Abstract
Multiple bone disorders due to mutations in the human noggin (NOG) causes a variety of phenotypes. Hearing impairment due to stapes ankylosis secondary to bony degeneration is also a feature of these syndromes. We describe the case of an individual in a Japanese family with conductive hearing loss due to stapes ankylosis and hyperopia and dactylosymphysis. We revealed a novel NOG mutation, NM_005450.6:c.222 C > A / p.Tyr74*, and confirmed genetic significance.
Similar content being viewed by others
Stapes ankylosis is characterized by hearing loss due to congenital or acquired stapes fixation. While otosclerosis is the most common progressive conductive hearing loss caused by stapes ankylosis in adults, congenital stapes ankylosis is often difficult to differentiate from otosclerosis if diagnosed later in life. Congenital stapes ankylosis seems to be associated with osteodysplasty, such as osteogenesis imperfecta type I. It may occur as an isolated temporal bone anomaly, such as X-linked stapes fixation with perilymphatic gusher (DFN3)1. Additionally, some families reportedly have an autosomal-dominant form of congenital stapes ankylosis1,2,3. They describe clinical manifestations and corresponding bone abnormalities, including multiple synostosis, proximal symphalangism, and facial abnormalities. They also list several corresponding NOG gene mutations identified for these genealogy changes. Noggin is a secreted protein encoded by NOG that is essential for normal bone and joint formation in both humans and mice4, and appears to play a regulatory role as a bone morphogenetic protein (BMP) antagonist during joint formation. Mutations in NOG are in multiple autosomal-dominant syndromes that often share symptoms, such as conductive hearing loss, hyperopia, and digital anomalies5,6. These include stapes ankylosis syndromes such as proximal symphalangism (SYM1, OMIM 185800), multiple-synostoses syndrome (SYNS1, OMIM 186500), stapes ankylosis with broad thumbs and toes (SABTT, OMIM184460), tarsal-carpal coalition syndrome (TCC, OMIM 186570), and brachydactyly type B2 (BDB2, OMIM 611377). Currently, similarities and variations in overlapping features have led to the categorization of all these syndromes as NOG-related symphalangism spectrum disorder (NOG-SSD). Here, we describe the pedigree of a Japanese family with inherited stapes ankylosis, hyperopia, and digital anomalies, and show that a novel heterozygous NOG mutation results in NOG-SSD.
The proband (Case B: III-3) was a 27-year-old woman referred to our hospital due to bilateral hearing loss. She was not administered a newborn hearing screening test but seemed to have been aware of her hearing disability since early childhood and continued to suffer in her job due to hearing difficulties. Pure tone audiometry showed a bilateral conductive hearing loss, especially in the low pitch area. Although tympanometry yielded a type A curve, a stapedial reflex test indicated no response in either ear. A High-resolution computed tomography scan showed no ossicular malformation or inner ear abnormalities.
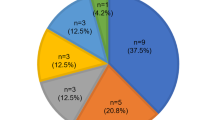
Her medical history and pedigree, including hearing loss, symphalangism, dactylosymphysis, brachydactyly, and hyperopia, were evaluated before surgery. Fig. 1 shows the pedigree of this family, which had five affected individuals. Physical findings and X-ray evaluation of her hands showed symphalangism and short, intermediate phalanges (brachydactyly) in two fingers (Fig. 2a, b, c). The range of motion in her elbow joint was restricted, and she could not touch her shoulders with her hands (Fig. 2d). An ophthalmologic examination revealed hyperopia. Two of her elder brothers (III-1 and III-2) also suffered from hearing loss, hyperopia, dactylosymphysis.
a Family Pedigree. Square symbols denote male patients, and circles denote female patients. Blackened symbols denote affected individuals, and white symbols denote unaffected individuals. b Sanger sequencing chromatogram. Sanger DNA sequencing chromatogram demonstrates heterozygosity for a NOG variant (c.222 C > A / p.Tyr74*) in proband (III-3) and her mother (II-2).
Phenotypic characteristics of the patient. a Photographs and b X-ray imaging of the hands of the proband. Circles indicate symphalangism, and arrowheads indicate brachydactyly. c, d Photograph illustrating a restricted range of elbow joint motion in affected individuals and their inability to touch their shoulders with their hands.
Blood samples were obtained from the proband (caseB: III-3) and her mother (caseA:II-2), and DNA was extracted from peripheral lymphocytes using the PAXgene Blood DNA kit (Qiagen#761133, Valencia, USA). As pedigree and clinical features were suggestive of mutations in NOG, we analyzed the NOG-coding region in each case by sequencing genomic DNA. Primer pairs were designed to include the entire protein-coding region consisting of 698 nucleotides, and the NOG-coding region was amplified by polymerase chain reaction using the following primers pairs: NOG (forward), 5'-CTCGGCGTGCTCTCCTC-3'; NOG (reverse), 5' - ATCGATCAAGTGTCCGGGTG-3'. DNA sequencing was performed using the standard protocol of the Applied Biosystems 3130 l gene sequence analyzer (Applied Biosystems, Nieuwerkerk aan de IJssel, The Netherlands). Study participants provided written informed consent. The Ethical Review Committee of the Hiroshima University, Japan, approved the research protocol.
