pattern was poor (Supplementary Figure 3), a lack of seasonality in the concordance ratio of the nocturnal dipping pattern (Kendall’s coefficient of concordance; overall, 0.545; winter, 0.527; middle, 0.539; summer, 0.515) suggested less influence of day-to-day BP variability on the seasonal changes in nocturnal BP.
Seasonal differences in day-to-day BP variability. The closed circle and square indicate the mean day-to-day coefficient of variation (CV) of SBP and DBP, respectively. The dotted-line indicates a quadratic regression line (evening BP: SBP, p = 0.402; DBP, p = 0.025; sleeping BP: SBP, p = 0.100; DBP, p = 0.001; morning BP: SBP, p = 0.791, DBP, p = 0.078). The day-to-day CV was calculated in individuals whose home BP was available for more than 3 days (n = 3475). The seasonal effect was assessed by a multiple linear regression analysis using the winter season as a reference. The adjusted factors in this model were age, sex, BMI, alcohol consumption, antihypertensive medication, eGFR, and BNP levels
Discussion
In this large-scale, cross-sectional study involving multiday measured sleep BP, we clarified that there was a marked seasonal variation in nocturnal BP dipping level and consequently higher frequencies of non-dipper and riser patterns in the summer season. The seasonal variation might not be due to seasonal differences in the day-to-day variation in nocturnal BP dipping levels.
The frequencies of riser and non-dipper patterns in the summer season were 2.7 and 1.4 times higher than those in the winter season, respectively. Although these abnormal circadian BP patterns were suggested to be associated with adverse cardiovascular outcomes [1, 2], the large seasonality in the frequency raises a question about whether the prognostic significance of riser and non-dipper patterns in the summer was similar to that observed in the winter. The frequency difference poses a hypothesis that non-dipping and rising patterns in the winter season might be more deleterious. Further, lower awakening BP in the summer may outweigh any risks due to smaller nocturnal BP decline, although no supportive evidence is currently available. This issue deserves further longitudinal study, considering the higher incidence ratio of myocardial infarction [18] and stroke [19] in the winter season.
Although mechanisms underlying the seasonal differences in circadian BP variation are uncertain, the most plausible one for the higher sleep BP in the summer might be a condition of discomfort, namely, a higher night-time temperature and humidity, which contributes to nocturnal BP elevation by worsening sleep quality. We investigated another possibility that the poor reproducibility of the BP measurement, particularly sleep BP, might be involved in the seasonality by capturing an episodic outlier value when a single BP measurement was adopted for the assessment of the nocturnal dipping pattern [13, 14]. However, because the day-to-day variability of the nocturnal BP level did not differ by season, the seasonality might not be due to an increase in the individual’s daily BP variation. As the summer season was associated with both lower awakening BP and higher nighttime BP, the increase in the prevalence of the non-dipping pattern in the summer might not simply be a result of awakening BP decline.
Notably, sodium sensitivity in essential hypertensive patients was suggested to be a factor in the rising of nocturnal BP [20, 21], and facilitation of sodium excretion and diuresis has been suggested as a reason why nocturnal BP levels remained higher in sodium-sensitive hypertensive patients [22, 23]. We also reported an involvement of excessive body fluid retention in the rise of sleep BP by showing an inverse relationship between circulating BNP levels, a marker of increased body fluid retention, and decreased nocturnal BP fall [10]. This inverse association was replicated in the present study in an independent population, suggesting a robustness of the relationship between body fluid retention and circadian BP variation. However, the seasonality in nocturnal BP changes was independent of BNP levels, although BNP level also showed significant seasonal variation, with lower levels in the winter season. The effect of body fluid retention on seasonality might therefore be modest. The association of the seasonal variation of nocturnal BP and BNP levels with heart failure, the incidence of which in the community was reported to be oppositely high in the winter and spring seasons [24], also deserves further investigation.
Sleep apnea is another strong determinant of sleep BP [9]. We reported that increased oxygen desaturation during sleep was an independent determinant of the non-dipping pattern; however, an increase in oxygen desaturation was not a determinant of the rising pattern by a simultaneous measure of ambulatory BP [10]. Because oxygen drop is an episodic event, its effect on nocturnal BP levels might not be strong enough to raise it above awakening BP levels. Given the previous results, as well as the presently observed insignificant association of sleep duration and sleeping period with seasonality in nocturnal BP change, sleep parameters might not be a primary reason for the seasonal variation in nocturnal BP fall. Involvement of the remaining physiological factors, such as insufficient deactivation of sympathetic nervous activity, needs to be investigated to shed light on the mechanism causing seasonality involvement in nocturnal BP fall.
Antihypertensive treatment, particularly the administration time, might influence the circadian BP variation in hypertensive subjects [25, 26] and those with sleep apnea syndrome [27]. A large-scale observational study in hypertensive subjects reported that the number of antihypertensive drugs administered was linearly associated with decreasing nocturnal BP dipping level and increased frequency of the non-dipping pattern [28]. In the present study, however, antihypertensive medication status was not associated with either nocturnal BP fall or a circadian BP pattern; although, based on the body fluid hypothesis, individuals taking diuretics were assumed to have lower nocturnal BP levels. A plausible reason for the discrepancy is a different study setting, namely, a smaller proportion of individuals taking antihypertensive drugs in our study population. The results of our previous study [10] also showed a nonsignificant association between antihypertensive medication status and circadian BP variation in a different general population in which the frequency of antihypertensive drug use was 33.4%.
No marked association was observed between daily alcohol intake and the nocturnal BP pattern, although a previous general population-based study [29] suggested a possibility that moderate (23–45 g alcohol/day) to heavy (≥46 g alcohol/day) drinking might increase morning BP. Similar results were found in another population-based study [30]. Here, since we considered only the amount of alcohol intake as a covariate, more detailed analyses such as a Mendelian randomization analysis using the aldehyde dehydrogenase 2 gene genotype, a rate-controlling enzyme in ethanol metabolism in which an inactive allele is frequent in East Asians, as an instrumental variable may further clarify the possible involvement of alcohol in nocturnal BP variation [31, 32].
Reproducibility of the nocturnal BP dipping pattern was modest. Because we used a multiday measured sleep BP in the seasonal variation analysis, biases of poor reproducibility in the present findings might be kept to a minimum. A lack of seasonal differences in the day-to-day concordance of the nocturnal BP dipping pattern (Kendall’s coefficient) also supports the robustness of the present findings. However, the poor reproducibility of the nocturnal dipping pattern in general should be interpreted with caution when ambulatory monitored BP was used in epidemiological studies. Multiday measurement may be the easiest method to certainly evaluate circadian BP variation.
A strength of this study was the large population size, which enables us to calculate the seasonal variation in nocturnal BP dipping. Another strength is the multiday measurement of nocturnal BP, which was helpful to clarify associations between nocturnal BP changes and various clinical and environmental phenotypes beyond the intra-individual variations in nocturnal BP changes. Instead, to perform multiday BP monitoring, we did not measure 24-h BP using a conventional ambulatory BP monitor. The calculation of the nocturnal BP dipping level, as well as its dipping pattern, was therefore somewhat different from that of previous studies. However, it was recently reported that the simple measured nighttime BP and BP measured using an ambulatory monitor had similar values and a comparable relationship with target-organ damage [33]. As another study limitation, we did not measure intra-individual seasonal variation in nocturnal BP, which remains a possibility of confounding population differences across the measurement seasons. We used actigraphy to determine the sleeping period. In contrast to the studies that determined sleeping period by a self-reported sleep diary, our study has the strength of accurate measurement of sleep BP.
In summary, we found large seasonal variations in nocturnal BP fall and its dipping pattern in a large general population. Careful attention should be given to seasonality in epidemiological studies regarding circadian BP variation. The poor reproducibility of the nocturnal BP dipping pattern should also be cautiously considered.
References
Salles GF, Reboldi G, Fagard RH, Cardoso CR, Pierdomenico SD, Verdecchia P, Eguchi K, Kario K, Hoshide S, Polonia J, de la Sierra A, Hermida RC, Dolan E, O’Brien E, Roush GC, ABC-H Investigators. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the Ambulatory Blood Pressure Collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700.
Tsioufis C, Andrikou I, Thomopoulos C, Syrseloudis D, Stergiou G, Stefanadis C. Increased nighttime blood pressure or nondipping profile for prediction of cardiovascular outcomes. J Hum Hypertens. 2011;25:281–93.
Hermida RC, Ayala DE, Smolensky MH, Fernández JR, Mojón A, Portaluppi F. Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks. Hypertens Res. 2016;39:277–92.