Due to significant conductive hearing loss, we performed surgery on her left ear using an endoscope, which revealed ankylosis of the stapes footplate; hence, we performed a stapedotomy. The patient’s hearing threshold improved significantly, and her hearing level has remained stable for >1.5 years after surgery.
Genetic analysis identified a heterozygous c.222 C > A/p.Tyr74* mutation in NOG in the proband (Case B) and in her mother (Case A) (Fig. 1b), which has not been previously reported or cataloged in either the HGMD or other databases such as ClinVar. Given that other nonsense mutations such as p.Gln110* and p. Leu129* have been reported to be pathognomic, we hypothesize that this produces a truncated noggin protein that disrupts protein function.
The human NOG gene is present on chromosome 17q22, has one exon, and codes a secreted protein, Noggin, that seems to be involved in BMP signaling as an antagonist essential for bone formation in both humans and mice4,7,8. BMP promotes mesenchymal cell proliferation and differentiation into chondroblasts and osteoblasts and induces apoptosis during joint formation9.
NOG mutations have been previously described in the context of multiple bone diseases10, e.g., the typical features of SYM1 are narrow proximal interphalangeal joint space and symphalangism of the 4th and/or 5th fingers11,12. SYM1 is characterized by an autosomal-dominant heritability with minimal genetic heterogeneity, and mutations in NOG are thought to be predominantly responsible for SYM1; nevertheless, other genes such as GDF5 have also been implicated13. Thus, even though our patient presented with conductive hearing loss, a proximal phalangeal fusion of the fingers, and limited range of motion in the shoulder, we considered it reasonable to clinically diagnose her with SYM1 despite the absence of other systemic skeletal abnormalities or ocular symptoms. Additionally, a variety of syndromes, such as SYNS1, TCC, BDB2, SABTT, have been attributed to heterozygous NOG, and are described as subtypes of SSD.
Notably, the same variant of NOG can result in dissimilar phenotypes among different families or various affected members of the same family14,15. Gong et al. reported that the key features differentiating SYM1 from SYNS1 are characteristic physiognomy, hyperopia, and the absence of cervical vertebral fusion and symphalangism16,17. Similarly, it is hard to accurately categorize such patients as having a particular disease because, to date, >50 mutations in NOG are reportedly involved in a wide variety of bone development anomalies, as listed by Yuan et al7. Congruently, previous case reports confirm that mutations in the same NOG-coding sequence can lead to various phenotypes within one family18,19,20,21,indicating that disease expression may correlate to either location or type of NOG mutation.
We describe the pedigree of a Japanese family with SSD, and analysis of the genetic changes in the proband and her mother revealed a novel NOG c.222 C > A/p.Tyr74*. This mutation site is present between c.163 G > T/p.Asp55Tyr and c.328 C > T/p.Gln110*, which, according to Yuan et al.7, are pathognomic for SYM1 and FOP, respectively. Further, as these two mutations reportedly result in a termination codon and consequent degeneration of the noggin protein, a codon in this specific region is expected to be crucial for BMP7 binding; hence, its loss can affect joint morphogenesis. Congruently, evaluation of the pathogenicity of this mutation in “MutationTaster” and “Provean” confirmed its significance, as the results were “Prediction disease causing” and “Deteleous,” respectively. Thus, and under ACMG guidelines, we posit that the c.222 C > A mutation causes a meaningful change in NOG that is pathogenic (PVS1, PM2, PM3, and PP4).
The occurrence of bilateral congenital stapes ankylosis without other anomalies is rare, and it is sometimes not found in mild hearing loss. Further, congenital stapes ankylosis syndrome is difficult to distinguish from otosclerosis when first identified in adults. Thus, as some patients diagnosed with sporadic or non-syndromic familial otosclerosis may indeed have SSD, those with conductive hearing loss should be evaluated for other osseous lesions. The degree of hearing impairment in SSD is different from those described previously, i.e., mild to profound, possibly due to disease progression. Thus, attention must be paid to patients with suspected bilateral conductive hearing loss due to mutations in NOG. Unlike the NOG mutation reported in SYM 1 and SYNS1, family lineages with stapes ankylosis but no other fusions presumably have a protein with a dysfunctional terminal domain otherwise abundant in cysteine (C). Some pathogenic differences due to cysteine may exist among patients without osseous abnormality.
We identified a novel NOG mutation in a Japanese family, which helped clarify the relationship between phalangeal fusion disease and conductive hearing loss. Apart from genetic counseling, we could also provide beneficial information about progressive hearing loss, which would help affected siblings as they could recover hearing after surgery. Thus, managing patients presenting with bilateral conductive hearing loss requires careful physical evaluation of osteodystrophy based on both past and family medical histories.
Change history
15 November 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41439-023-00249-6
References
Brown, D. J. et al. Autosomal dominant stapes ankylosis with broad thumbs and toes, hyperopia, and skeletal anomalies is caused by heterozygous nonsense and frameshift mutations in NOG, the gene encoding noggin. Am. J. Hum. Genet. 71, 618–624 (2002).
Takano, K. et al. A novel nonsense mutation in the NOG gene causes familial NOG-related symphalangism spectrum disorder. Hum. Genome Var. 3, 16023 (2016).
Ishino, T., Takeno, S. & Hirakawa, K. Novel NOG mutation in Japanese patients with stapes ankylosis with broad thumbs and toes. Eur. J. Med Genet. 58, 427–432 (2015).
Zimmerman, L. B., De Jesus-Escobar, J. M. & Harland, R. M. The Spemann organizer signal noggin binds and inactivates bone morphogenetic protein 4. Cell 86, 599–606 (1996).
Takahashi, T. et al. Mutations of the NOG gene in individuals with proximal symphalangism and multiple synostosis syndrome. Clin. Genet 60, 447–451 (2001).
Mangino, M., Flex, E., Digilio, M. C., Giannotti, A. & Dallapiccola, B. Identification of a novel NOG gene mutation (P35S) in an Italian family with symphalangism. Hum. Mutat. 19, 308 (2002).
Yuan, Z. Z. et al. Identification of an unknown frameshift variant of NOG in a Han Chinese family with proximal symphalangism. Biosci. Rep. 40, BSR20200509 (2020).
Bernatik, O. et al. A novel role for the BMP antagonist noggin in sensitizing cells to non-canonical Wnt-5a/Ror2/disheveled pathway activation. Front Cell Dev. Biol. 5, 47 (2017).
Hashimi, S. M. Exogenous noggin binds the BMP-2 receptor and induces alkaline phosphatase activity in osteoblasts. J. Cell Biochem. 120, 13237–13242 (2019).
Khan, S., Mudassir, M., Khan, N. & Marwat, A. Brachdactyly instigated as a result of mutation in GDF5 and NOG genes in Pakistani population. Pak. J. Med Sci. 34, 82–87 (2018).
Xiong, J. et al. Identification of a novel NOG Missense mutation in a Chinese family with symphalangism and tarsal coalitions. Front Genet. 10, 353 (2019).
Sha, Y. et al. Novel NOG (p.P42S) mutation causes proximal symphalangism in a four-generation Chinese family. BMC Med. Genet. 20, 133 (2019).
Wang, X., Xiao, F. & Yan, Q. A novel mutation in GDF5 causes autosomal dominant symphalangism in two Chinese families. Am. J. Med Genet A. 140A, 1846–1853 (2006).
Lehmann, K. et al. A new subtype of brachydactyly type B caused by point mutations in the bone morphogenetic protein antagonist NOGGIN. Am. J. Hum. Genet. 81, 388–396 (2007).
Liu, F., Huang, Y., Liu, L, Liang, B., Qu, Z., Huang, G. et al. Identification of a novel NOG mutation in a Chinese family with proximal symphalangism. Clin Chim Acta. 429, 129–133 (2014).
Gong, Y., Krakow, D. & Marcelino, J. Heterozygous mutations in the gene encoding noggin affect human joint morphogenesis. Nat. Genet. 21, 302–304 (1999).
Vesell, E. S. Symphalangism, strabismus and hearing loss in mother and daughter. N Engl J Med. 263, 839–842 (1960).
Takahashi, T. et al. Mutations of the NOG gene in individuals with proximal symphalangism and multiple synostosis syndrome. Clin. Genet. 60, 447–451 (2001).
Pang, X. et al. A novel missense mutation of NOG interferes with the dimerization of NOG and causes proximal symphalangism syndrome in a Chinese family. Ann. Otol. Rhinol. Laryngol. 124, 745–751 (2015).
Athanasakis, E., Biarnés, X., Bonati, M. T., Gasparini, P. & Faletra, F. Identification of a new mutation (L4 6P) in the human NOG gene in an Italian patient with symphalangism syndrome. Mol. Syndromol. 3, 21–24 (2012).
Ganaha, A. et al. Identification of two novel mutations in the NOG gene associated with congenital stapes ankylosis and symphalangism. J. Hum. Genet. 60, 27–34 (2015).
Acknowledgements
We thank Yukako Okamoto who helped us in analyzing the genetic confirmation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sonoyama, T., Ishino, T., Ogawa, Y. et al. Identification of a novel nonsense NOG mutation in a patient with stapes ankylosis and symphalangism spectrum disorder. Hum Genome Var 10, 12 (2023). https://doi.org/10.1038/s41439-023-00236-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41439-023-00236-x