O’Flynn AM, Madden JM, Russell AJ, Curtin RJ, Kearney PM. Isolated nocturnal hypertension and subclinical target organ damage: a systematic review of the literature. Hypertens Res. 2015;38:570–5.
Cai A, Zhong Q, Liu C, Zhou D, Li X, Zhang Y, Feng Y, Zhou Y. Associations of systolic and diastolic blood pressure night-to-day ratios with atherosclerotic cardiovascular diseases. Hypertens Res. 2016;39:874–8.
Smith W, Malan NT, Schutte AE, Schutte R, Mc Mels C, Vilser W, Malan L. Retinal vessel caliber and its relationship with nocturnal blood pressure dipping status: the SABPA study. Hypertens Res. 2016;39:730–6.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–41.
Wolf J, Hering D, Narkiewicz K. Non-dipping pattern of hypertension and obstructive sleep apnea syndrome. Hypertens Res. 2010;33:867–71.
Tabara Y, Igase M, Miki T, Ohyagi Y, Matsuda F, Kohara K, J-SHIPP Study Group. B-type natriuretic peptide is a determinant of the nocturnal increase in blood pressure independently of arterial hypertrophy and hypoxia. J Hypertens. 2016;34:2393–401.
Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, Mancia G. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. J Hypertens. 1998;16:1585–92.
Hanazawa T, Asayama K, Watabe D, Hosaka M, Satoh M, Yasui D, Obara T, Inoue R, Metoki H, Kikuya M, Imai Y, Ohkubo T. Seasonal variation in self-measured home blood pressure among patients on antihypertensive medications: HOMED-BP study. Hypertens Res. 2016; https://doi.org/10.1038/hr.2016.133.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, Giglio A, Bilo G, Caldara G, Lonati L, Orlandini S, Maracchi G, Mancia G, Gensini GF, Parati G. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155–61.
Fedecostante M, Barbatelli P, Guerra F, Espinosa E, Dessì-Fulgheri P, Sarzani R. Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J Hypertens. 2012;30:1392–8.
Minami J, Kawano Y, Ishimitsu T, Yoshimi H, Takishita S. Seasonal variations in office, home and 24 h ambulatory blood pressure in patients with essential hypertension. J Hypertens. 1996;14:1421–5.
Stergiou GS, Myrsilidi A, Kollias A, Destounis A, Roussias L, Kalogeropoulos P. Seasonal variation in meteorological parameters and office, ambulatory and home blood pressure: predicting factors and clinical implications. Hypertens Res. 2015;38: 869–75.
Fujiwara T, Kawamura M, Nakajima J, Adachi T, Hiramori K. Seasonal differences in diurnal blood pressure of hypertensive patients living in a stable environmental temperature. J Hypertens. 1995;13:1747–52.
van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG. Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol. 2001;30:1109–16.
Shinkawa A, Ueda K, Hasuo Y, Kiyohara Y, Fujishima M. Seasonal variation in stroke incidence in Hisayama, Japan. Stroke. 1990;21:1262–7.
Uzu T, Kazembe FS, Ishikawa K, Nakamura S, Inenaga T, Kimura G. High sodium sensitivity implicates nocturnal hypertension in essential hypertension. Hypertension. 1996;28:139–42.
Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997;96:1859–62.
Uzu T, Kimura G. Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1999;100:1635–8.
Fujii T, Uzu T, Nishimura M, Takeji M, Kuroda S, Nakamura S, Inenaga T, Kimura G. Circadian rhythm of natriuresis is disturbed in nondipper type of essential hypertension. Am J Kidney Dis. 1999;33:29–35.
Ogawa M, Tanaka F, Onoda T, Ohsawa M, Itai K, Sakai T, Okayama A, Nakamura M, Northern Iwate Heart Disease Registry Consortium. A community based epidemiological and clinical study of hospitalization of patients with congestive heart failure in Northern Iwate, Japan. Circ J. 2007;71:455–9.
Takeda A, Toda T, Fujii T, Matsui N. Bedtime administration of long-acting antihypertensive drugs restores normal nocturnal blood pressure fall in nondippers with essential hypertension. Clin Exp Nephrol. 2009;13:467–72.
Minutolo R, Gabbai FB, Borrelli S, Scigliano R, Trucillo P, Baldanza D, Laurino S, Mascia S, Conte G, De Nicola L. Changing the timing of antihypertensive therapy to reduce nocturnal blood pressure in CKD: an 8-week uncontrolled trial. Am J Kidney Dis. 2007;50:908–17.
Kario K, Kuwabara M, Hoshide S, Nagai M, Shimpo M. Effects of nighttime single-dose administration of vasodilating vs sympatholytic antihypertensive agents on sleep blood pressure in hypertensive patients with sleep apnea syndrome. J Clin Hypertens. 2014;16:459–66.
de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, de la Cruz JJ, Sobrino J, Llisterri JL, Alonso J, Vinyoles E, Pallarés V, Sarría A, Aranda P, Ruilope LM, Spanish Society of Hypertension Ambulatory Blood Pressure Monitoring Registry Investigators. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–72.
Ohira T, Tanigawa T, Tabata M, Imano H, Kitamura A, Kiyama M, Sato S, Okamura T, Cui R, Koike KA, Shimamoto T, Iso H. Effects of habitual alcohol intake on ambulatory blood pressure, heart rate, and its variability among Japanese men. Hypertension. 2009;53:13–19.
Nakashita M, Ohkubo T, Hara A, Metoki H, Kikuya M, Hirose T, Tsubota-Utsugi M, Asayama K, Inoue R, Kanno A, Obara T, Hoshi H, Totsune K, Satoh H, Imai Y. Influence of alcohol intake on circadian blood pressure variation in Japanese men: the Ohasama study. Am J Hypertens. 2009;22:1171–6.
Tabara Y, Arai H, Hirao Y, Takahashi Y, Setoh K, Kawaguchi T, Kosugi S, Ito Y, Nakayama T, Matsuda F, Nagahama study group. The causal effects of alcohol on lipoprotein subfraction and triglyceride levels using a Mendelian randomization analysis: The Nagahama study. Atherosclerosis. 2016;257:22–28.
Tabara Y, Ueshima H, Takashima N, Hisamatsu T, Fujiyoshi A, Zaid M, Sumi M, Kohara K, Miki T, Miura K, SESSA Research Group.; J-SHIPP Study Group. Mendelian randomization analysis in three Japanese populations supports a causal role of alcohol consumption in lowering low-density lipid cholesterol levels and particle numbers. Atherosclerosis. 2016;254:242–8.
Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens. 2017;35:442–52.
Acknowledgements
We are extremely grateful to the Nagahama City Office and non-profit organization Zeroji Club for their help in performing the Nagahama study. We also thank the editors of Crimson Interactive Pvt. Ltd. for their help in the preparation of this manuscript.
Funding
The present study was supported by a university grant, The Center of Innovation Program, The Global University Project, a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science & Technology in Japan, the Practical Research Project for Rare/Intractable Diseases, the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D from the Japan Agency for Medical Research and Development (AMED), and a research grant from the Takeda Science Foundation. The Department of Respiratory Care and Sleep Control Medicine is funded by endowments from Philips-Respironics, Teijin Pharma, Fukuda Denshi, and Fukuda Lifetec-Keiji to Kyoto University.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
APPENDIX
APPENDIX
The Nagahama study group executive committee is composed of the following individuals: Yasuharu Tabara, Takahisa Kawaguchi, Kazuya Setoh, Yoshimitsu Takahashi, Shinji Kosugi, Takeo Nakayama, and Fumihiko Matsuda from the Center for Genomic Medicine, Kyoto University Graduate School of Medicine (Ya T, T K, K S, F M), the Department of Health Informatics (Yo T, T N), the Department of Medical Ethics and Medical Genetics (S K), and Kyoto University School of Public Health.
Rights and permissions
About this article
Cite this article
Tabara, Y., Matsumoto, T., Murase, K. et al. Seasonal variation in nocturnal home blood pressure fall: the Nagahama study. Hypertens Res 41, 198–208 (2018). https://doi.org/10.1038/s41440-017-0003-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-017-0003-3
This article is cited by
-
Seasonal variation in blood pressure and its impact on target organ damage and cardiovascular disease incidence
Hypertension Research (2023)
-
The Association Between Season and Hypertensive Disorders in Pregnancy: a Systematic Review and Meta-analysis
Reproductive Sciences (2023)
-
The relationship between home blood pressure measurement and room temperature in a Japanese general population
Hypertension Research (2021)
-
Nighttime home blood pressure as a mediator of N-terminal pro-brain natriuretic peptide in cardiovascular events
Hypertension Research (2021)
-
Seasonal variation in blood pressure: current evidence and recommendations for hypertension management
Hypertension Research (2021)